More Information
Submitted: October 20, 2022 | Approved: October 25, 2022 | Published: October 26, 2022
How to cite this article: Santi M, Diener I, Oostendorp R. Assessment and treatment of patients with kinesiophobia: A Delphi consensus. J Nov Physiother Rehabil. 2022; 6: 023-028.
DOI: 10.29328/journal.jnpr.1001047
Copyright License: © 2022 Santi M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Assessment; Treatment; Kinesiophobia; Delphi
Assessment and treatment of patients with kinesiophobia: A Delphi consensus
Mattias Santi1* , Ina Diener2 and Rob Oostendorp3-5
, Ina Diener2 and Rob Oostendorp3-5
1Reunion Masso-Kinesitherapy Training Institute, CHU SUD, Saint-Pierre, France
2Department Physiotherapy, University of the Western Cape, Cape Town, South Africa
3Scientific Institute for Quality of Healthcare, Radboud University Nijmegen Medical Centre, Nijmegen, the Netherlands
4Department of Manual Therapy, Faculty of Medicine and Pharmacy, Free University of Brussels, Brussels, Belgium
5Pain in Motion International Research Group, Faculty of Physical Education and Physiotherapy, Free University of Brussels, Brussels, Belgium
*Address for Correspondence: Mattias Santi, Reunion Masso-Kinesitherapy Training Institute, CHU SUD, Saint-Pierre, France, Email: [email protected]
Kinesiophobia is described as pain-related fear of movement and plays a role in the development of chronic musculoskeletal pain. Several approaches have been described in the literature, but there does not seem to be a consensus on the most appropriate way to evaluate and treat patients with kinesiophobia. The aim of this study was to identify clinically relevant assessments and treatments recommended by a consensus of experts. Fourteen experts were identified to participate in a three-round internet-based Delphi study. Participants were asked to propose assessments and treatments (round 1), to grade each proposal on a Likert scale of 9 (round 2), and to reassess their level of agreement (round 3). The consensus was defined with 75% agreement. Five methods of assessment and six treatment approaches reached a consensus. The TAMPA scale reached the top position as an assessment of kinesiophobia. Graded exposure to movement, cognitive and behavioral therapy, and pain neuroscience education were the highest-rated interventions. These results provide the first expert consensus on preferred assessments and treatments for patients with kinesiophobia and correspond with the evidence base in the literature.
Kinesiophobia or fear of movement is defined as “an excessive, irrational and debilitating fear to carry a physical movement, due to a feeling of vulnerability to a painful injury or reinjury” [1]. Fear is the anticipated emotional response to an imminent threat [2]. According to Vlayen, et al. [2], fear develops through adaptive learning when a subject will associate acute pain with movements, and repetition of these movements will have the capacity to trigger pain even if recovery is achieved. This fear can then generalise and other initially neutral movements, may trigger pain.
There is a 79% prevalence of kinesiophobia among patients suffering from musculoskeletal pain referred for physiotherapy in France [3]. Patients with kinesiophobia have a longer duration of physiotherapy care, lower levels of satisfaction with care [3-5] increased disability, and reports of higher pain intensity compared to patients without kinesiophobia [6].
Kinesiophobia is considered a maladaptative pain behavior that has been identified as a strong contributor to the development of chronic pain [5,6]. The assessment of components of pain behavior is an integral part of a biopsychosocial approach, but there does not seem to be a consensus on the best way to assess kinesiophobia [7]. Some questionnaires focus on the assessment of patients with kinesiophobia, such as the Tampa Scale for Kinesiophobia (TSK) [8], the Fear Avoidance Beliefs Questionnaire (FABQ) [9], the Pain Anxiety Symptoms Scale (PASS) [10], as well as the Photograph series of daily activities (PHODA) [11].
Several studies have investigated exercise interventions for patients with kinesiophobia such as functional [12], aerobic [13] and Pilates [14]. Other studies reported on education [15], cognitive-behavioral therapies [16], and innovative techniques such as virtual reality [17]. According to Xu, et al. (2020), a combination of physical and psychological rehabilitation has the best evidence to reduce kinesiophobia.
There are currently many assessments and treatments for kinesiophobia in the literature, but there does not seem to be a consensus for the assessment or the treatment of patients with kinesiophobia [18]. Secondly, a wide variety of interventions described in the literature makes it difficult for clinicians to choose the most effective treatment for kinesiophobia. Establishing a consensus between experts may assist clinicians in decision-making [19]. Therefore, the aim of this study was to establish consensus about the assessment and treatment of patients with kinesiophobia.
