More Information
Submitted: February 09, 2021 | Approved: February 13, 2021 | Published: February 15, 2021
How to cite this article: Adhikari SP, Tretriluxana J, Dev R, Eglitis E, Shrestha N, et al. FITT-CORRECT: Updated dynamic and evidence-based principle of exercise prescription. J Nov Physiother Rehabil. 2021; 5: 005-009.
DOI: 10.29328/journal.jnpr.1001039
Copyright License: © 2021 Adhikari SP, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: FITT; FITT-CORRECT; Principle of EP; Clinical decision-making; Clinical reasoning
FITT-CORRECT: Updated dynamic and evidence-based principle of exercise prescription
Shambhu P Adhikari1*, Jarugool Tretriluxana2, Rubee Dev3, Emily Eglitis4, Nistha Shrestha5 and Cheryl Kerfeld6
1Department of Physiotherapy, School of Medical Sciences, Kathmandu University, Nepal
2Faculty of Physical Therapy, Mahidol University, Thailand
3School of Public Health, San Yat-sen University, China
4Physiotherapist, Australia
5Department of Physiotherapy, School of Medical Sciences, Kathmandu University, Nepal
6Seattle Public Schools, Seattle, Washington, USA
*Address for Correspondence: Shambhu Prasad Adhikari, PT, Ph.D., Department of Physiotherapy, School of Medical Sciences, Kathmandu University, Dhulikhel, Nepal, Tel: +977-9860801047; +977 11 490497; Email: [email protected]
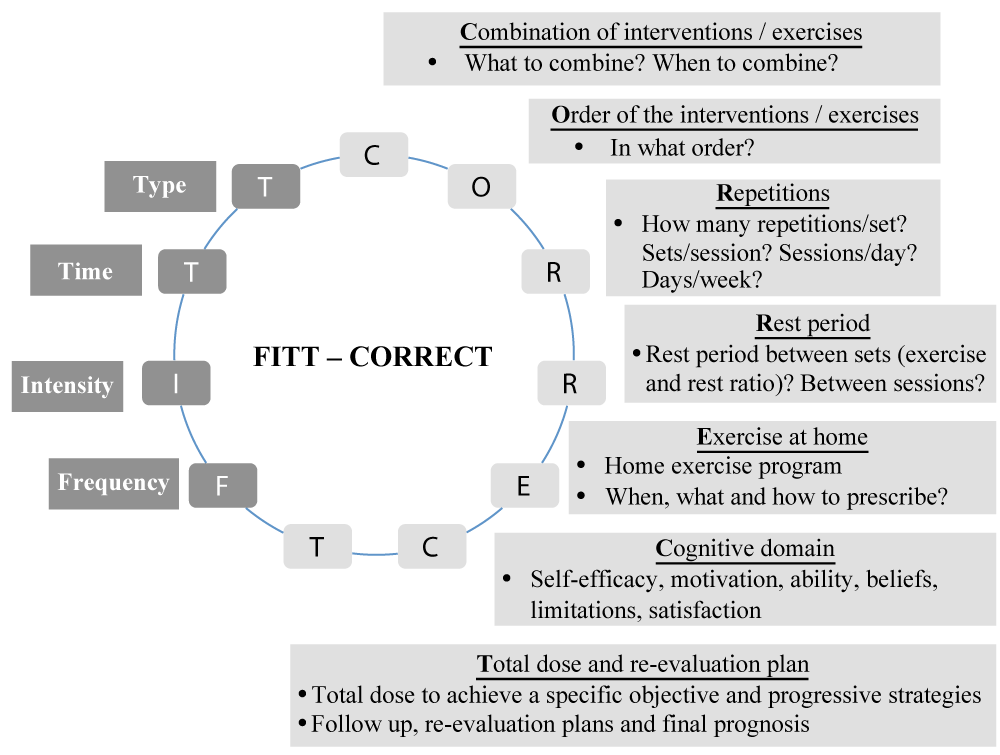
Objective: The FITT (Frequency, Intensity, Time, and Type) principle is an effective foundation in EP. However, the CORRECT components; C–Combination of interventions, O–Order of the Interventions, R–Repetitions, R–Rest period between sets and between sessions, E–Exercise at home, C–Cognitive domain, T–Total dose and re-evaluation plans, should be considered. The purpose of this paper was to describe the updated dynamic and evidence based FITT-CORRECT principle of EP and demonstrates its application using a case study.
