More Information
Submitted: June 05, 2024 | Approved: June 12, 2024 | Published: June 13, 2024
How to cite this article: Ahmed AS, Pradhan DK. Remote Effect of Fascial Manipulation on Knee Pain: A Case Report. J Nov Physiother Rehabil. 2024; 8: 017-021.
DOI: 10.29328/journal.jnpr.1001059
Copyright License: © 2024 Ahmed AS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Fascial dysfunction; Hyaluronic acid polymers; Fascial tension
Remote Effect of Fascial Manipulation on Knee Pain: A Case Report
Asifuzzaman Shahriyar Ahmed* and Deepak Kumar Pradhan
Abhinav Bindra Sports Medicine and Research Institute, India
*Address for Correspondence: Asifuzzaman Shahriyar Ahmed, Abhinav Bindra Sports Medicine and Research Institute, India, Email:[email protected]; [email protected]
The study on the remote effect of fascial manipulation on knee pain presents a case report of a patient with knee pain who underwent a single session of fascial manipulation to reduce pain and improve daily activities. The report explains the anatomy of the knee joint and the potential causes of knee pain, including bony and soft tissue involvement. Fascial manipulation is a technique that involves applying mechanical force to areas of fascial dysfunction to stimulate the body’s natural inflammatory response. The therapy is based on applying physical friction to the densified connective tissue with an elbow or knuckle to raise the temperature and change the consistency of loose connective tissue rich in hyaluronic acid. The locations picked were proximal and distal to the problematic area, and no point was treated over the painful region, which is consistent with the notion of pain being caused by aberrant fascial tensions. Manipulation of the connective tissue is thought to cause mechanical stress and heat, resulting in less macromolecular crowding and defragmentation of the Hyaluronic Acid (HA) polymers and normalised fascial gliding across the connective tissue. Reduced discomfort and enhanced range of motion are two more regularly reported effects of Fascial Manipulation. The patient was urged to resume his everyday activities after each treatment session to favour typical physiological motions that would align collagen fibres along normal lines of force. The report concludes that fascial manipulation can be a beneficial technique for managing knee pain, and it can be complemented with exercises and stretches to improve outcomes.
The knee comprises 2 articulations; the patellofemoral joint and the tibio-femoral joint. Stability of the joint is governed by a combination of static ligaments, dynamic muscular force, and menisco capsular and joint loads. Patellofemoral joints transmit tensile forces generated by the quadriceps to the patellar tendon, the patella travels 7 cm caudally during full flexion. Tibiofemoral joints help to transmit the body weight from the femur to the tibia. The screw home mechanism acts where the tibia externally rotates 5 0C in the last 15 0C of extension. The anterior cruciate ligament helps to prevent anterior translation of the tibia and varus stress is prevented by lateral collateral and valgus stress is prevented by the medial collateral ligament and posterior translation is prevented by the posterior cruciate ligament [1].
Knee pain can occur due to bony involvement or soft tissue involvement. In bony involvement, some causes are fracture, osteoarthritis, and dislocation, and in soft tissue involvements, are tendinitis, bursitis, fat pad syndrome, synovitis, strain, ligament sprain, and meniscus tear [2]. The main cause of knee pain occurs mainly due to biomechanical abnormalities like increase Q angle, increase external tibia rotation, increase femoral adduction, increase side bending of the trunk, pes planes and other causes due to overuse injury like repetitive trauma on the soft tissue or joint can also cause knee pain, sudden direct trauma can cause an abnormal force on joint and ligament which cause fracture and ligament sprain. Some other external factors are also responsible for knee pain like inappropriate footwear, inappropriate surface of training, and sudden increase in strengthening exercise loading. Consequences can happen with constant knee pain like chronic pain which can be converted into a central pain pattern, due to the inability to move and can lead to a decreased range of motion, due to weak ligaments that can lead to joint instability, due to abnormal biomechanics it can lead to external tibial rotation and lateral gliding of patella lead to tight lateral retinaculum and tight IT band or IT band friction syndrome [3].
After a knee injury, the main impairments are a decreased range of motion and decreased strength of the quadriceps which leads to difficulty during functional activity such as stair climbing, squatting, and terminal extension of the knee during the mid-stance phase of the gait cycle. Gait abnormality can be seen in patients with knee pain which leads to abnormal force distribution or abnormal loading which leads to inflammation of overloaded structure. Balance impairment is also common in patients with knee pain [4].
