More Information
Submitted: 23 May 2020 | Approved: 05 June 2020 | Published: 08 June 2020
How to cite this article: Thiruvarangan S, Srigrishna P, Thileebphan B. A trial of Cnservative care for restoring scapular dyskinesis: A clinical series. J Nov Physiother Rehabil. 2020; 4: 011-015.
DOI:10.29328/journal.jnpr.1001031
Copyright License: © 2020 Thiruvarangan S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Scapular dyskinesis; Conservative approach; Scapular algorithm
Abbreviations: VAS: Visual Analog Scale; DASH: Disabilities of the Arm, Shoulder and Hand; ROM: Range Of Motion; MMT: Manual Muscle Testing; SLAP: Superior Labrum Anterior and Posterior; SAT: Scapular Assistance Test; SRT: Scapular Retraction Testc
A trial of conservative care for restoring scapular dyskinesis: A clinical series
S Thiruvarangan1*, P Srigrishna2 and B Thileebphan3
1Clinical Physiotherapist, Department of Physical Medicine, Base Hospital, Mulankavil, Killinochi, Sri Lanka
2Consultant Orthopaedic Surgeon, Teaching Hospital, Jaffna, Sri Lanka
3Registrar in Orthopaedics, National Hospital, Sri Lanka
*Address for Correspondence: S Thiruvarangan, BSc.PT (SL), FDOSR (UK), Clinical Physiotherapist, Department of Physical Medicine, Base Hospital, Mulankavil, Killinochi, Sri Lanka, Tel: +94778470824; Email: [email protected]
The shoulder is the greatest movable joint in the human body. Its anatomical design allows a wide range of motion in all directions, leading to an insubstantial balance between stability and mobility. Conservative treatments are suggested by a number of authors for restoring the scapular dyskinesis. However, this condition can be overlapped by other clinical findings. Therefore, comprehensively analysing individual biomechanical rationale is central to design the ideal rehabilitation regimen to overcome scapular dyskinesis by restoring the scapular thoracic rhythm and preventing the associated problems. This study presents a brief clinical series of three patients with shoulder pain due to the alteration of their scapulahumeral rhythm and highlights a comprehensive examination and follow up an evidence-based rehabilitation algorithm to regain pain free functional ability in daily routine life.
Shoulder pain is a very common complaint in general medical practice. A study reported that one-third of the population suffers from shoulder symptoms during their lifetime and it is associated with a negative impact on both personal and national levels. Moreover, it decreases the quality of life due to personal suffering and subsequent economic impact on health care services. The resultant cost and work absence associated with shoulder pain are a social concern [1]. The incidence of shoulder pain in general medical practice increases with age and peaks at 45 to 64 years of age, however, various age groups experience shoulder pain. It depends on the subject’s work-related activities and recreational sports that involve upper extremity repetitive motion [2]. The condition ‘Scapular dyskinesis’ refers to changes of the normal static or dynamic position of the scapula and alteration of coupled scapulohumeral movements [3]. Scapular dyskinesis is not necessarily a pathological term, because it can be found not only in symptomatic shoulder regions but also in asymptomatic patients. It is suggested that scapular dyskinesia contributes more often in symptomatic shoulder pain and has been shown to be a predictive factor in developing other associated problems such as shoulder impingement and adhesive capsulitis [4]. The purpose of this article is to describe common musculoskeletal alteration of complex shoulder anatomy and biomechanics leading to pathomechanics and clinical characteristics of the scapular dyskinesia as well as explaining how to perform a precise musculoskeletal examination and how to apply conservative interventions that can be easily incorporated into the scope of physical therapist practice to achieve successful outcomes in scapular dyskinesis.
Case 1
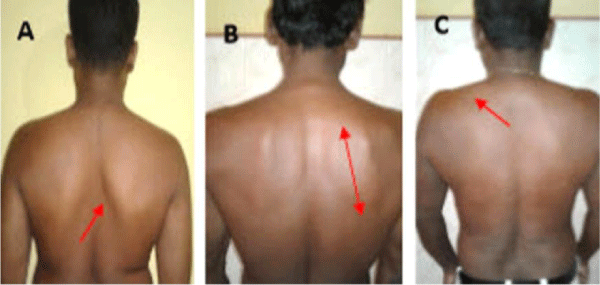
A 29 year old man presented with pain in his right shoulder for about one month, he had no history of trauma to right upper limb but he had been performing weight training exercise over the last six months. The pain was getting worse and interrupting his day to day activities (Figure 1A).
Case 2
A 58 year old male, whose occupation involved repetitive sailing and vigorous drawing physical activities. He complained of right shoulder pain over the last eight months, which had a gradual onset, with none history of previous trauma, however symptoms were gradually worsening (Figure 1B).