Results: Literatures, related to EP, clinical reasoning and clinical decision-making, were critically reviewed. Established evidence is summarized to describe an updated dynamic and evidence-based principle of EP. The gaps within the FITT and other related principles of EP are addressed. The FITT-CORRECT principle was introduced and an effective outcome of the updated principle was demonstrated using a case study. The FITT-CORRECT principle integrates many components that are missing in the FITT and other related EP principles. Based on the reported case study, the FITT-CORRECT principle of EP should optimize patients’ intervention outcomes. Physiotherapists can potentially improve their EP by utilizing the FITT-CORRECT in clinical practice.
The principles of EP (EP) are intended for the development of individually tailored exercise programs [1]. The gold standard principle of EP derived by the American College of Sports Medicine (ACSM) is the FITT [Frequency (how often), Intensity (how much or how hard), Time (duration or how long), and Type (mode or what kind)] principle [2].
The fundamental principle of EP has been modified to FITT-VP in 2014 with the addition of Volume (amount) and Progression (advancement) [1]. Reid, et al. added a third ‘T’ introducing the FITT-T principle to address Timing of exercise [3]. Furthermore, the cognitive behavioral components are important but not included in FITT, for exercise adherence and behavioral change [1-4]. Ranasinghe, et al. derived FITTSBALL (“SBALL” - Stage of change, Belief and Ability of the client, Limitations and Life satisfaction) principle to address the missing cognitive behavioral component [4]. These multiple variations demonstrate the need for the many added components to be integrated into one all-encompassing principle.
While prescribing exercises based on the existing principles, there will be many unanswered questions as follows. Which interventions yield positive effect when two or more interventions are combined? Can any exercise be combined with any another exercise? What is the best order? With a combination of exercises, how are the parameters redefined? How do the number of repetitions, number of sets and number of sessions determine total duration? Should interventions be applied concurrently or simultaneously or with an interval period? How are duration and rest periods established? In an individually tailored prescription, how does one decide which exercise to be progressed and how? Is the rest period between exercises considered within the total duration? What should the total dose be to achieve the specific objectives? Are specific home exercise programs required? How to decide what home exercise programs are required and what will be their parameters? How to make sure that the home program will not interfere to that of the intervention administered at the clinic? How do we progress an exercise? Which parameter to be progressed first? What are the factors to be considered while progressing an exercise? What cognitive domain plays an important role to yield better intervention effect?
Usual parameters, described by the FITT principle, may not always be appropriate with different health conditions. Therefore, an updated dynamic and evidence-based principle of EP is needed to address the literature gaps.
A brief review
This brief review provides critical examination of the literature and integrates the existing evidence to educate the clinical practitioners to apply in their routine work. Literatures related to EP, clinical reasoning, clinical decision-making were critically reviewed and established evidence has been summarized to describe an updated dynamic and evidence-based principle of EP. The new principle of EP is expected to address the existing gaps in the literature.
Development of the FITT-CORRECT principle of EP
Based on various existing principles of EP, principles of neuroscience, motor control and learning, practice guidelines, evidence-based physiotherapy practice, experience and outcome of the various contemporary physiotherapy interventions, an updated dynamic and evidence-based principle of EP has been described. The term “CORRECT” has been coined to include all possible components supported by the evidence and that are not included in the original “FITT” principle.
The FITT-CORRECT principle integrates the original technical domains of FITT and added CORRECT components. The FITT-CORRECT principle has been introduced to address the gaps within FITT and its other related principles. The detail on FITT-CORRECT has been described in figure 1 and tables 1,2.