Design
The Delphi technique is a structured mixed method of research for obtaining opinions on given issues by a group of experts [20]. It is increasingly used in research as a tool to address problems and develop consensus advice on best practices. In accordance with the recommendations on Conducting and Reporting Delphi Studies (CREDES), a process characterized by the involvement of experts with diverse and international representation was implemented [21]. The process was iterative, involving two or more rounds.
Participants
A sampling strategy was used to recruit ‘experts’ defined as individuals with priori-rich knowledge and relevant clinical expertise related to the field of kinesiophobia. The experts were selected according to the following inclusion criteria: (1) publication of an article in a peer-reviewed journal with one of the following keywords in the title or abstract: “kinesiophobia” “pain-related fear” “pain-related avoidance” “fear avoidance” “fear of movement”; and (2) being a health professional.
After a review of three biomedical databases (PubMed, Google Scholar, Science Direct) and three thesis databases (ProQuest, OATD, theses) and the use of the keywords mentioned above, 162 authors with at least one published article and 4 Ph.D. students on the topic, were identified. We were able to extract the contact information (e-mail) of 60 authors and 3 Ph.D., students.
Delphi process
The study consisted of three rounds with one online questionnaire per round available in English or French and hosted with the software [SphinxDéclic© https://sphinxdeclic.com]. Identified experts (n = 63) were invited to participate via an email that included key information about the study, its interest, its purpose, and how it would reach a consensus. The questionnaires were available online for two weeks each. Two reminders were sent to participants (on day 5 and day 10). In the second and third rounds, we used a 9 Likert scale to measure the degree of agreement of an expert with a proposition from 1 for “strongly disagree” to 9 for “strongly agree. A consensus would be considered as reached if at least 75% of respondents scored > 5 on the 9-point Likert scale [22]. The consensus was reached in the second or third round. After each round, the average response of the group was summarised in a report given to each respondent, allowing them to reconsider their own views on the subject. In order to comply with the CREDES recommendations, the aforementioned characteristics were integrated into our Delphi study. This project was exempted from ethics review under French law.
Round 1: The 1st qualitative questionnaire (Figure 1) was explorative, with open-end questions. This questionnaire allowed us to describe the participating experts (training, experience, number of patients with kinesiohobia) and to explore the assessment and treatment options that the expert proposed for patients with kinesiophobia. The questions were focused on the clinical signs of patients with kinesiophobia and on the assessment to identify this behavior. The treatment questions were focused on how the participating expert would adapt treatment for a patient with kinesiophobia, and what the best treatment options were preferred to reduce this deficit. The data from the 1st questionnaire were analyzed qualitatively via content analysis [20].
Round 2: On the basis of the results from Round 1, questions were rephrased and presented for the second round. The questionnaire was quantitative with closed questions and the experts were asked to rate their agreement on a 9-point Likert scale. A lack of a vote on a question was considered indecision, i.e. a rating of 5. For each proposal, a weighted average was calculated in order to rank the consensus. The strongest consensus was recorded as the proposals with the highest possible weighted average (maximum value 9).
The weighted average formula (m) was:
m = (Σ rate)/n
- Rate is the value assigned by the experts on the Likert scale of 9 for a given proposal.
- n is the number of respondents
For example: In the second round there were 14 participants (n = 14) and on the proposal of the TSK score the total of the scores is 109.
The weighted average is then n = 109/14 = 7.79 (with the minimum weighted average of 1 and the maximum of 9).
Round 3: The questionnaire was quantitative with closed questions, and the experts were asked to rate their agreement on the same 9-point Likert scale. This questionnaire contained the results of the 2nd questionnaire (mean, median and dispersion), but did not contain proposals that have already been accepted in the 2nd round (75% of respondents scored > 5). For each proposal, a weighted average was calculated as it was done in the 2nd round.