Case 3
A 46 year old moderate manual male worker was referred to our clinic with complaints of progressive worsening of pain in the left shoulder, for the past four months, with none history of trauma or comorbidities. The onset of pain was insidious; lasted for several hours, when it was triggered by lying on the left side, reaching overhead in day to day activities and lifting with the left arm (Figure 1C).
Figure 1: Scapular dyskinesis classification A: Type I, B: Type II, C: Type III.
Aetiology
Postural abnormality eventually develops cervical lordosis or disproportionate thoracic kyphosis, changing the typical resting position of the scapula resulting in increasing protraction and acromial depression [5]. The most identified origin of scapular dyskinesia is due to muscular imbalance between the shoulder girdle agonist and antagonist muscles. This leads to shoulder girdle’s anatomical positional changes and alteration of scapular movements’ coordination [6]. In few cases, anatomical disruption due to clavicular fractures or resections can shorten or angulate the position of the clavicle disturbing the quality of scapula humeral rhythm, since the posterior clavicular rotation allows the initial and final 30° of overhead motions. In addition to that, contractures of the pectoralis major can restrict posterior clavicular motion. Moreover, acromioclavicular joint injuries and acromial morphology can cause abnormal scapula humeral rhythmic motion. Pectoralis minor or short head of biceps muscular contracture can anteriorly move the scapula over the top of the thorax due to their attachments to the coracoid process. Lack of capsular flexibility, especially of the posterior capsule prevents anterior and superior translation of the humeral head and loss of internal rotation to cause scapular dyskinesis [7].
History
The main cause of shoulder pain among scapular dyskinesis subjects is an alteration of the scapular anatomical position due to rotator cuff dysfunction that consequently leads to subacromial impingement syndrome along with pain and stiffness. The pain can be quite severe on abduction and internal rotation of the glenohumeral joint and last for several hours as dull pain. The shoulder pain from musculoskeletal disorders is most often described as insidious neither any previously reported trauma nor history of radiating symptoms along the upper extremity of the affected shoulder. In a significant number of symptomatic scapula dyskinesia, subjects may complain of pain in the anterior and/or the posterior-superior aspect of the shoulder region, surrounding the deltoid tuberosity and intermittent pain along the upper trapezius. The pain is triggered by reaching and lifting in overhead functional activities.
Classification patterns
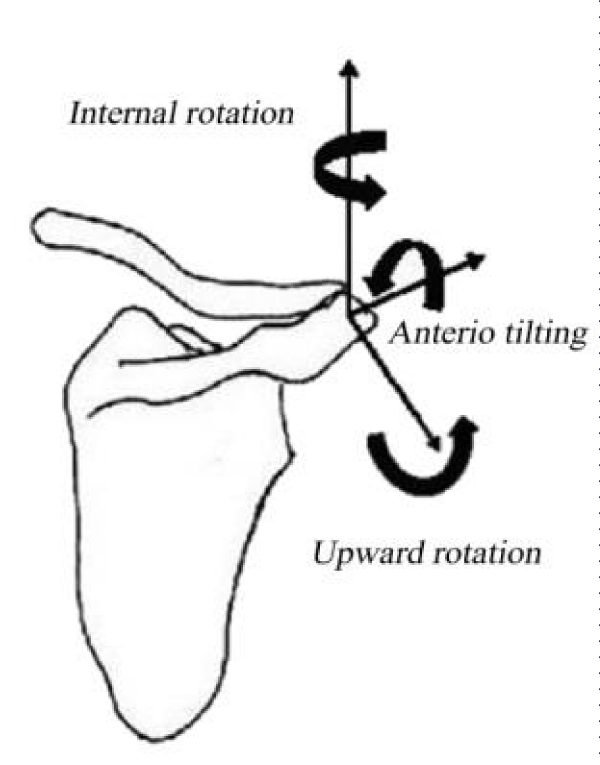
The shoulder region pain should be observed from posterior to anterior view in anatomical position to investigate the pattern of scapula dyskinesis. It is generally noticed, when the subject shows one or more abnormal positions of the scapula compared to the sound side (Figure 2). It is classified into three dyskinesia patterns [8]. Type I is characterized when at rest, the inferior angle of the scapula may be prominent dorsally and during arm motion, the inferior angle tilts dorsally and the acromion tilts anteriorly over the top of the thorax. The axis of the rotation is in the horizontal plane (Figure 1A). Type II is described at rest, the entire medial border may be prominent posteriorly and during arm motion, the medial scapular border tilts dorsally off the thorax. The axis of the rotation is vertical in the frontal plane (Figure 1B). Type III displays at rest, the superior border of the scapula may be elevated and the scapula can also be dorsally displaced and during arm movement, a shoulder shrug initiates movement. The axis of this motion occurs in the sagittal plane (Figure 1C).Figure 2: Biomechanical scapular alteration.