Figure 1: Components and description of the FITT-CORRECT principle of exercise prescription.
| Table 1: Definition of the terminology used in the text. | |
| Terms | Definition |
| Repetition of an exercise | Repetition of ‘one performance’ of a single exercise. |
| ‘Set’ of an exercise | A ‘set’ indicates group of repetitions performed without stopping. |
| Exercise: rest | Ratio of the performance and rest time. |
| Intervention | Either exercise or modality that is used in physiotherapy treatment. |
| Physiotherapist administered intervention | Interventions administered by the physiotherapist (it may be at the clinic – institution-based intervention and at patients’ home- community based intervention). |
| Home exercise intervention or programs | Exercise to be performed by the patients themselves or with the support of caregivers at their home. |
| Priming intervention | When two interventions are given at a time, the effect of second intervention is improved with the prior intervention. The prior or the first intervention is termed priming intervention. |
| Exercise volume | Total amount of exercise performed just in a single session. |
| Table 2: Description of the CORRECT components of FITT-CORRECT principle. | |
| Components | Description |
| C – Combination | When combining interventions, there should be established evidence for the combined effect and all of the influencing factors for interventions have to be considered in order to optimize therapeutic outcomes. One also needs to consider the order or sequence of exercises, which influences outcomes. One order of interventions may work positively whereas another may not. Therefore, evidence-based orders have to be followed. The order is usually decided based on the objective of the treatment, assessment of aberrant movement pattern, and the evidence for effectiveness of the selected intervention plan. |
| O – Order of interventions or exercises | |
| R – Repetitions | Interventions are usually applied repeatedly over time to drive neuroplasticity, tissue adaptation and lasting changes. The total duration described in the FITT principle does not clarify repetition within the sets. Varied number of repetitions yields various outcomes, which must be predetermined based on the objectives and evidence. Once the number of repetitions is determined, then the rest time between the sets, and the number of sets within a session must be decided. Number of repetitions, number of sets (sessions) and exercise-rest ratio can be entertained to meet individualized intervention parameters. Therefore, (repetitions x sets + rest time) x number of sessions = duration of the intervention per day. |
| R – Rest period between sets (exercise-rest ratio) and between sessions: | |
| E – Exercise at home (home exercise program (HEP)): | A patient can also be prescribed a HEP if the physiotherapist-administered intervention (PAI) has to be reinforced., This will work only if the HEP can be correctly carried out by the client or with the help of the caregiver. We need to make sure that there is high HEP adherence and it should not interfere with the PAI. The HEP parameters have to be tailored as per the evidence. If two exercises do not work well together, there might be interference instead of transference and ultimately a negative outcome instead of positive outcome. |
| C – Cognitive domain | Ranasinghe et al., in FITTSBALL principle (4) explained the importance of a cognitive domain using a case series. Winstein et al introduced the use of a cognitive domain during an accelerated skill acquisition program in which motivation was one of the key components. Another important component included self-determination; which consists of the self-analysis of ability and outcome, confidence level and self-drive during assessment and intervention (6). In current patient-centered treatment systems, a client’s active involvement in self-analysis and treatment planning is important. The client must be motivated to improve exercise adherence and behavioral changes. Their ability and beliefs as well as limitations must be considered. Intrinsic factors of the client such as motivation, determination and confidence influence the effectiveness of exercise interventions. Client satisfaction with the outcome is a key indicator of a successful intervention. |
| T – Total dose and re-evaluation plan | The final component in FITT-CORRECT is the total dose and reevaluation plan. Once all parameters have been decided through clinical reasoning, one must prescribe a total dose to achieve a specific outcome with a corresponding plan for re-evaluation of the intervention program. Re-evaluation allows progression and/or modification of the interventions to address issues that have arisen during the intervention administration and updated patient prognosis. In the FITT-CORRECT principle, the last ‘T’ of FITT has been redefined in such a way that it would represent all types of intervention or exercise or modalities rather than only mode of exercise. |
Demonstrating the use of the FITT-CORRECT principle of EP using a case study
Ms. K (name changed, informed written consent was taken) sustained a stroke one week ago and subsequently was unable to perform activities with her right dominant hand. Ms. K’s primary goal was to be able to use her right hand for her Activities of Daily Living (ADLs).
Using the FITT-CORRECT principle, a physiotherapist prescribed an exercise protocol for Ms. K. Based on the evidence, feasibility, appropriateness and patient’s need, the physiotherapist-administered intervention (PAI) called task-oriented training (TOT) was administered at the outpatient clinic. A drinking task was selected as per patient’s preference. This task was divided into components (reaching; reaching and grasping; reaching, grasping and lifting; reaching, grasping, lifting, transport) and trained in the order of their complexity (least to most complex).