Like other causes, tightness of fascia can lead to pain and loss of mobility so to treat fascia there is a manipulation technique called fascial manipulation. It comprises of application of pressure and friction which leads to an improved range of motion, decreases pain, and eases movements. It mainly focuses on the history and identification of the restrictive body segment, and restores the vital step and slide between the fascial layer [5]. It is mainly considered when not responding to other medical conditions and non-diagnosed cases. Recent management protocols for knee injury are extra pectoral shock wave therapy, myofascial release, muscle activation mainly vastus medialis obliques, dry needling, kinesio taping, gluteus maximus strengthening, and kinetic chain correction can help ease knee impairments [6].
The fascia is any tissue with characteristics that may respond to mechanical stimulation. The fascial continuum is the result of the evolution of perfect synergy among various tissues, liquids, and solids capable of supporting, dividing, penetrating, feeding, and connecting all of the body’s districts: epidermis, dermis, fat, blood, lymph, blood and lymphatic vessels, tissue covering the nervous filaments (endoneurium, perineurium, epineurium), voluntary striated muscle fibres, and the tissue covering and permeating it. The continuum is continually transmitting and receiving mechanical metabolic information that has the potential to impact the structure and function of the entire body. These afferent/efferent impulses come from the fascia and the tissues that are not considered part of the fascia in a bi-univocal mode [7].
The fascial tissue in the collective imagination is associated with a solid structure, which can lead to problems related to pain or a disturbance of motor functions [8].
The circumneurium replaces the previous name of paraneurium or paraneural sheath, which is a non-neural tissue or fascia that covers most nerves and is more external than the underlying layer or epineurium; the epineurium may contain adipocyte-containing compartments in its thickness (internal and external), which may be absent or present depending on the overall thickness of the nerve [9].
The three-dimensional continuum of soft, collagen-containing, loose, and thick fibrous connective tissues that pervade the body is known as fascia. Adipose tissue, adventitia and neurovascular sheaths, aponeuroses, deep and superficial fascia, epineurium, joint capsules, ligaments, membranes, meninges, myofascial expansions, periosteum, retinacula, septa, tendons, visceral fasciae, and all intramuscular and intermuscular connective tissues, including endo-/peri-/epimysium are all included. The fascial system surrounds, interweaves through, and interpenetrates all organs, muscles, bones, and nerve fibres, giving the body a functional framework and creating an environment in which all bodily systems may work together [10].
During gastrulation, the mesoderm gives rise to the axial (notochord), paraxial (somites), and lateral regions, which will further split (in the post-gastrulation phase) into anterior and posterior domains [11].
The mesoderm shares multiple transcriptional pathways with the ectoderm, particularly the neural crests, and ectomesenchyme (ectoderm-derived mesenchyme); neural crest cells migrate (delaminate) from the dorsal neural tube to various different organs and parts of the body [12,13].
The Spiral Line (SL) travels through the three cardinal lines, looping around the trunk in the Helix with another loop in the legs from the hip to the arch and back again. It connects one side of the cranium to the opposite shoulder, then across the front of the chest to the same side of the hip, knee, and foot. Return the arch up the back of the body to the head. The SL produces and mediates rotations of the body during movement. The S L interacts with other cardinal lines in a variety of ways. The SL wraps the torso in a double helix posture, which helps to maintain spinal length and balance in all planes. The SL combines the foot arches with knee and pelvic position monitoring. Deeper rotations in the spine or pelvic core are frequently compensated for by the SL [14].
There are numerous studies that have been published to investigate the effect of soft tissue manipulation on knee pain. However, myofascial manipulation being the unique technique among the soft tissue treatments, the evidence is still unclear for various local and remote techniques. The concept of myofascial manipulation is to apply mechanical force to the areas of dysfunction of fascia to stimulate the body’s natural inflammatory response by stimulating the most painful area and along with it one agonist muscle and one antagonist muscle should go through the same mechanical force. For local effect movement with mobilisation has been proven to be beneficial and for remote effect myofascial release and dry needling have proven to be beneficial when compared to other techniques. There have been many studies related to the remote effect of myofascial release in knee pain but the effect was not that beneficial, hence the current study is an attempt to explore the remote effect of myofascial manipulation and its long-standing effects on an individual with knee pain.