Associated problems
Scapular dyskinesis is a widespread term used to label the loss of scapulohumeral rhythmic motion. A number of shoulder pathological conditions may result from abnormal scapular motion. Subacromial impingement syndrome is the most commonly associated problem with scapular dyskinesia. It occurs when soft tissues such as supraspinatus, long head of biceps brachii tendon, subacromial bursa and superior joint capsule are impinged in the subacromial space. Symptoms involving shoulder impingement can turn into functional impairments in the chronic term. In addition to that, adhesive capsulitis and SLAP lesion can be developed among overlooked or poor scapular dyskinesis rehabilitation [9].
Biomechanical concepts
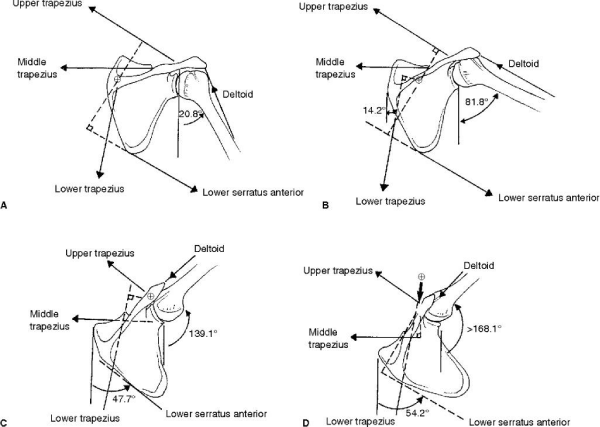
The biomechanical analysing of the shoulder accentuates the coordinated motion of four joints: glenohumeral, scapulothoracic, sternoclavicular, and acromioclavicular. Any full range of shoulder joint movement is brought by contributing all four joints’ play motion [10]. This joint movement is described as arthrokinematics, which contain rolling, spinning, and sliding in different directions at the joint surfaces according to their concurrent articular surfaces [11]. Ideal joint play motion occurs only in the availability of normal periarticular connective tissue, integrity, extensibility and tension relationship muscles function [12]. Static stability is built up from glenoid labrum, joint capsule, glenohumeral ligaments and intrinsic negative pressure of the joint. Dynamic stabilizers include rotator cuff muscles, long head of the biceps tendon and other scapulothoracic muscles such as pectoralis major, rhomboid, latismusdorsi and serratus anterior [13] (Figure 3). The rotator cuff muscles provide dynamic stability to the humeral head onto the glenoid fossa, forming a force couple with the deltoid to allow elevation of the arm. This force couple provides about 45% of the abduction strength and 90% of the external rotation strength [14]. A stiff shoulder presents inadequate capsular flexibility and altered muscle function, therefore the clinicians should treat the connective tissue extensibility and restore normal muscle function in order to re-establish harmonious glenohumeral movements within the shoulder complex [15].
Figure 3: Force couples for scapular rotation [16].
Physical examination
After gaining the medical history, a comprehensive physical examination should be carried out. Ideally the patient needs to wear appropriate clothes to be thoroughly assessed by a systemic approach. It includes observing posture, soft-tissue inspection, palpation, ROM, strength testing, neurological assessment and applying high clinical value (sensitive and specificity) special shoulder tests [17]. The initial examination is accomplished by observing posterior to anterior view posture, specifically the shoulder region at plumb line standing position at rest. Next, the evaluation of the affected arm quality of joint motion is done by asking the subject to perform overhead shoulder motion in ascending and descending phases to observe the scapular motion; deviations are typically noticed in the descending phase with eccentric muscle loading. One of the three patterns of dyskinesia can be found by comparing the contralateral scapula. Then consistency of the sternoclavicular and acromioclavicular joints needs to be evaluated and clavicle examination should be done to identify any angulation. Following that, the coracoid process should be investigated to determine its position by comparing the sound side and possible tenderness on its medial border where the pectoralis minor inserts. In the existence of scapular dyskinesis, it may present with other pathological conditions such as subacromial impingement syndrome, rotator cuff tear and SLAP lesion [18]. Two corrective manoeuvres can be performed to check the kinematic alterations and understand whether these manoeuvres normalize the arm motion and reduces the patient’s symptoms [19]. Firstly, the scapular assistance test (SAT), the clinician supports the scapula into an upward rotation in coronal plane by pushing upward and laterally on the inferior angle and posterior tilt in the sagittal plane by pulling the superior aspect of the scapula while the patient is performing humeral elevation. If there is relief of symptoms and increased motion, the test is positive, since the SAT increases the subacromial space and is helpful in detecting the scapular contribution to impingement and rotator cuff dysfunction. Secondly, scapular retraction test (SRT), the clinician first measures the supraspinatus muscle strength by using the empty can position for arm elevation then repeats the test meanwhile stabilizing the medial border of scapula. If the pain decreases and arm elevation increases, the test is positive. It is also useful to perform the scapular load test to take measurements from a fixed vertebral landmark to the medial border of scapula in three different levels for calculating muscular demand [20]. Pain, muscle strength and quality of functional assessment would be measured by VAS, MMT and DASH tool respectively. These evaluating tools may help to follow up the documentation in regard to the patient progress while participating in a rehabilitation programme.