The parameters and total dose of the TOT (30 minutes per session, once a day, six days a week for two weeks) was set as per motor control, learning and principles of exercise dependent neuroplasticity. Parameters were progressed based on patient’s performance level and ability. Distributed practice with a rest period whenever needed (indicated with reduced performance or compensatory movement or increased exertion) was adopted. Impairment mitigation strategies (training muscle function, improving range of motion, stretching tight muscles, proprioceptive neuromuscular stimulation, dexterity training) were integrated during the TOT and patient’s active involvement was encouraged.
Functional exercises were prescribed to do at home (HEP- Home Exercise Program) to enhance the effect of TOT. The ADLs such as eating fruit, drinking tea, and eating rice were advised to do three times a day for six days a week for two weeks using the affected hand. She was asked to take rest periods whenever required during the functional tasks. The functional tasks were then progressed to having her put on her eyeglasses and hairclips and combing her hair. The TOT was progressed in line with the progressively more difficult functional tasks through client-therapist collaboration. The exercise adherence for the two weeks was excellent (9/10 in the form of visual analogue scale).
Application of the dynamic FITT-CORRECT principle resulted in a detectable change within two weeks. The motor function improved from 35/66 to 54/66 on Fugl Meyer Assessment (FMA), wrist and finger flexion-extension improved from partial (some flexion; 1/2 and ability to release active mass flexion grasp; 1/2) to full (complete active flexion; 2/2 and full active extension, 2/2), strength improved to almost normal (able to do test-related functions independently) and she could eat, put on hair clips and bands using her affected hand independently, which was not possible before the treatment. However, each component of FMA-upper extremity-specific evaluation and interventions induced changes have to be explored during large-scaled studies.
The improvement in Ms. K’s upper extremity function supports the use of an appropriate combination of task-oriented and functional training. The parameters and total dose were set as per motor control, learning and principles of exercise dependent neuroplasticity. The cognitive domains has been integrated during task collaboration (for task selection), task analysis (finding problems to do the task), self-assessment and management [6].
Ms. K was asked to attend clinic-based therapy sessions in order to receive TOT, which had to be administered by a skilled physiotherapist. A HEP was provided to Ms. K to enhance the effect of the PAI thereby yielding better outcomes. Sequential progression of the interventions and parameters [6], existed for both the PAI and HEP. A re-evaluation was performed after achieving our target goal at the completion of the total dose. The strategies adopted in the treatment of this patient were as per FITT-CORRECT principle that resulted in a detectable positive change and outcome within two weeks.
The FITT-CORRECT principle integrates many components that are missing in the FITT and other related EP principles. Based on the reported case study, the FITT-CORRECT principle of EP should optimize patients’ intervention outcomes. Physiotherapy providers can potentially improve their EP in their clinical practice by utilizing the FITT_CORRECT principle.
While combining, those interventions, which yield positive effect and have established evidence, can only be combined with the consideration of other influencing factors. During the combination, the order of the interventions makes a difference. For example, while combining endurance and strength training, if gaining endurance is the main objective, endurance training should be performed first. If gaining strength is the main objective, strengthening exercises should be performed first [8,9]. The priming interventions should always be administered first [10]. For example, the motor preparation biases visual processing during motor-visual combination whereas visual events enhance motor activation during visuo-motor combination [11]. In addition, congruency versus in-congruency between two interventions produces completely opposite outcomes. Therefore, having an appropriate order between combined interventions is of vital importance [12]. The order of interventions not only influences the effectiveness, safety and efficacy but also influence the parameters of each intervention [8,13,14].
Induction of plasticity or long term change in function requires sufficient repetitions [15]. Research has shown a range of 3 to 50 repetitions per set of exercises in individually tailored prescription is successful in producing a change [16]. Repetitions, however, should not be considered alone. It also depends on the number of sets and exercise-rest ratio. For example, one-minute rest between sets may suit a set of fewer repetitions when compared to a three-minute rest between sets to accommodate the effort of a higher number of repetitions [14,17].
If acquisition of skills is to be enhanced, the rest period should be kept as short as possible [6,7]. If fatigue level is to be reduced, the rest period has to be relatively longer [7]. The total intervention duration is calculated based on the number of repetitions within sets, number of sets, exercise-rest ratio and number of sessions per day. This total duration per day is different than the exercise volume used in previous literature [18]. The time of self–analysis during the intervention is included within the total duration whereas the time of outcome assessment should not be included [7].
