More Information
Submitted: January 09, 2025 | Approved: January 15, 2025 | Published: January 16, 2025
How to cite this article: Herrera AS, Esparza MA, Shuckov S. The Fundamental Role of Dissolved Oxygen Levels in Drinking Water, in the Etiopathogenesis, Prevention, Treatment and Recovery of Cerebral Vascular Events (Stroke). J Nov Physiother Rehabil. 2025; 9(1): 001-006. Available from:
https://dx.doi.org/10.29328/journal.jnpr.1001064
DOI: 10.29328/journal.jnpr.1001064
Copyright License: © 2025 Herrera AS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Blood vessels; Brain vasculature; CSF; Oxygen; Stroke; Vascular cerebral events; Water dissociation
The Fundamental Role of Dissolved Oxygen Levels in Drinking Water, in the Etiopathogenesis, Prevention, Treatment and Recovery of Cerebral Vascular Events (Stroke)
Arturo Solís Herrera*, María del Carmen Arias Esparza and Sergey Shuckov
Human Photosynthesis™ Study Center, Aguascalientes 20000, México
*Address for Correspondence: Arturo Solís Herrera, MD, PhD, Human Photosynthesis™ Study Center, Aguascalientes 20000, México, Email: [email protected]
Stroke is a clinically defined syndrome of acute focal neurological deficit attributed to vascular injury (infarction, hemorrhage) of the central nervous system. Stroke is the second leading cause of death and disability worldwide. Stroke is not a single disease but can be caused by a wide range of risk factors, disease processes and mechanisms. Approximately 15% of strokes worldwide are the result of intracerebral hemorrhage, which can be deep (basal ganglia, brainstem), cerebellar or lobar. A minority (about 20%) of intracerebral hemorrhages are caused by macrovascular lesions (vascular malformations, aneurysms, cavernomas), venous sinus thrombosis or rarer causes.
The prevalence of stroke is highest in developing countries, with ischemic stroke being the most common type. Stroke therapy primarily focuses on restoring blood flow to the brain and treating stroke-induced neurological damage. Lack of success in recent clinical trials has led to significant refinement of animal models, focus-driven study design and use of new technologies in stroke research.
Stroke is a neurological disorder characterized by blockage of blood vessels. Clots form in the brain and interrupt blood flow, clogging arteries and causing blood vessels to break, leading to bleeding. Rupture of the arteries leading to the brain during stroke results in the sudden death of brain cells owing to a lack of oxygen. Stroke can also lead to depression and Dementia [1].
Stroke is the second leading cause of death globally. It affects roughly 13.7 million people and kills around 5.5 million annually. Approximately 87% of strokes are ischemic infarctions, a prevalence which increased substantially between 1990 and 2016, attributed to decreased mortality and improved clinical interventions.
The incidence of stroke increases with age, doubling after the age of 55 years. However, in an alarming trend, strokes in people aged 20–54 years increased from 12.9% to 18.6% of all cases globally between 1990 and 2016 [2].
The highest reported stroke incidence is in China, where it affects an estimated 331–378 individuals per 100,000 life years. The second-highest rate is in eastern Europe (181–218 per 100,000 life years) and the lowest in Latin America (85–100 per 100,000 life years) [3].
Both brain infarction and intracerebral hemorrhage (ICH) are common in men, but cardioembolic stroke, a more severe form of stroke, is more prevalent among women. The fatality rate for stroke is also higher among women [4].
A global population-based study of the prevalence of stroke and related risks examined demography, behavior, physical characteristics, medical history and laboratory reports, and revealed the contribution of exposure to air pollution and particulate matter to stroke mortality [5].
The annual number of strokes and deaths due to stroke increased substantially from 1990 to 2019, despite substantial reductions in age-standardised rates, particularly among people older than 70 years. The highest age-standardised stroke-related mortality and DALY rates were in the World Bank low-income group. The fastest-growing risk factor for stroke between 1990 and 2019 was high body-mass index. Without urgent implementation of effective primary prevention strategies, the stroke burden will probably continue to grow across the world, particularly in low-income countries [6].
Where survivors of stroke live may make a difference in their clinical outcomes, including long-term mortality. A large body of supportive evidence from epidemiologic studies has demonstrated that geographic difference in stroke mortality is non-artifactual, although both its presence and magnitude are likely scale-dependent at different population levels [7].