Participation per round
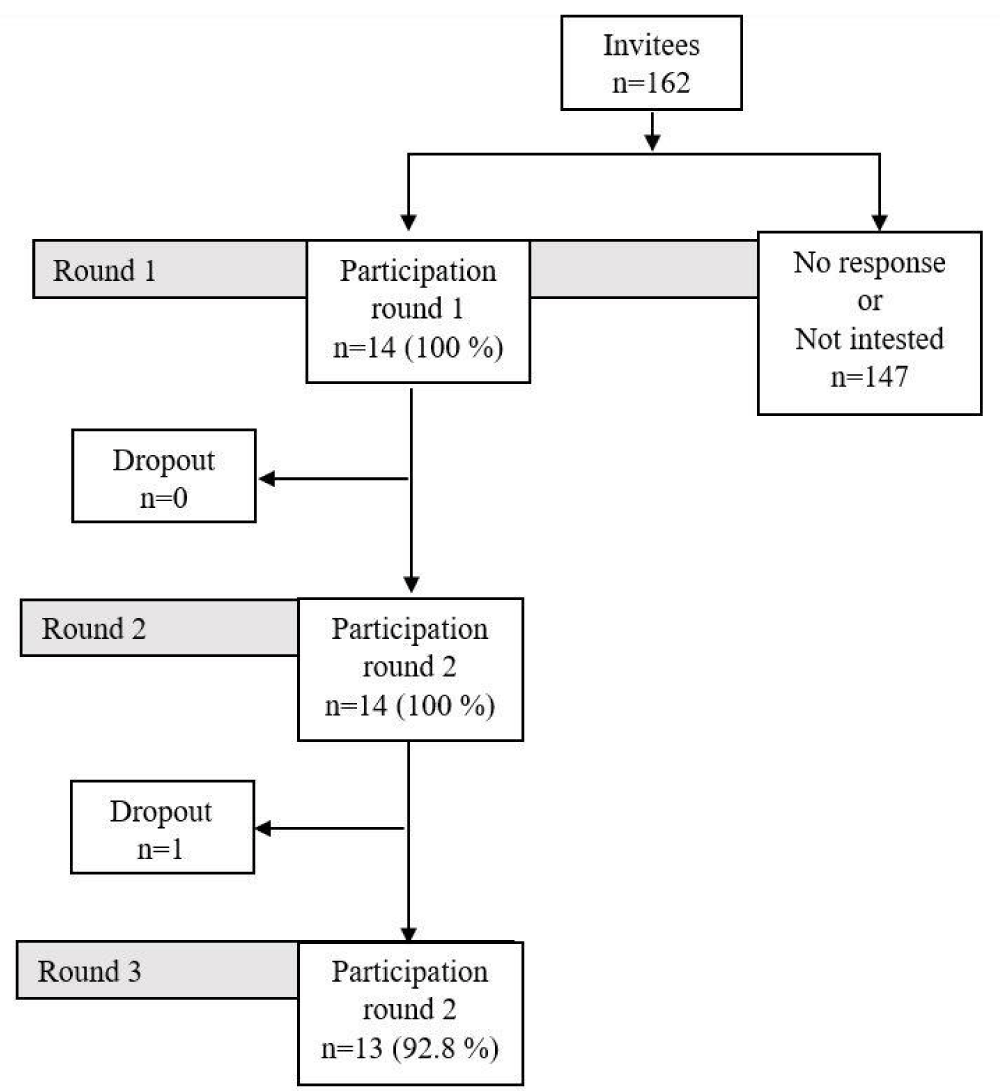
Of the 163 invitation emails sent, 14 invitees responded to participating in the study (Figure 1).
Figure 1: Flowchart of participants in Delphi procedure.
In Round 1, 14 experts (100%), in round 2, 14 experts (100%) and in round 3, 13 experts (92.8%). The characteristics of the respondents are presented in Table 1. There was international representation, with participants from 11 countries and a multidisciplinary panel.
| Table 1: Characteristics of respondents. | ||
| Gender | Male (n = 8) | Female (n = 6) |
| Country of origin | France (n = 3), Netherlands (n = 2), China (n = 1), South Africa (n = 1), Brazil (n = 1), Nigeria (n = 1), Cyprus (n = 1), Australia (n = 1), Turkey (n = 1), Iran (n = 1), USA (n = 1) | |
| Diploma* | Physiotherapist (n = 9), doctor of medicine (MD) (n = 7), psychologist (n = 1) | |
| Average age [standard deviation] | 43 years [s = 13] | |
| Number of kinesiophobic patients treated per month | 4 [s = 3] | |
| Input language | English (n = 11) | French (n = 3) |
| Expertise | 12 published an article on kinesiophobia in a scientific journal. | 2 validated their thesis on kinesiophobia |
| Conflict of interest | 0 % | |
| *more than 1 option could be selected; s: standard deviation | ||
Results of round 1
The results of the 1st round are presented in Table 2 assessment proposals and 11 treatment proposals.
| Table 2: Proposals from content analysis after round 1. | ||
| Proposals | Assessment of kinesiophobia | Treatment of kinesiophobia |
| 1 | TSK | Graduated in vivo exposure |
| 2 | Patient-specific questions (What movements do you dread? What can you no longer do?) |
Behavioral and cognitive therapy |
| 3 | Photographs | Education in the neuroscience of pain |
| 4 | FABQ scale | Therapeutic education |
| 5 | Questions about patient motivation (What are your goals? What do you wish for your end of rehabilitation?) |
Motivational interviewing |
| 6 | KINAP questionnaire | Imagined movements |
| 7 | Stabilisation exercises | |
| 8 | Mirror therapy | |
| 9 | Restraint of the area (splint) | |
| 10 | Aerobic activity | |
| 11 | Music | |
| TSK: Tampa Scale of Kinesiopbia; FABQ: Fear Avoidance Beliefs Questionnaire; KINAP: questionnaire: KINesiophobia in Physical Activity (a pictorial instrument measuring fear of specific physical activities). | ||
Results of round 2 and round 3
Details of the scores on each proposal in the second and third rounds are presented in Table 3.