When therapists administer PAI and provide HEPs, the interventions should not interfere with each other. As Kleim and Jones mentioned in their principle, we look for transference rather than interference effect [15]. If any PAI is to be performed at home, the treatment should be reproducible. The HEP should be such that the exercise adherence level is high and protocol reinforces PAI [16].
The integration of cognitive domain in the evaluation, analysis, as well as in treatment, not only improves treatment outcome but also enhances exercise adherence and reinforces behavioral change [4,6]. Adhikari, et al. in 2018 [7] demonstrated an enhanced effect of an intervention and significant improvement in the self-efficacy level by encouraging clients’ active involvement and integrating motivational strategies. These were evidence to show importance of consideration of cognitive domain in prescribing exercises.
Therapeutic interventions must be prescribed in terms of dosage. The total intervention dose should be adjusted according to the patient’s pathology, relevant medical conditions, and their individual needs and goals. Other contextual factors also influence total dose, which is directly associated with the effect size [19,20]. The total dose should be devised by specifying the desired therapeutic outcome for individuals considering all influencing factors. Therapists further need to consider intervention – response and/or dose response effect, fatigue and nutritional level, motivation and ability, family and caregiver’s support, resources required while dealing with each intervention and/or parameter of the interventions [7,18].
Re-evaluation of the intervention effect must be planned from the beginning to progress, modify or change the prescription (either intervention or the parameters) to meet the evolving needs of the patient. Re-evaluation may be done during the intervention programs or after certain interval follow-ups. An exercise progression model given by Broody and team is the best evidence to progress interventions and/or parameters [18].
Finally, therapists must consider holistically the patient’s pathological factors (e.g. lesion type, side, size, location, severity, duration, comorbidities), personal factors (e.g. age, body size, gender, habits), and socio-environmental factors (home and workplace demands and requirements) when determining intervention prescription [18].
The FITT principle is a foundation principle in EP, which is still used today. The FITT-CORRECT principle enhances and integrates many components that were lacking in the original FITT and other related principles. The FITT-CORRECT principle assists therapists to work within the evidence based practice guidelines. Using the FITT-CORRECT requires critical clinical decision-making that considers patients’ needs, clinician skill, current evidence and context.
Though the updated principle was based on the established principles and evidence, we conducted just a brief review, which is a limitation of this study. A validation of the updated principle is warranted. The effectiveness of the intervention was evaluated through a case study. The outcome of present case study would provide preliminary information and therefore, clinical trials should be conducted to establish interventions effectiveness for its application in the clinical practice.
We would like to express our sincere gratitude to the participant without whom conduction of the case study would not have been possible.
Declarations
Consent to participate: The participant in our study cannot be identified in any way in the manuscript. A written informed consent was obtained from the participant and the caregiver prior to the recruitment.
Consent to publish: A written informed consent was obtained from the participant and the caregiver prior to the recruitment to publish or disseminate the outcome of the case study.
Availability of data and materials: Any information regarding the present study can be available from the first author up on reasonable request.
Authors’ contributions: All authors (SPA, JT, RD, EE, NS, CK) contributed to the preparation of this manuscript. SPA led the conception and design of the study. SPA and CK prepared the first draft of the manuscript. SPA participated in revising and finalizing the draft of the manuscript by critically revising the important intellectual content. SPA conducted the case study. All authors contributed in describing the case and writing the discussion. All authors read and approved the final version of the manuscript.
- Riebe D. editor. General Principles of EP ACSM's Guidelines for Exercise Testing and Prescription. 9th ed: Wolters Kluwer/Lippincott Williams & Wilkins; 2014. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4139760/
- ACSM, editor. Guidelines for exercise testing and prescription. 8th ed: Philadelphia: Lippincott Williams & Wilkins; ; 2010.
- Reid RER, Thivel D, Mathieu ME. Understanding the Potential Contribution of a Third "T" to FITT EP: The Case of Timing in Exercise for Obesity and Cardiometabolic Management in Children. Appl Physiol Nutr Metab. 2019.