Since at least 1940s there has been a consistent pattern of market geographic variation in stroke mortality within the U.S., with very high rates reported in the southeast Atlantic coastal plain and very low rates in the Mountain census division [8]. By the mid-1990s, despite minor geographic shifts, such regional differences in stroke mortality had persisted for more than half a century, yet the underlying causes of geographic disparities remained elusive [9].
The persistence of the pattern over more than five decades; the similarity of the pattern for different age, race, and sex groups; the fact that the pattern is not delimited by county, state, or other political administrative boundaries; and the extreme magnitude of the differences between rates in high- and low-rate areas suggest that the geographic pattern of stroke mortality rates is not an artifact of different diagnostic and reporting practices [10].
Regional variation in stroke risk factors (eg, prevalence of hypertension, diabetes, and cigarette smoking) has been documented by various US government health surveys, but none of the factors have been clearly related to the pattern of geographic variation in stroke morbidity and mortality [1]. Systematic attempts to investigate the geographic variation in stroke risk factors as an explanation of the geographic variation in stroke frequency have been few and the results inconsistent [11]. Recognized stroke risk factors, including hypertension, apparently account for only a small fraction of the spatial variation in stroke mortality [12].
Although hypertension is strongly associated with both atherothrombotic brain infarction and intraparenchymal hemorrhage [13], geographic variation in hypertension prevalence does not appear to account for the large variation in stroke occurrence and mortality. Only about 10% of Mormons are regular smokers compared with approximately 40% for the non-Mormon white population of Utah and 35% for the general US population. Significantly, stroke mortality rates are low in both Mormons and non-Mormons in Utah [14], presumably implicating some other protective factor.
The first use of the “stroke belt” concept is now obscure, but the term was applied in the 1970s after the gradual recognition during the 1960s of the existence of a broad area of excess stroke mortality in the southeastern United States [15]. Studies of the geographic distribution of stroke mortality in the United States had been conducted earlier, in fact as early as the late 1940s, but these studies downplayed the evident spatial variation in stroke mortality, especially in comparison with the apparently larger spatial variation in cardiovascular mortality [16].
The National Heart, Lung, and Blood Institute (NHLBI) stroke belt therefore includes Alabama, Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North and South Carolina, Tennessee, and Virginia. In contrast, Howard and colleagues [17] define the stroke belt somewhat arbitrarily as a group of contiguous counties along the coastal plains of Georgia and the Carolinas, since is roughly consistent with some of the area of extreme rates among whites in corresponding state economic areas [18].
The role of dissolved oxygen levels in water in the etiopathogenesis of stroke
As a result of our observation that our body does not take oxygen from the air that surrounds us, but from the water contained inside the cells that make us up, through molecules derived from protoporphyrin IX and melanin [19], we began to correlate dissolved oxygen levels in drinking water, as well as the source of it, with various epidemiologically important diseases [20].
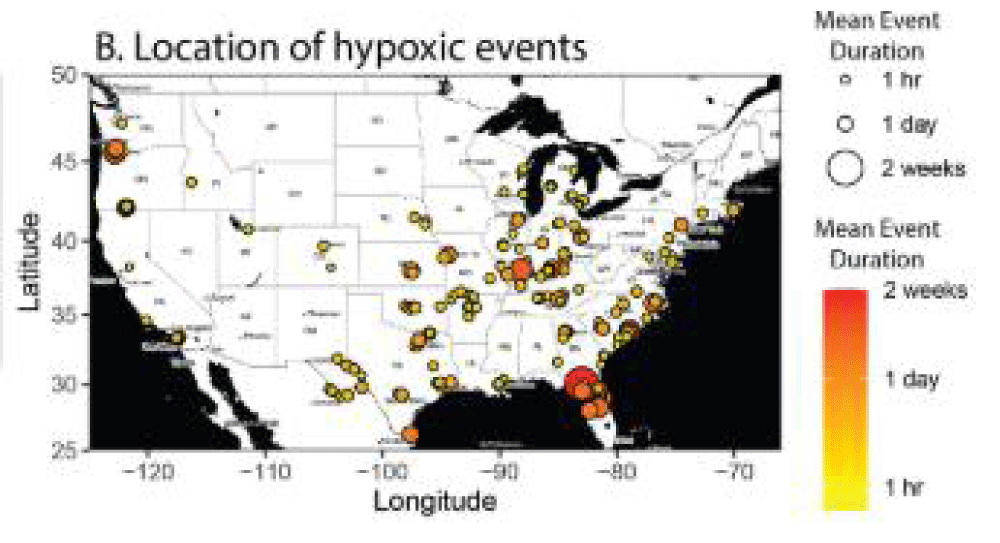
And since our body obtains oxygen from water localized intracellularly, dissociating the molecule; as in plants, the results correlated in a surprising way. That is: the lower the levels of dissolved oxygen in drinking water, as well as the sources of it, since the usual purification does not raise these levels, we have a higher incidence and prevalence of Stroke, and other diseases (Figure 1).