| Table 3: Consensus scores on proposals. | |||||
| Assessment of kinesiophobia | |||||
| Proposals | Round | > 5 | = 5 | < 5 | m |
| TSK | 2 | 14/14 (100%) | 7.79 | ||
| Patient-specific questions | 2 | 11/14 (79 %) | 2/14 (14%) | 1/14 (7 %) | 7.64 |
| Photographs | 2 | 12/14 (86 %) | 2/14 (14 %) | 7.14 | |
| FABQ scale | 2 3 |
10/14 (71 %) 12/13 (92 %) |
1/14 (7 %) | 3/14 (21 %) 1/13 (8 %) |
6.71 6.92 |
| Questions about patient motivation | 2 3 |
9/14 (64 %) 10/13 (77 %) |
2/14 (14%) 2/13 (15%) |
3/14 (21 %) 1/13 (8 %) |
6.00 6.23 |
| KINAP questionnaire | 2 3 |
4/14 (46 %) 6/13 (46 %) |
10/14 (43%) 6/13 (46 %) |
0/14 (8 %) 1/13 (8 %) |
5.64 5.46 |
| Treatment of kinesiophobia | |||||
| Proposals | Round | > 5 | = 5 | < 5 | m |
| Behavioral and cognitive therapy | 2 | 14/14 (100%) | 7.79 | ||
| Graduated in vivo exposure | 2 | 12/14 (86 %) | 2/14 (14%) | 7.71 | |
| Therapeutic education | 2 | 13/14 (93 %) | 1/14 (7 %) | 7.50 | |
| Education in the neuroscience of pain | 2 | 13/14 (100%) | 1/14 (7 %) | 7.43 | |
| Motivational interviewing | 2 | 12/14 (86 %) | 1/14 (7 %) | 1/14 (7 %) | 6.79 |
| Imagined movements | 2 3 |
10/14 (71 %) 10/13 (77%) |
3/14 (22%) 1/13 (8%) |
1/14 (7 %) 2/13 (15%) |
6.64 6.31 |
| Stabilisation exercises | 2 3 |
7/14 (50%) 8/13 (62%) |
3/14 (21%) 4/13 (31%) |
4/14 (29%) 1/13 (8%) |
5.79 5.92 |
| Mirror therapy | 2 3 |
7/14 (50%) 7/13 (54%) |
3/14 (21%) 4/13 (31%) |
4/14 (29%) 2/13(15%) |
4.86 5.46 |
| Restraint of the area (splint) | 2 3 |
6/14 (43%) 7/13 (54%) |
3/14 (21%) 2/13 (15%) |
5/14 (36%) 4/13 (31%) |
5.36 5.46 |
| Aerobic activity | 2 3 |
6/14 (43%) 6/13 (46%) |
3/14 (21%) 2/13 (15%) |
5/14 (36%) 5/13 (39%) |
4.93 4.92 |
| Music | 2 3 |
4/14 (29%) 4/13 (31%) |
6/14 (43%) 3/13 (23%) |
4/14 (29%) 6/13 (46%) |
5.29 4.62 |
| • " > 5 " indicates the number of participants who gave a score higher than 5/9 on the given proposal. If there is more than 75% of the panel scoring higher than 5/9, the proposal is considered accepted or consensual. • in bold are the proposals that received a consensus (75% of values > 5). • m is the weighted average. |
|||||
Participants reached a consensus on 5 out of 6 (83%) assessment proposals. The proposals with the strongest consensus were TSK (m = 7.79), patient-specific questions (m = 7.64), photographs (m = 7.14), FABQ scale (m = 6.92), and questions about patient motivation (m = 6.23).
Participants reached a consensus on 6 out of 11 (54,5%) treatment proposals. In descending order of the proposals with the strongest consensus, the results are behavioral and cognitive therapy (m = 7.79), graduated in vivo exposure (m = 7.71), therapeutic education (m = 7.50), education in the neuroscience of pain (m = 7.43), motivational interviewing (m = 6.79), imagined movements (m = 6.31).
To the best of our knowledge, this is the first study that established consensus about the assessment and treatment of patients with kinesiophobia with musculoskeletal pain. The main results demonstrated 5 consensus assessment tools and 6 treatment tools for patients with kinesiophobia.