- Ranasinghe C, King NA, Arena R, Hills AP. FITTSBALL - a dynamic tool for supervision of clinical EP. Disabil Rehabil. 2019: 41: 3216-3226. PubMed: https://pubmed.ncbi.nlm.nih.gov/30053786/
- Billinger SA, Boyne P, Coughenour E, Dunning K, Mattlage A. Does aerobic exercise and the FITT principle fit into stroke recovery? Curr Neurol Neurosci Rep. 2015; 15: 519. PubMed: https://pubmed.ncbi.nlm.nih.gov/25475494/
- Winstein C, Lewthwaite R, Blanton SR, Wolf LB, Wishart L. Infusing motor learning research into neurorehabilitation practice: a historical perspective with case exemplar from the accelerated skill acquisition program. J Neurol Phys Ther. 2014; 38: 190-200. PubMed: https://pubmed.ncbi.nlm.nih.gov/24828523/
- Adhikari SP, Tretriluxana J, Chaiyawat P, Jalayondeja C. Enhanced Upper Extremity Functions with a Single Session of Action-Observation-Execution and Accelerated Skill Acquisition Program in Subacute Stroke. Stroke Res Treat. 2018; 2018: 1490692.
- Inoue DS, Panissa VL, Monteiro PA, Gerosa-Neto J, Rossi FE, et al. Immunometabolic Responses to Concurrent Training: The Effects of Exercise Order in Recreational Weightlifters. J Strength Cond Res. 2016; 30: 1960-1967. PubMed: https://pubmed.ncbi.nlm.nih.gov/26626027/
- Jones TW, Howatson G, Russell M, French DN. Effects of strength and endurance exercise order on endocrine responses to concurrent training. Eur J Sport Sci. 2017;17: 326-334. PubMed: https://pubmed.ncbi.nlm.nih.gov/27817246/
- Stoykov ME, Madhavan S. Motor priming in neurorehabilitation. J Neurol Phys Ther. 2015; 39: 33-42. PubMed: https://pubmed.ncbi.nlm.nih.gov/25415551/
- Nedelko V, Hassa T, Hamzei F, Weiller C, Binkofski F, et al. Age-independent activation in areas of the mirror neuron system during action observation and action imagery. A fMRI study. Restor Neurol Neurosci. 2010; 28: 737-747. PubMed: https://pubmed.ncbi.nlm.nih.gov/21209489/
- Celnik P, Webster B, Glasser DM, Cohen LG. Effects of action observation on physical training after stroke. Stroke. 2008; 39: 1814-1820. PubMed: https://pubmed.ncbi.nlm.nih.gov/18403746/
- Simao R, Figueiredo T, Leite RD, Jansen A, Willardson JM. Influence of exercise order on repetition performance during low-intensity resistance exercise. Res Sports Med. 2012; 20: 263-273. PubMed: https://pubmed.ncbi.nlm.nih.gov/22742079/
- Simao R, de Salles BF, Figueiredo T, Dias I, Willardson JM. Exercise order in resistance training. Sports Med. 2012; 42: 251-265. PubMed: https://pubmed.ncbi.nlm.nih.gov/22292516/
- Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008; 51: S225-239. PubMed: https://pubmed.ncbi.nlm.nih.gov/18230848/
- Szalewska D, Zielinski P, Tomaszewski J, Kusiak-Kaczmarek M, Lepska L, et al. Effects of outpatient followed by home-based telemonitored cardiac rehabilitation in patients with coronary artery disease. Kardiol Pol. 2015; 73: 1101-1107. PubMed: https://pubmed.ncbi.nlm.nih.gov/25987401/
- Williams MA, Haskell WL, Ades PA, Amsterdam EA, Bittner V, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007; 116: 572-584. PubMed: https://pubmed.ncbi.nlm.nih.gov/17638929/
- Brody LT. Effective therapeutic EP: the right exercise at the right dose. J Hand Ther. 2012; 25: 220-231.
- Young JL, Rhon DI, de Zoete RMJ, Cleland JA, Snodgrass SJ. The influence of dosing on effect size of exercise therapy for musculoskeletal foot and ankle disorders: a systematic review. Braz J Phys Ther. 2018; 22: 20-32. PubMed: https://pubmed.ncbi.nlm.nih.gov/29157736/
- Young JL, Rhon DI, Cleland JA, Snodgrass SJ. The Influence of Exercise Dosing on Outcomes in Patients With Knee Disorders: A Systematic Review. J Orthop Sports Phys Ther. 2018; 48: 146-161. PubMed: https://pubmed.ncbi.nlm.nih.gov/29320945/