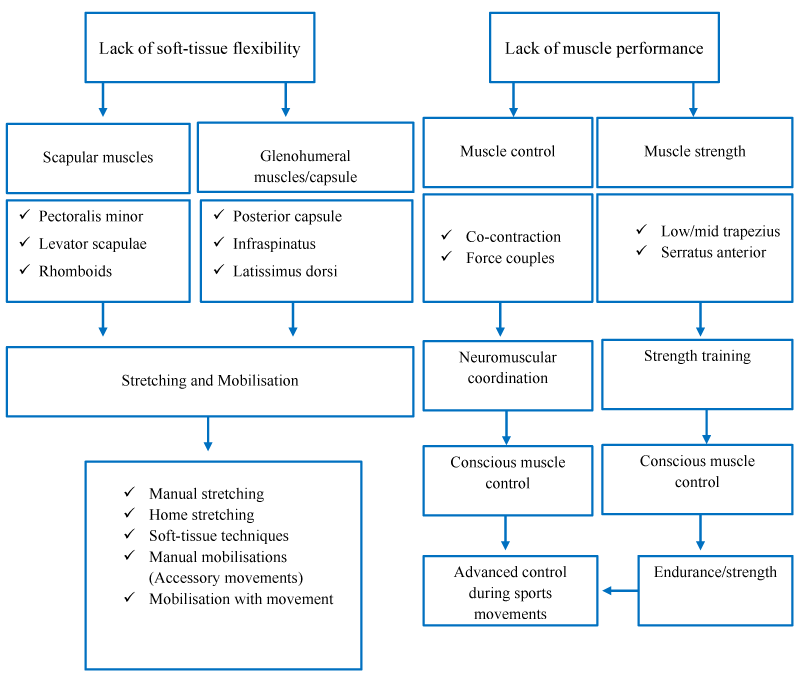
Scapular rehabilitation algorithm
The goal of the scapular dyskinesis rehabilitation regimen is restoring the scapular muscular imbalance and abnormal glenohumeral rhythm. The scapular dyskinesis takes in a higher activation of the upper trapezius and levator scapulae muscle, and simultaneously, a decreased switch of the middle and lower trapezius and serratous anterior muscles [21]. The objective is ensuring the balance ratio between the three parts of the trapezius. Cools, et al. recommend an algorithm, which includes a set of four exercises (prone extension, side lying external rotation, side lying forward flexion and prone horizontal abduction with external rotation). This probably encourages high activation of the middle and lower trapezius. Other exercises such as wall slide, push-up exercises and shoulder elevation in the scapular plane specifically improve the activation of the serratous anterior, furthermore these exercises minimize the activation of upper trapezius and levator scapulae [22]. Also the rehabilitation regimen contains exercises that aim to stretch the posterior capsule and the pectoralis major and minor muscles (Figure 4). The posterior capsule needs to be stretched in a side lying position with internal rotation, abduction of arm with elbow at 90° and pectoralis muscles stretching in the supine arm and elbow at 90° horizontal abducted position by pushing the shoulder posteriorly. A number studies emphasise that not only the middle and lower trapezius but also the rotator cuff muscles need to be strengthened with progressive resistance after adequate stabilization of the scapula under the physiotherapist’s supervision [23]. The majority of subjects capable to understand the exercises, which move the scapula to facilitate posterior tilt and upward rotation after attending a few supervised physiotherapy sessions and follow them without the assistance of the therapist [24].
Figure 4: Scapular dyskinesis rehabilitation algorithm [22].