Assessment of Kinesiophobia
In the current study consensus about the assessment of kinesiophobia are the TSK scale, Patient-specific questions, Photographs, the FABQ scale, and Questions about patient motivation. Therefore, the consensus of experts in the field was in close agreement with the literature review by Lundburg, et al. (2011), where the TSK scale and FABQ scale are among the 5 optimum measures for kinesiophobia, with the Fear-Avoidance of Pain Scale (FAPS), Fear of Pain Questionnaire (FPQ), Pain and Anxiety Symptoms Scale (PASS). The TSK scale and FABQ in the assessment of kinesiophobia are described in several studies and demonstrate good reliability and validity [18,23-26].
The use of photographs in the assessment of kinesiophobia is known in the literature with the PHODA questionnaire which has been tested in terms of clinometry in its short version called PHODA-sev [11]. It can assist clinicians to target and monitor activities that patients perceive as harmful, encouraging them to gradually face them in order to restore function [27].
In our Delphi study, new kinesiophobia assessments not listed in the literature were agreed upon, such as questions specific to the patient’s condition (What movements do you dread? What can you no longer do?) and to the patient’s motivation (What are your goals? What do you wish for your end of rehabilitation?). Specific questions can help clinicians to identify the specific movements/activities which patients fear. Moreover, it is useful to grade the patient’s fear in order to achieve gradual exposure to activities. Motivational questions may assess the patient’s barriers and levers to exposure, and identify the patient’s functional goals.
Treatment/rehabilitation of kinesiophobia
The treatment options that reached consensus are behavioral and cognitive therapy, graduated in vivo exposure, education in the neuroscience of pain, motivational interviewing, and imagined movements.
Cognitive behavior therapy is a structured, didactic, and goal-oriented form of therapy. The therapist and patient work in a collaborative manner with the goal of modifying patterns of thinking and behavior [28]. Concerning the reduction of kinesiophobia, a study showed effects in the medium term [29]. Among patients with kinesiophobia, psychological distress can appear in the forms of anxiety, depression, or behavioral irregularities. Cognitive behavior therapy aims to influence such issues and thereby kinesiophobia [30].
Gradual exposure to feared activities significantly reduces kinesiophobia [32]. Patients who are gradually exposed to feared activities become more comfortable with activities by readjusting their beliefs about the outcome of performing it, particularly regarding the likelihood that the activity will produce pain [32]. A reduction in the perceived threat of activity and disconfirmation of negative beliefs likely leads to an improved ability to predict pain, resulting in decreased hypervigilance and threat assessment, which in turn leads to decreased kinesiophobia.
Imagined movements are one part of Graded Motor Imagery (GMI) which has been shown to significantly reduce kinesiophobia in the short term [33]. GMI produces an effect on the central nervous system and may decrease sensory activity in structures related to emotional and affective factors of pain, such as catastrophizing and fear of movement [33]. This therapeutic tool may therefore reduce the sensation of threat or “danger” and tissue restriction.
Education can reduce kinesiophobia [15,34,35], by changing/decreasing fear beliefs. This may facilitate patients’ understanding of the value of gradually exposing themselves to the activities they fear [35]. It is important to distinguish between education in the broad sense, which is the transmission of knowledge about the patient’s illness (prognosis, evolution, symptoms, etc.), and pain neuroscience education (PNE), which is s an educational model which increases the patient’s level of knowledge about pain neurophysiology. The patients learn the physiology of the nervous system, as well as the neurobiology of pain, in an easy-to-understand manner through the use of drawings, prepared images, examples, metaphors, and pamphlets to supplement the explanations. The patients will then understand that pain is not equal to harm, persisting pain is not correlated with tissue damage, and that pain is modulated by many factors [36]. Pain neuroscience education (PNE) has evolved in recent years and has demonstrated a reduction in pain-related fear [34,37]. Finally, to maximize the effect of education on the reduction of kinesiophobia, it seems appropriate to combine it with physical therapy [38].
All the interventions for kinesiophobia that the expert participants agreed upon in this Delphi study are present in the literature. This may demonstrate a quality criterion because consensus is reinforced by external scientific evidence (Jünger, et al. 2017). The results of the study confirm that experts in the field use, or propose to use, assessments and interventions that have an evidence base in the scientific literature. Furthermore, consensus demonstrated both the physical and psychological side of kinesiophobia to be addressed in the therapeutic intervention [39].