Figure 1: Map of the mean duration of hypoxic events within a river reach defined as [DO] < 2 mg L−1 for locations within the same dataset as panel a. points are colored and sized by event duration [21].
The explanation is that as long as the oxygen levels inside the cell are within the relatively narrow parameters that cells require to maintain their shape and function, then the human body will function fine, but when the levels of dissolved oxygen in the water that is in contact with us (for bathing, for cooking, for washing dishes, for washing clothes, for cleaning houses, for watering the garden, etc.) Not only the one we ingest has levels below 6 milligrams per liter, but the intracellular mechanisms also that dissociate water molecules cannot do so with the speed and accuracy that the biochemical logic of life requires, so imbalances begin to occur in processes that are too exact, which manifests itself in various ways. different in each person; as is the case with Stroke, but it can be thought that as long as intracellular oxygen, which comes from water inside cells and not from the atmosphere, is in balance with the demanding needs of the complex biochemical processes that together lead to life, the entire organism will function well because it is very well made.
Therefore, it can be said that any disease has to start with oxygen imbalance, at the intracellular level. As long as these levels, which are essential for preserving the shape and function of cells, tissues, organs and systems, are in balance, the body will be fine, because they are very resilient processes. But decreased levels of dissolved oxygen reflect the water pollution, and the astonishingly accurate mechanisms of dissociation from the water that cells use for this purpose, and which have been the same since the beginning of time, since they together make up the origin of life, they cannot carry out this dissociation in the way as perfect as is required by intracellular metabolism, and imbalances ensue, which can reach clinical manifestations of various kinds, because each organism is unbalanced in its own way.
The name of the disease does not matter, as the body does not pay attention to it, but we can infer that any disease begins with the imbalance of oxygen at the intracellular level.
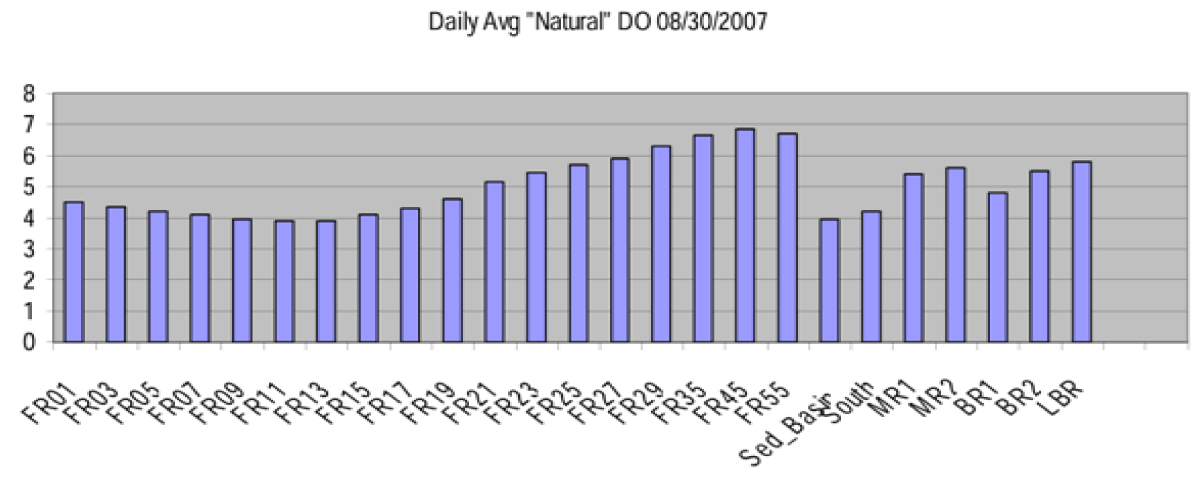
So, returning to the subject of the Stroke belt, described since the middle of the last century, it has a factor in common, and that is the low or very low levels of oxygen dissolved in the water that is in contact with the population (Figure 2).