A 42-year-old male patient arrived at the outpatient clinic complaining of right shoulder pain and difficulties doing everyday tasks. Before a month, he was fine. However, with time, he began to have soreness in his right shoulder and difficulties doing his everyday chores. There was no discernible medical history. The patient came into our department directly. Assessment of the pain revealed a gradual onset of an intermittent dull aching kind. By using the VAS, the level of discomfort was determined to be 7. Almost all activities that required internal rotation of the shoulder made it worse; in particular, scratching one’s back and putting on a shirt’s sleeves were excruciatingly uncomfortable. On observation, nothing noteworthy was discovered. The patient had grade 3 soreness upon palpation. Rhomboideus on the right side. The right shoulder’s range of motion was examined. Flexion ranges from 0 to 180, Extension from 0 to 20, Abduction from 0 to 180, Horizontal Adduction from 0 to 10, and Internal and External Rotation from 0 to 90. The MRC grading of manual muscle testing was used to evaluate muscle power. There are recordings. While internal rotators were shown to have 3+ power, shoulder flexion, extension, abduction, abduction, and external rotation were found to have 4+ power. Internal rotation of the right shoulder’s passive range of motion revealed an empty terminal feel. We did the Shoulder blade squeeze test and the Hislop-Montgomery test to distinguish this case from Shoulder dyskinesis pain, myofascial pain syndrome, and discogenic symptoms. Except for the Hislop-Montgomery test, which revealed that the right side is weaker than the left, all of the tests were negative. An understanding of the myofascial stiffness of the rhomboideus muscle was gained based on the history and clinical findings mentioned above.
Physiotherapy intervention
A single session of a fascial manipulation programme was planned which aimed at reducing pain and improving the activities of daily living. Baseline scores of pain and range of motion were measured by VAS and universal goniometer.
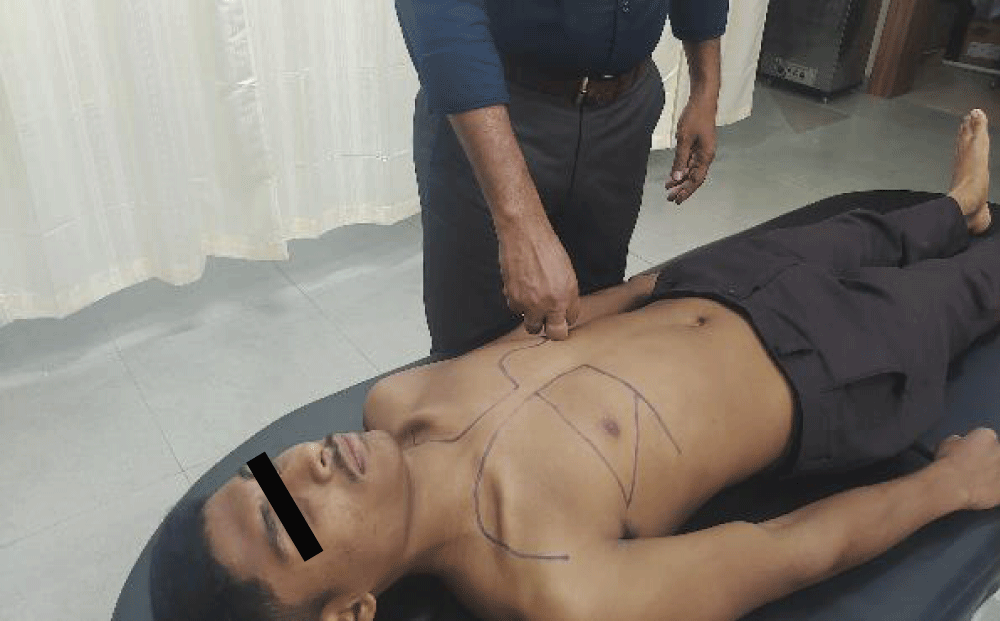
The subject was made to lie supine on the couch and Facial Manipulation was applied on the ANTE THORAX region for 3 minutes. The subject was made to lie prone on the couch and Facial Manipulation was applied on the RETRO THORAX, and RETRO SCAPULAR region for 3 minutes each.