Prognosis
The rehabilitation of scapula dyskinesis must follow comprehensive clinical evaluation based on the individual’s perspective for achieving better outcomes. Therefore, we have applied the scapular rehabilitation algorithm therapeutic interventions to our three types of scapular dyskinesia patients as per their clinical evaluation. Approximately, after 6-8 weeks follow up, all subject felt less pain and suffering in their day to day activities, VAS and DASH scores significantly improved.
This article highlights the positive outcomes of scapular dyskinesis by following a conservative management approach which focuses on the precise diagnosis and a standardized rehabilitation algorithm according to the individual biomechanical analysis to regain pain free activity of day life.
Ethical consideration
This study included all three patient’s informed written consent were received prior to involvement of this clinical study.
The authors wish to thank, Adriana Cruz-Banares who provided the proofreading services in the final stage of the manuscript submission process in regard to gain the potential language level.
- Feleusa MA, Bierma-Zeinstraa HS, Miedemab MD, Bernsena AN, Verhaard BW, et al. Department of General Practice Manual Therapy. 2008; 13: 426–433.
- Greving K. Incidence, prevalence, and consultation rates of shoulder complaints in general practice. Scand J Rheumatol.. 2012; 41: 150-155. PubMed: https://pubmed.ncbi.nlm.nih.gov/21936616
- Sciascia, AD. Clinical implications of scapular dyskinesis in shoulder injury: the consensus statement from the “Scapular Summit”. Br J Sports Med. 2013; 47: 877–885. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23580420
- Seitz AL, Mc Clure PW, Lynch SS, Ketchum JM, et al. Effects of scapular dyskinesis and scapular assistance test on subacromial space during static arm elevation. J Shoulder Elbow Surg. 2012; 21: 631-640. PubMed: https://pubmed.ncbi.nlm.nih.gov/21444218
- Smith R, Nyquist-Battie C, Clark M, Rains J. Anatomical Characteristics of the Upper Serratus Anterior: Cadaver Dissection. J Orthop Sports Phys Ther. 2003; 33: 449-453. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12968858
- Edward R, Laskowski ER, Newcomer-Aney K, Smith J. Refining Rehabilitation with Proprioception Training: Expediting Return to Play. Phys Med Rehabil Clin N Am. 1997; 25. PubMed: https://pubmed.ncbi.nlm.nih.gov/2008686
- Tyler TF, Nicholas SJ, Roy T, Gleim GW. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2000; 28: 668-673. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11032222
- Kibler W. Sciascia, A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010; 44: 300–305. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19996329
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003; 19: 641-661. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12861203
- Kent BE. Functional anatomy of the shoulder complex, a review. Phys Ther. 1971; 51: 867-887. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/4997967
- Warwick R. Williams P. Gray’s Anatomy, 35th British Ed. Philadelphia: WB Saunders Co. 1973; 399-407.
- Sarrafian SK. Gross and functional anatomy of the shoulder. Clin Orthop. 1983; 19: 173: 11-19. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/6825322
- Kapanji IA. Upper Limb. New York. Churchill Livingstone, The Physiology of the Joints. 1970; 24-76.
- Evans PJ, Maniac A. Rotator cuff tendinopathy many causes, many solutions. J Musculo Med. 1997; 14: 47-61.
- Soslowsky LJ, Carpenter JE, Bucchieri JS, Flatow EL. Biomechanics of the rotator cuff. Orthop Clin of North Am. 1997; 28: 17-30. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9024428
- Miniaci A, Salonen D. Rotator cuff evaluation: Imaging and diagnosis. Orthop Clin of North Am. 1997; 28: 43-58. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9024430
- Postacchini R, Carbone S. Scapular dyskinesis: Diagnosis and treatment. OA Musculoskeletal Medicine. 2013; 18: 20.
- Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2013; 11: 142-151. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12670140
- Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998; 26: 325-337. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9548131
- Rubin BD, Kibler WB. Fundamental principles of shoulder rehabilitation: conservative to postoperative management. Arthroscopy. 2002; 18: 29-39. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12426529
- Russ P, Michael LV. The role of the scapula. Int J Sports Phys Ther. 2013; 8: 617–629. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3811730/
- Cools AM, Dewitte V, Lanszweert F, Notebaert D, Roets A, Soetens B. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007; 35: 1744-1751. PubMed: https://pubmed.ncbi.nlm.nih.gov/17606671
- Cricchio M, Frazer C. Scapulothoracic and scapulohumeral exercises: a narrative review of electromyographic studies. J Hand Ther. 2011; 24: 322-333. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21820276
- Mottram SL, Woledge RC, Morrissey D. Motion analysis study of a scapular orientation exercise and subjects’ ability to learn the exercise. Man Ther. 2009; 14: 13-18. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17910930
- McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2008; 10: 269–277. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11408911