Figure 2: Daily average DO (dissolved oxygen) by zones [22].
The dissolved oxygen (DO) concentration in a river is an essential indicator of ecosystem assessment. DO decreases in rivers impact biological activities and result in reductions in biodiversity, Humans included.
Therefore, the data cited in previous paragraphs about China occupying the first place in incidence and prevalence of Stroke, is not surprising given that values of even less than 2 mg/L of dissolved oxygen are frequently reported in that region [21].
An area off the Yangtze River Estuary (YRE), China, annually develops one of the world ocean’s largest hypoxic areas. Observations collected by ship since 1999, and by long-term sensors since 2009, show that DO concentration in this region has been both declining and greatly fluctuating [22].
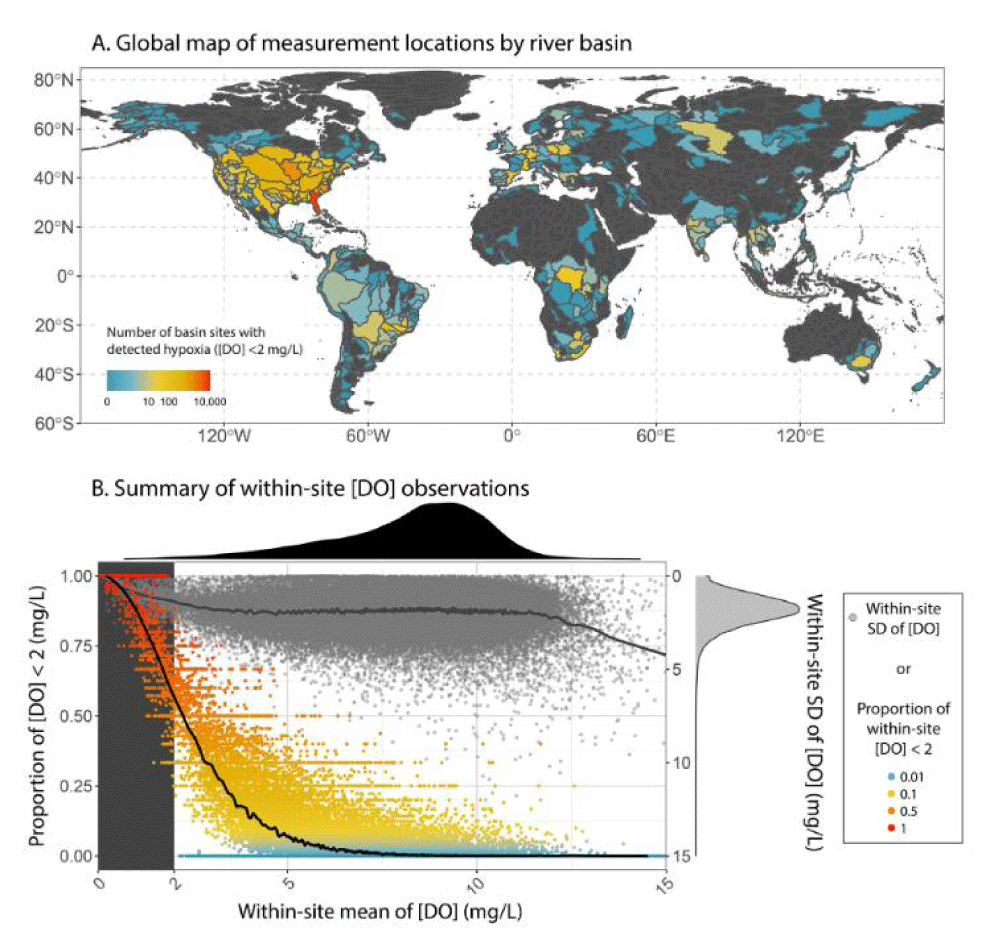
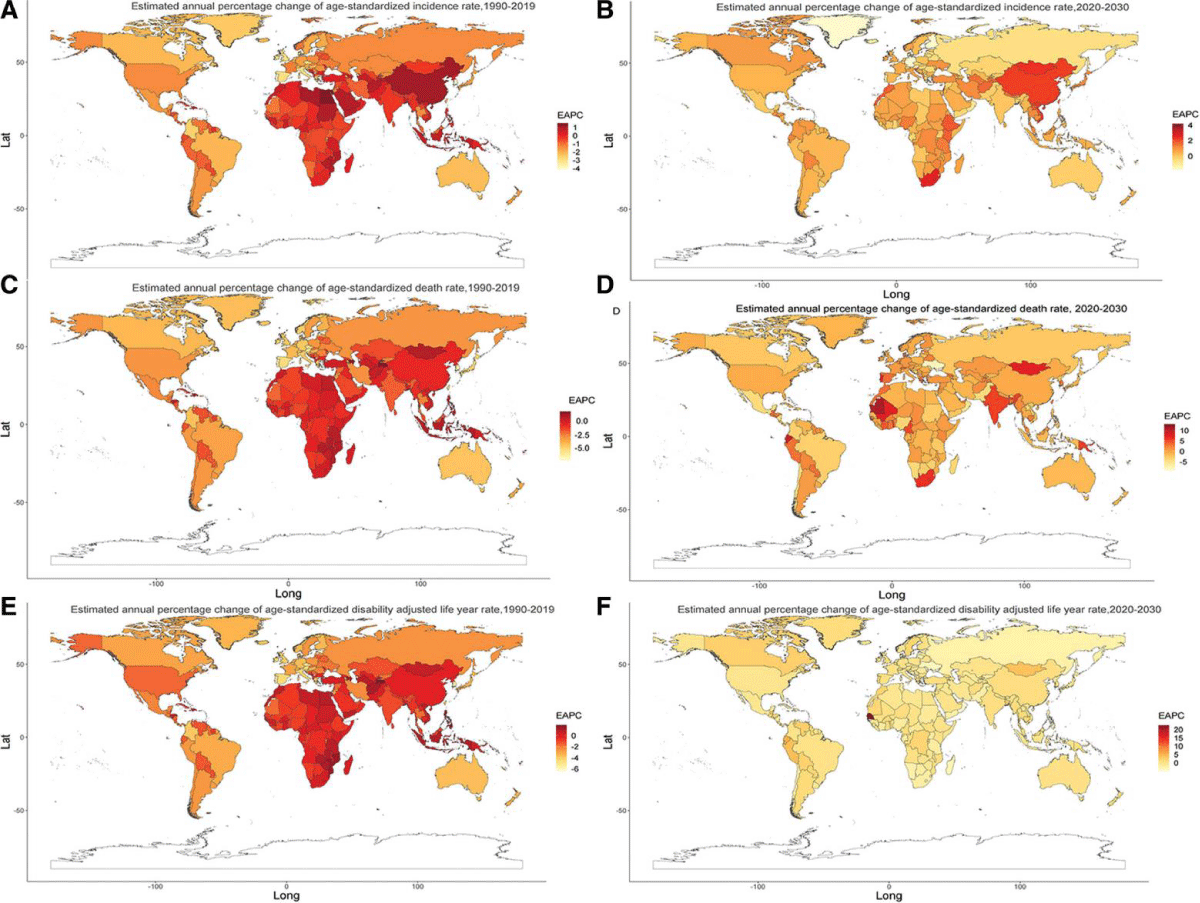
The deoxygenation of water is a growing worldwide challenge (Figure 3). And the growing incidence and prevalence of stroke it’s a consequence (Figure 4).
Figure 3: There is a widespread, short-term occurrence of hypoxia in rivers across the globe, with rivers draining both disturbed and undisturbed landscapes vulnerable to hypoxia. Despite being generally ephemeral, hypoxic conditions in rivers are of outsized relevance because of detrimental effects on aquatic organisms and implications for greenhouse gas emissions [25].
Figure 4: The projections indicated that the incidence rate of ischemic stroke will increase both sexes, all age groups, resulting in neurological death and long-term adult disability and thus imposes massive health and economic burdens [26].
During the last two decades, epidemiological studies conducted worldwide have shown a consistent, increased risk for cardiovascular events [23]. These include heart disease and stroke deaths, in relation to short-term and long-term exposures to present-day concentrations of ambient air pollution, especially particulate matter (PM). Several reports showing excessive mortality associated unexpectedly with low PM concentrations. Recent meta-analyses confirmed that short-term exposure to ambient ozone increases cardiovascular mortality [24].