Clinical implications
This study has practical applications for the clinician who would have to take care of a patient with kinesiophobbia. Clinicians can orient their choice of assessments and treatments towards the recommendations of this study if the ‘patient’s wish’ and his ‘therapist’s experience’ allow it [40]. Thus, in the assessment of the patient with kinesiophobia, it is recommended to use the TAMPA or FABQ score to confirm and evaluate the intensity of the kinesiophobia, ask “specific questions” to the patient and use photographs of daily activities to prioritize the patient’s dreaded activities. As an intervention, it is recommended to do a motivational interview followed by therapeutic education (about the neuroscience of pain) before moving on to gradual exposure. Gradual exposure can be done physically with exercises adapted to the patient’s current level of fear, but it can also be done mentally with gradual motor imagery (GMI). Finally, it is recommended to set up cognitive behavior therapy to help the patient with kinesiophobia.
Strengths and limitations of the study
This study followed the recommendations of CREDES. These are recommendations on the rigorous conduct of studies using the Delphi technique for the development of good practice guidelines in the health field and a standard for the transparent reporting of Delphi studies (Conducting and REporting of DElphi Studies (CREDES)) (Jünger, et al. 2017).
The results of this study should be interpreted in light of a number of methodological limitations. Firstly, the consensuses are based only on the theoretical knowledge and/or clinical experience of the study participants. Secondly, the purposive sampling strategy and small sample size (n = 13) employed in this study may limit the generalisability of its results. Furthermore, in the absence of any standardized guidelines for defining and selecting experts, the credibility and expertise of the study participants must be inferred and assumed from their composition and professional attributes. A differently defined group of experts might have produced different results. In order to reduce the burden on participants, the consensuses in this study were ranked according to their relative importance using the weighted average. Other rankings could have been produced if the participants themselves had been asked to rank them.
Research perspectives
The present study has created recommendations, but they lack guidance. We know which techniques to use, but we don’t know when to use which techniques. Further studies using appropriate methodologies should focus on the creation and validation of categories of patients with kinesiophobia. These categories allow the identification of treatment indications according to categories of patients with kinesiohobia [41]. This will allow us to identify groups of patients who would respond best to a type of treatment in order to refine the decision support for a patient with kinesiophobia.
This study identifies recommended assessments and treatments for kinesiophobia based on an expert consensus. It provides a first decision aid to choose relevant tools for assessment and treatment.
- Kori SH. Kinisophobia : A new view of chronic pain behavior . Pain Manage Jan:/Feb:35‑43,1990.
- Vlaeyen JWS, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain. 2016 Aug;157(8):1588-1589. doi: 10.1097/j.pain.0000000000000574. PMID: 27428892.
- Perrot S, Trouvin AP, Rondeau V, Chartier I, Arnaud R, Milon JY, Pouchain D. Kinesiophobia and physical therapy-related pain in musculoskeletal pain: A national multicenter cohort study on patients and their general physicians. Joint Bone Spine. 2018 Jan;85(1):101-107. doi: 10.1016/j.jbspin.2016.12.014. Epub 2017 Jan 3. PMID: 28062380.
- Brown OS, Hu L, Demetriou C, Smith TO, Hing CB. The effects of kinesiophobia on outcome following total knee replacement: a systematic review. Arch Orthop Trauma Surg. 2020 Dec;140(12):2057-2070. doi: 10.1007/s00402-020-03582-5. Epub 2020 Aug 24. PMID: 32839826.
- Filardo G, Roffi A, Merli G, Marcacci T, Ceroni FB, Raboni D, Bortolotti B, De Pasqual L, Marcacci M. Patient kinesiophobia affects both recovery time and final outcome after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016 Oct;24(10):3322-3328. doi: 10.1007/s00167-015-3898-8. Epub 2015 Dec 19. PMID: 26685685.
- Luque-Suarez A, Martinez-Calderon J, Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J Sports Med. 2019 May;53(9):554-559. doi: 10.1136/bjsports-2017-098673. Epub 2018 Apr 17. PMID: 29666064.
- Ng W, Slater H, Starcevich C, Wright A, Mitchell T, Beales D. Barriers and enablers influencing healthcare professionals' adoption of a biopsychosocial approach to musculoskeletal pain: a systematic review and qualitative evidence synthesis. Pain. 2021 Aug 1;162(8):2154-2185. doi: 10.1097/j.pain.0000000000002217. PMID: 33534357.
- Weermeijer JD, Meulders A. Clinimetrics: Tampa Scale for Kinesiophobia. J Physiother. 2018 Apr;64(2):126. doi: 10.1016/j.jphys.2018.01.001. Epub 2018 Mar 19. PMID: 29567379.
- Williamson E. Fear Avoidance Beliefs Questionnaire (FABQ). Aust J Physiother. 2006;52(2):149. doi: 10.1016/s0004-9514(06)70052-6. PMID: 16805041.
- McCracken LM, Zayfert C, Gross RT. The Pain Anxiety Symptoms Scale: development and validation of a scale to measure fear of pain. Pain. 1992 Jul;50(1):67-73. doi: 10.1016/0304-3959(92)90113-P. PMID: 1513605.