A single session of Facial Manipulation was performed. Immediately after the treatment the pain score measured by VAS reduced from 7 to 2 after the single session and similarly the internal rotation range of motion improved from 40 to 70. No adverse effects were found during or after the treatment (Table 1).
| Table 1: Describes pre and post-VAS scores and ROM of internal rotation. | ||
| PRE | POST | |
| VAS | 7/10 (VAS) | Internal Rotation 50 |
| ROM | 2/10 (VAS) | Internal Rotation 70 |
The aim of this study was to evaluate shoulder ROM before and after the myofascial manipulation of RETRO THORAX, RETRO SCAPULAR, and ANTE THORAX. This case was a trial to find out whether the fascial manipulation can aid remote effects on knee pain or not. The patient showed remarkable improvement after one session only. The patient was a 42-year-old teacher who came with a problem in difficulty during shoulder lateral rotation. The patient was complaining of pain and discomfort while doing all the activities which included lateral rotation and was complaining of incomplete internal rotation of the right shoulder because of pain as the pain was interfering with his ADLs. A goniometer was used for measuring the ROM of the shoulder joint and VAS was used to measure pain.
The assessment chart is divided into four parts: patient details, patient history, patient physical examination (movement and palpation verifications), and treatment. There is a single table for better viewing and understanding. After the assessment, we found that the following points (ante thorax, retro thorax, and retro scapula) show dysfunction and they were treated accordingly. The pictures are the keystone of the method and are taught to all practitioners. Figure 1 represents the ante thorax, Figure 2 represents the retro thorax, and Figure 3 represents the retro scapula. The abbreviations used in the chart have been previously described (Stecco 2004) and are used worldwide. Myers (2010) describes fascia as the richest sensory organ, responsible for nociception, proprioception, increasing postural balance, and acting as a shock absorber in all aspects of motion. As a result, fascial dysfunctions may be one of the key contributors to chronic musculoskeletal discomfort. This case report supports this hypothesis. The therapy is based on applying physical friction to the densified CCs with an elbow or a knuckle to raise the temperature and change the consistency of loose connective tissue rich in hyaluronic acid (Stecco, et al. 2013). Because mechanoreceptors and free nerve endings would be engaged at a lower threshold with mechanical tension on improperly gliding fascial tissue, the therapy is a painful operation.
Figure 1: Ante thorax.
Figure 2: Retro thorax.
Figure 3: Retro scapular.
It should be observed that the locations picked were proximal and distal to the problematic area, and no point was treated over the painful region, which is consistent with the notion of pain being caused by aberrant fascial tensions. Manipulation of the CC is thought to cause mechanical stress and heat, resulting in less macromolecular crowding and defragmentation of the HA polymers (Cowman, et al. 2015) and normalised fascial gliding across the CC. Reduced discomfort and enhanced range of motion are two more regularly reported effects of Fascial Manipulation® (Guarda-Nardini, et al. 2012, Pratelli, et al. 2015, Branchini, et al. 2016, Busato, et al. 2016); indeed, normalised gliding commonly leads to better function. Following modification, the free nerve terminals embedded in the fascia would no longer be stimulated at a lower threshold, and the patient would usually experience pain relief while maintaining the typical sense of pressure. Pain reduction can also be explained by Conditioned Pain Modulation (CPM) by activating the endogenous pain inhibitory system (Bjorkedal & Flaten 2012). The patient was urged to resume his everyday activities at the conclusion of each treatment session in order to favour typical physiological motions that would align collagen fibres along normal lines of force (Chaitow 2014).