Short-term elevations of PM and ozone can increase ischemic stroke mortality [25], hospitalizations and emergency visits [26]. Beyond these acute effects, large cohort studies have consistently shown that long-term exposure to air pollution is associated with increased cardiovascular mortality [27]; PM exposure also increases the risks for coronary heart diseases and stroke.
Thereby, exposure to ambient air pollutants can induce excessive oxidative stress, provoke inflammatory responses, perturb endothelial function, damage microvasculature, and cause progression of atherosclerosis [28], although the underlying mechanisms are unclear. The cause of specific mortality associated with air pollution is not investigated easily, due to complex and poorly understood interactions between pollutants and cells and tissues.
However, the interplay between dissolved oxygen levels in the drinking water or those that are in contact with the population, and the etiopathogenesis, prevention, and treatment of cerebral vascular events have not been explored. Probably because the impact of the increasing decline in dissolved oxygen levels on human health was not given due importance.
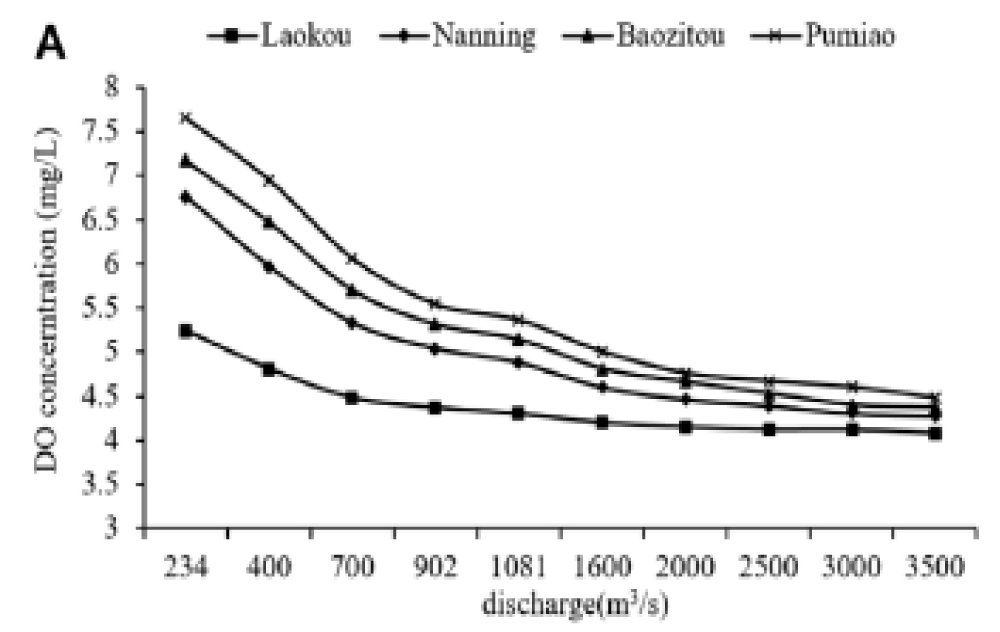
The frenetic anthropogenic activity is a determining factor in the levels of dissolved oxygen in the different types of water that are in contact with human beings and in general with living beings (Figure 5), as it affects the delicate balance between cells and oxygen that we now know comes from the interior of cells, through the dissociation of water. As in plants, and not in the atmosphere, as maintained by the prevailing dogma proposed by Lavoisier and Priestley, in 1750.
Figure 5: Effects of Discharge Flow on River DO. Anthropogenic activities use water, which is polluted in multiple ways and then discharged into rivers, streams, lakes, lagoons, oceans and seas; which have been dumps since the beginning of time. The greater the number of discharges, the lower the dissolved oxygen values, since almost anything that falls into the water decreases its dissolved oxygen levels [33].
We could conclude that the lower the levels of oxygen dissolved in the water that is in contact with the population, the higher the incidence and prevalence of cerebral vascular events or stroke, and vice versa.
This correlation would allow us to design effective interventions, since the basis would be to raise the levels of dissolved oxygen in the drinking water that is distributed to the population, with which, according to statistics, we would probably reduce the incidence and prevalence of stroke and other frequent diseases that increasingly afflict us. For decades it has been said and published that contaminated water, and therefore with low levels of dissolved oxygen; it can cause any type of disease.