- Oliveira CB, Pinto RZ. Clinimetrics: Photograph Series of Daily Activities - Short Electronic Version (PHODA-SeV). J Physiother. 2021 Jul;67(3):222. doi: 10.1016/j.jphys.2020.09.006. Epub 2020 Oct 20. PMID: 33097439.
- Monticone M, Ferrante S, Rocca B, Salvaderi S, Fiorentini R, Restelli M, Foti C. Home-based functional exercises aimed at managing kinesiophobia contribute to improving disability and quality of life of patients undergoing total knee arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil. 2013 Feb;94(2):231-9. doi: 10.1016/j.apmr.2012.10.003. Epub 2012 Oct 12. PMID: 23063624.
- Mannion AF, Müntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine (Phila Pa 1976). 1999 Dec 1;24(23):2435-48. doi: 10.1097/00007632-199912010-00004. PMID: 10626305.
- Domingues de Freitas C, Costa DA, Junior NC, Civile VT. Effects of the pilates method on kinesiophobia associated with chronic non-specific low back pain: Systematic review and meta-analysis. J Bodyw Mov Ther. 2020 Jul;24(3):300-306. doi: 10.1016/j.jbmt.2020.05.005. Epub 2020 May 12. PMID: 32826004.
- de Jong JR, Vlaeyen JW, Onghena P, Goossens ME, Geilen M, Mulder H. Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain. 2005 Jan-Feb;21(1):9-17; discussion 69-72. doi: 10.1097/00002508-200501000-00002. PMID: 15599127.
- Cai L, Gao H, Xu H, Wang Y, Lyu P, Liu Y. Does a Program Based on Cognitive Behavioral Therapy Affect Kinesiophobia in Patients Following Total Knee Arthroplasty? A Randomized, Controlled Trial With a 6-Month Follow-Up. J Arthroplasty. 2018 Mar;33(3):704-710. doi: 10.1016/j.arth.2017.10.035. Epub 2017 Oct 28. PMID: 29239772.
- Nambi G, Abdelbasset WK, Alrawaili SM, Alsubaie SF, Abodonya AM, Saleh AK. Virtual reality or isokinetic training; its effect on pain, kinesiophobia and serum stress hormones in chronic low back pain: A randomized controlled trial. Technol Health Care. 2021;29(1):155-166. doi: 10.3233/THC-202301. PMID: 32831210.
- MKE Lundberg, Jorma S, Sven G. Carlsson. A Psychometric Evaluation of the Tampa Scale for Kinesiophobia — from a Physiotherapeutic Perspective. Physiotherapy Theory and Practice 20(2):121‑33. doi: 10.1080/09593980490453002.
- Black N, Murphy M, Lamping D, McKee M, Sanderson C, Askham J, Marteau T. Consensus development methods: a review of best practice in creating clinical guidelines. J Health Serv Res Policy. 1999 Oct;4(4):236-48. doi: 10.1177/135581969900400410. PMID: 10623041.
- Michael Quinn P. Qualitative Research & Evaluation Methods. 2002.
- Jünger S, Payne SA, Brine J, Radbruch L, Brearley SG. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat Med. 2017 Sep;31(8):684-706. doi: 10.1177/0269216317690685. Epub 2017 Feb 13. PMID: 28190381.
- Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, Wales PW. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014 Apr;67(4):401-9. doi: 10.1016/j.jclinepi.2013.12.002. PMID: 24581294.
- Gregg CD, McIntosh G, Hall H, Watson H, Williams D, Hoffman CW. The relationship between the Tampa Scale of Kinesiophobia and low back pain rehabilitation outcomes. Spine J. 2015 Dec 1;15(12):2466-71. doi: 10.1016/j.spinee.2015.08.018. Epub 2015 Aug 14. PMID: 26282104.
- Liu H, Huang L, Yang Z, Li H, Wang Z, Peng L. Fear of Movement/(Re)Injury: An Update to Descriptive Review of the Related Measures. Front Psychol. 2021 Jul 7;12:696762. doi: 10.3389/fpsyg.2021.696762. PMID: 34305755; PMCID: PMC8292789.
- Mintken PE, Cleland JA, Whitman JM, George SZ. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with shoulder pain. Arch Phys Med Rehabil. 2010 Jul;91(7):1128-36. doi: 10.1016/j.apmr.2010.04.009. PMID: 20599053.
- Swinkels-Meewisse EJ, Swinkels RA, Verbeek AL, Vlaeyen JW, Oostendorp RA. Psychometric properties of the Tampa Scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. 2003 Feb;8(1):29-36. doi: 10.1054/math.2002.0484. PMID: 12586559.