The results indicate that RETRO THORAX, RETRO SCAPULAR, and ANTE THORAX increased the internal rotation of the shoulder joint. Treatment directed towards neighbouring or remote myofascial structures via specific fascial connectivity could prove to be effective in reducing pain (Grieve, 2015). As per the myofascial meridian concept both these regions form a part of the SBL (Superficial back line), a fascial connectivity that extends from head to toe through the posterior aspect of the body. Studies of myofascial force transmission confirm that the actual stiffness of the general fascia and fascial compartments appear to be very important for the quantity of myofascial force transmission (Huijing and Baan, 2003). Both Paoletti (2002) and Stecco (2004) hypothesise that the deep fascia between two joints is directly involved in safeguarding a perceptive and directional continuity along a specific myokinetic chain or sequence. It could be that fascia acts somewhat like a sensitive transmission belt between two adjacent joints and synergic muscle groups. The precise stretching of selective regions of the fasciae due to these muscular expansions could activate receptors embedded in the fasciae (Barker, 1974; Stecco, et al.
2006). Fascial Manipulation theory (Stecco, 2004), distal paraesthesia may occur when the fascia is not free to glide and subsequent fascial tension along a sequence culminates in the terminal part of a sequence. Stecco (2004) also suggests that this mechanism implies a basal or resting tension of the fascia. Fascial manipulation on these specific points (CC and CF) aims at restoring tensional balance. Compensatory tension may extend along a myofascial sequence so myofascial continuity could be involved in the referral of pain along a limb or at a distance, even in the absence of specific nerve root disturbance [15].
Stecco proposes that when gamma fibre stimulation causes intrafusal spindle fibres to contract a minimal stretch could be propagated throughout the entire fascial continuum, including tensioning the deep fascia at the CC. If this fascial continuum is elastic, then it could adapt to this stretch permitting muscle spindles to contract normally with subsequent correct activation of alpha motor fibres and muscular contraction [16].
Stretching the joint capsule and surrounding ligaments can help with ROM. Stretching can cause connective tissue elongation and remodelling, allowing for increased joint mobility. Muscles are essential for joint mobility. Muscle lengthening and relaxation can improve ROM by decreasing muscle stiffness and resistance to joint mobility. Neuromuscular regulation is essential for proper joint function. Neuromuscular control training and exercises can improve ROM by developing coordination, stability, and efficient movement patterns.
The mechanism as to how manual therapy regulates inflammation remains elusive. Therefore, the authors hypothesised that the human fascial system induces proinflammatory mediators in response to RMS; and that direct (MFR model) or indirect (SCS model) manipulation, reduces such secretions (Meltzer and Standley, 2007; Meltzer, et al. 2010). Fibroblast activity not only participates in muscle repair but represents a key step in the wound healing process, involving secretions of necessary proinflammatory cytokines and extracellular matrix proteins that enhance proliferation, migration, and angiogenesis (Tettamanti, et al. 2004). It has been observed that lower magnitude (3% to 6%) and longer duration (5 min) improved wound healing in-vitro. This mechanism could be attributed to changes in the extracellular matrix (eg, collagen synthesis, secretion, and architecture) that might result from MFR applied for longer than 2 min. The role of cell remodelling could be explained by the regulation of interstitial fluid pressure and flow. This mechanism might serve as protection against fluid stasis by keeping the matrix under tension equilibrium (Langevin, et al. 2013a,b) [17].
The limitations of this case report are inherent in the research design and include the inability of these findings to be generalizable to the general population. The outcome measures were immediately used after the first session, indicating the necessity for further research that includes randomised controlled trials with a larger sample size compared to gold-standard physiotherapeutic treatment in these kinds of patients followed by a long-term follow-up.
Ethical considerations
The author obtained written consent from the participant for the study.
Author contribution
Author A: Asifuzzaman Shahriyar Ahmed.
Author B: Deepak Kumar Pradhan
Conceived and designed the analysis - A
Collected the data - A
Contributed data or analysis tools - A
Performed the analysis - A and B
Wrote the paper - A and B
Other contribution - NA
- Flandry F, Hommel G. Normal anatomy and biomechanics of the knee. Sports Med Arthrosc Rev. 2011 Jun;19(2):82-92. doi: 10.1097/JSA.0b013e318210c0aa. PMID: 21540705.
- Farrokhi S, Chen YF, Piva SR, Fitzgerald GK, Jeong JH, Kwoh CK. The Influence of Knee Pain Location on Symptoms, Functional Status, and Knee-related Quality of Life in Older Adults With Chronic Knee Pain: Data From the Osteoarthritis Initiative. Clin J Pain. 2016 Jun;32(6):463-70. doi: 10.1097/AJP.0000000000000291. PMID: 26308705; PMCID: PMC4766069.
- Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med. 2011 Spring;2(2):205-12. PMID: 24024017; PMCID: PMC3766936.
- O'Reilly SC, Muir KR, Doherty M. Knee pain and disability in the Nottingham community: association with poor health status and psychological distress. Br J Rheumatol. 1998 Aug;37(8):870-3. doi: 10.1093/rheumatology/37.8.870. PMID: 9734678.
- Rajasekar S, Marchand AM. Fascial Manipulation® for persistent knee pain following ACL and meniscus repair. J Bodyw Mov Ther. 2017 Apr;21(2):452-458. doi: 10.1016/j.jbmt.2016.08.014. Epub 2016 Sep 4. PMID: 28532890.
- Li R, Chen H, Feng J, Xiao Y, Zhang H, Lam CW, Xiao H. Effectiveness of Traditional Chinese Exercise for Symptoms of Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int J Environ Res Public Health. 2020 Oct 27;17(21):7873. doi: 10.3390/ijerph17217873. PMID: 33121082; PMCID: PMC7662219.
- Bordoni B, Escher AR, Tobbi F, Ducoux B, Paoletti S. Fascial Nomenclature: Update 2021, Part 2. Cureus. 2021 Feb 11;13(2):e13279. doi: 10.7759/cureus.13279. PMID: 33604227; PMCID: PMC7880823.
- Hutchinson LA, Lichtwark GA, Willy RW, Kelly LA. The Iliotibial Band: A Complex Structure with Versatile Functions. Sports Med. 2022 May;52(5):995-1008. doi: 10.1007/s40279-021-01634-3. Epub 2022 Jan 24. PMID: 35072941; PMCID: PMC9023415.
- Hutchinson LA, Lichtwark GA, Willy RW, Kelly LA. The Iliotibial Band: A Complex Structure with Versatile Functions. Sports Med. 2022 May;52(5):995-1008. doi: 10.1007/s40279-021-01634-3. Epub 2022 Jan 24. PMID: 35072941; PMCID: PMC9023415.
- Schleip R, Adstrum S, Hedley G, Stecco C, Yucesoy CA. Regarding: Update on fascial nomenclature - An additional proposal by John Sharkey MSc, Clinical Anatomist. J Bodyw Mov Ther. 2019 Jan;23(1):9-10. doi: 10.1016/j.jbmt.2018.12.002. Epub 2018 Dec 6. PMID: 30691769.
- Paulissen E, Palmisano NJ, Waxman JS, Martin BL. Somite morphogenesis is required for axial blood vessel formation during zebrafish embryogenesis. Elife. 2022 Feb 9;11:e74821. doi: 10.7554/eLife.74821. PMID: 35137687; PMCID: PMC8863375.
- Fabian P, Crump JG. Reassessing the embryonic origin and potential of craniofacial ectomesenchyme. Semin Cell Dev Biol. 2023 Mar 30;138:45-53. doi: 10.1016/j.semcdb.2022.03.018. Epub 2022 Mar 21. PMID: 35331627; PMCID: PMC9489819.
- Okuno H, Okano H. Modeling human congenital disorders with neural crest developmental defects using patient-derived induced pluripotent stem cells. Regen Ther. 2021 Aug 24;18:275-280. doi: 10.1016/j.reth.2021.08.001. PMID: 34504908; PMCID: PMC8390449.
- Thomas W. Myers: An Introduction to Anatomy Trains Myofascial Meridians
- Day JA, Stecco C, Stecco A. Application of Fascial Manipulation technique in chronic shoulder pain--anatomical basis and clinical implications. J Bodyw Mov Ther. 2009 Apr;13(2):128-35. doi: 10.1016/j.jbmt.2008.04.044. Epub 2008 Jun 24. PMID: 19329049.
- Stecco L, Stecco C. Fascial Manipulation: Practical Part. Padova: Piccin; 2009.
- Parravicini G, Bergna A. Biological effects of direct and indirect manipulation of the fascial system. Narrative review. J Bodyw Mov Ther. 2017 Apr;21(2):435-445. doi: 10.1016/j.jbmt.2017.01.005. Epub 2017 Jan 9. PMID: 28532888.