Water with low levels of dissolved oxygen should not only not be ingested, but should not be used to wash dishes, much less for cooking, bathing, or washing clothes.
This work was funded by The Human Photosynthesis™ Research Center, Aguascalientes 20000, México.
- Kuriakose D, Xiao Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int J Mol Sci. 2020 Oct 15;21(20):7609. Available from: https://doi.org/10.3390/ijms21207609
- Kelly-Hayes M. Influence of age and health behaviors on stroke risk: Lessons from longitudinal studies. J Am Geriatr Soc. 2010;58:S325–S328. Available from: https://doi.org/10.1111/j.1532-5415.2010.02915.x
- Collaborators G.S. Global, regional, and national burden of stroke, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:439–458. Available from: https://doi.org/10.1016/s1474-4422(19)30034-1
- Appelros P, Stegmayr B, Terént A. Sex differences in stroke epidemiology: A systematic review. Stroke. 2009;40:1082–1090. Available from: https://doi.org/10.1161/strokeaha.108.540781
- Chen JC. Geographic determinants of stroke mortality: Role of ambient air pollution. Stroke. 2010;41:839–841. Available from: https://doi.org/10.1161/strokeaha.110.578476
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021 Oct;20(10):795-820. Available from: https://doi.org/10.1016/s1474-4422(21)00252-0
- Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. Heart disease and stroke statistics—2010 update. A report from the American Heart Association. Circulation. 2009 Feb 23;121(7):948-54. Available from: https://doi.org/10.1161/circulationaha.109.192666
- Lanska DJ. Geographic distribution of stroke mortality in the United States: 1939–1941 to 1979–1981. Neurology. 1993;43:1839–1851. Available from: https://doi.org/10.1212/wnl.43.9.1839
- Lanska DJ, Kuller LH. The geography of stroke mortality in the United States and the concept of a stroke belt. Stroke. 1995;26:1145–1149. Available from: https://doi.org/10.1161/01.str.26.7.1145
- Lanska DJ, Kryscio R. The geographic distribution of hospital admissions, case fatality, and mortality from stroke among Medicare enrollees. Neurology. 1994;44:1541-1550. Available from: https://doi.org/10.1212/wnl.44.8.1541
- Nefzger MD, Kuller LH, Lilienfeld AM, Diamond EL, Miller GD, Stolley PD, et al. Three-area epidemiologic study of geographic differences in stroke mortality, I: Background and methods. Stroke. 1977;8:546-550. Available from: https://doi.org/10.1161/01.str.8.5.546
- Kovar MG, Pokras R, Collins JG. Trends in medical care and survival from stroke. Ann Epidemiol. 1993;3:466-470. Available from: https://doi.org/10.1016/1047-2797(93)90097-n
- Dyken ML, Wolf PA, Barnett HJ, Bergen JJ. Risk factors in stroke: A statement for physicians by the Subcommittee on Risk Factors and Stroke of the Stroke Council. Stroke. 1984;15:1105-1111.
- Lyon JL, Bishop CT, Nielsen NS. Cerebrovascular disease in Utah, 1968-1971. Stroke. 1981;12:564-566. Available from: https://doi.org/10.1161/01.str.12.5.564
- Takahashi E. On the geographic distribution of death rates from vascular lesions affecting the central nervous system in the United States: An epidemiological hypothesis. Tohoku J Exp Med. 1962;76:224-232. Available from: https://www.jstage.jst.go.jp/article/tjem1920/76/3/76_3_224/_pdf
- Gover M. Statistical studies of heart disease, IV: Mortality from heart disease (all forms) related to geographic section and size of city. Public Health Rep. 1949;64:439-456. Available from: https://pubmed.ncbi.nlm.nih.gov/18114617/
- Howard G, Evans GW, Pearce K, Howard VJ, Bell RA, Mayer EJ, et al. Is the stroke belt disappearing? An analysis of racial, temporal and age effects. Stroke. 1995;26:1153-1158. Available from: https://doi.org/10.1161/01.str.26.7.1153