- George SZ, Zeppieri G. Physical therapy utilization of graded exposure for patients with low back pain. J Orthop Sports Phys Ther. 2009 Jul;39(7):496-505. doi: 10.2519/jospt.2009.2983. PMID: 19574658.
- Chand SP, DP Kuckel, Martin R. Huecker. Cognitive Behavior Therapy . in StatPearls. Treasure Island (FL): StatPearls Publishing. 2021.
- Monticone M, Cedraschi C, Ambrosini E, Rocca B, Fiorentini R, Restelli M, Gianola S, Ferrante S, Zanoli G, Moja L. Cognitive-behavioural treatment for subacute and chronic neck pain. Cochrane Database Syst Rev. 2015 May 26;2015(5):CD010664. doi: 10.1002/14651858.CD010664.pub2. PMID: 26006174; PMCID: PMC8922276.
- Stefanie T, Thomas H, Ehrenbrusthoff K. Effectiveness of additional cognitive behavioural interventions on pain, catastrophising, kinesiophobia and anxiety in people with whiplash-associated disorders compared to physiotherapy alone: A systematic review . Pain and Rehabilitation - the Journal of Physiotherapy Pain Association 2022(52):53‑81.
- Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. Graded exposure in vivo in the treatment of pain-related fear: a replicated single-case experimental design in four patients with chronic low back pain. Behav Res Ther. 2001 Feb;39(2):151-66. doi: 10.1016/s0005-7967(99)00174-6. PMID: 11153970.
- Woods MP, Asmundson GJG. Evaluating the efficacy of graded in vivo exposure for the treatment of fear in patients with chronic back pain: a randomized controlled clinical trial. Pain. 2008 Jun;136(3):271-280. doi: 10.1016/j.pain.2007.06.037. Epub 2007 Aug 22. PMID: 17716819.
- Araya-Quintanilla F, Gutiérrez-Espinoza H, Jesús Muñoz-Yanez M, Rubio-Oyarzún D, Cavero-Redondo I, Martínez-Vizcaino V, Álvarez-Bueno C. The Short-term Effect of Graded Motor Imagery on the Affective Components of Pain in Subjects with Chronic Shoulder Pain Syndrome: Open-Label Single-Arm Prospective Study. Pain Med. 2020 Oct 1;21(10):2496-2501. doi: 10.1093/pm/pnz364. PMID: 32003812.
- Bilterys T, Kregel J, Nijs J, Meeus M, Danneels L, Cagnie B, Van Looveren E, Malfliet A. Influence of education level on the effectiveness of pain neuroscience education: A secondary analysis of a randomized controlled trial. Musculoskelet Sci Pract. 2022 Feb;57:102494. doi: 10.1016/j.msksp.2021.102494. Epub 2021 Dec 15. PMID: 34953290.
- Burton AK, Waddell G, Tillotson KM, Summerton N. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine (Phila Pa 1976). 1999 Dec 1;24(23):2484-91. doi: 10.1097/00007632-199912010-00010. PMID: 10626311.
- Lorimer MG.Reconceptualising Pain According to Modern Pain Science. Physical Therapy Reviews 12(3):169‑78. 2007; doi: 10.1179/108331907X223010.
- Meeus M, Nijs J, Van Oosterwijck J, Van Alsenoy V, Truijen S. Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: a double-blind randomized controlled trial. Arch Phys Med Rehabil. 2010 Aug;91(8):1153-9. doi: 10.1016/j.apmr.2010.04.020. PMID: 20684894.
- Gül H, Erel S, Toraman NF. Physiotherapy combined with therapeutic neuroscience education versus physiotherapy alone for patients with chronic low back pain: A pilot, randomized-controlled trial. Turk J Phys Med Rehabil. 2021 Sep 1;67(3):283-290. doi: 10.5606/tftrd.2021.5556. PMID: 34870114; PMCID: PMC8606998.
- Huang J, Xu Y, Xuan R, Baker JS, Gu Y. A Mixed Comparison of Interventions for Kinesiophobia in Individuals with Musculoskeletal Pain: Systematic Review and Network Meta-Analysis. Front Psychol. 2022 Jun 29; 13:886015. doi: 10.3389/fpsyg.2022.886015. PMID: 35846681; PMCID: PMC9277051.
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996 Jan 13; 312(7023):71-2. doi: 10.1136/bmj.312.7023.71. PMID: 8555924; PMCID: PMC2349778.
- Pincus T, Smeets RJ, Simmonds MJ, Sullivan MJ. The fear avoidance model disentangled: improving the clinical utility of the fear avoidance model. Clin J Pain. 2010 Nov-Dec; 26(9):739-46. doi: 10.1097/AJP.0b013e3181f15d45. PMID: 20842017.