- Wing S, Casper M, Davis WB, Pellom A, Riggan W, Tyroler HA. Stroke mortality maps: United States whites aged 35-74 years, 1962-1982. Stroke. 1988;19:1507-1513. Available from: https://doi.org/10.1161/01.str.19.12.1507
- Solís Herrera A, Arias Esparza MC. Oxygen from the atmosphere cannot pass through the lung tissues and reach the bloodstream. The unexpected capacity of the human body to dissociate the water molecule. J Pulmonol Res Rep. 2022;SRC/JPRR-133. Available from: https://doi.org/10.47363/JPRR/2022(4)124
- Herrera AS. The disdain importance of dissolved oxygen levels in drinking water in pandemic control. Adv Ecol Environ Res. 2020;5(11):296-299. Available from: https://www.ss-pub.org/wp-content/uploads/2020/11/AEER2020102201.pdf
- Blaszczak JR, Koenig LE, Mejia FH, Gómez-Gener L, Dutton CL, Carter AM, et al. Extent, patterns, and drivers of hypoxia in the world's streams and rivers. Limnol Oceanogr Lett. 2023;8:453-463. Available from: https://doi.org/10.1002/lol2.10297
- Total Maximum Daily Load (TMDL) For Dissolved Oxygen in Savannah Harbor Savannah River Basin Chatham and Effingham Counties, Georgia, Jasper County, South Carolina. Available from: https://epd.georgia.gov/sites/epd.georgia.gov/files/related_files/site_page/EPA_SavannahHarbor_DO_TMDL_2006.pdf
- Ji X, Shang X, Dahlgren RA, Zhang M. Prediction of dissolved oxygen concentration in hypoxic river systems using support vector machine: A case study of Wen-Rui Tang River, China. Environ Sci Pollut Res. 2017;24:16062–16076. Available from: https://pubmed.ncbi.nlm.nih.gov/28537025/
- Ni X, Zhou F, Zeng D, Li D, Zhang T, Wang K, et al. Long-term observations of hypoxia off the Yangtze River Estuary: Toward prediction and operational application. In: Frontiers in Ocean Observing: Emerging Technologies for Understanding and Managing a Changing Ocean. E.S. Kappel, V. Cullen, M.J. Costello, L. Galgani, C. Gordó-Vilaseca, A. Govindarajan, S. Kouhi, C. Lavin, L. McCartin, J.D. Müller, B. Pirenne, T. Tanhua, Q. Zhao, S. Zhao, eds. Oceanography. 2023;36(Supplement 1):40–41. Available from: https://doi.org/10.5670/oceanog.2023.s1.13
- Blaszczak JR. Distribution, frequency, and global extent of hypoxia in rivers. U.S. Geological Survey. 2021.
- Pu L, Wang L, Zhang R, Zhao T, Jiang Y, Han L. Projected global trends in ischemic stroke incidence, deaths and disability-adjusted life years from 2020 to 2030. Stroke. 2023;54(5):1330-1339. Available from: https://doi.org/10.1161/STROKEAHA.122.040073
- Pope CA, Dockery DW. Health effects of fine particulate air pollution: Lines that connect. J Air Waste Manag Assoc. 2006;56:709–742. Available from: https://doi.org/10.1080/10473289.2006.10464485
- Bell ML, McDermott A, Zeger SL, Samet JM, Dominici F. Ozone and short-term mortality in 95 US urban communities, 1987–2000. JAMA. 2004;292:2372–2378. Available from: https://doi.org/10.1001/jama.292.19.2372
- Hong YC, Lee JT, Kim H, Kwon HJ. Air pollution: A new risk factor in ischemic stroke mortality. Stroke. 2002;33:2165–2169. Available from: https://doi.org/10.1161/01.str.0000026865.52610.5b
- Wellenius GA, Schwartz J, Mittleman MA. Air pollution and hospital admissions for ischemic and hemorrhagic stroke among Medicare beneficiaries. Stroke. 2005;36:2549–2553. Available from: https://doi.org/10.1161/01.str.0000189687.78760.47
- Dockery DW, Pope CA 3rd, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993;329:1753–1759. Available from: https://doi.org/10.1056/nejm199312093292401
- Simkhovich BZ, Kleinman MT, Kloner RA. Air pollution and cardiovascular injury: Epidemiology, toxicology, and mechanisms. J Am Coll Cardiol. 2008;52:719–726. Available from: https://doi.org/10.1016/j.jacc.2008.05.029
- Hutchins MG, Qu Y, Charlton MB. Successful modelling of river dissolved oxygen dynamics requires knowledge of stream channel environments. J Hydrol. 2021;603(B):126991. Available from: http://dx.doi.org/10.1016/j.jhydrol.2021.126991