Research Article
Postural and Kynematic effect of a new custom-made foot insole called “Prodynamic” in a cohort of patients affected by extrapiramidal disease

Maurizio Falso1*, Matilde Grillo2, Anna Righetti2, Franco Lopa3, Lisa Rocco3 and Emanuela Facchi2
1Middle Cares Rehabilitation Unit, Madonna del Corlo Foundation, Lonato (Bs), Italy
2Middle Cares Rehabilitation Unit, Richiedei Foundation, Gussago (Bs), Italy
3Ortopedia Signori, Desenzano d / G, Italy
*Address for Correspondence: Maurizio Falso, MD, Physical Medicine and Rehabilitation, Middle Cares Rehabilitation Unit, Madonna del Corlo Foundation, Corso Garibaldi 3, 25017, Lonato (Bs), Italy, Tel: 349.4971729; Email: [email protected]
Dates: Submitted: 16 April 2019; Approved: 22 May 2019; Published: 23 May 2019
How to cite this article: Falso M, Grillo M, Righetti A, Lopa F, Rocco L, et al. Postural and Kynematic effect of a new custom-made foot insole called “Prodynamic” in a cohort of patients affected by extrapiramidal disease. J Nov Physiother Rehabil. 2019; 3: 039-081. DOI: 10.29328/journal.jnpr.1001027
Copyright License: © 2019 Falso M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Foot-insole; Parkinson; Parkinsonism; static and dynamic postural and gait control; baropodometry
Abbreviations: P: Parkinson’s disease; PS: Parkinsonism; VPA: Visual Postural Analysis; VGA: Visual Gait Analysis; BBS: Berg Balance Scale; FW: Free Walk; MMSE: Mini Mental State Examination; AP: Anterior-Posterior; LL: Latero-lateral; COP: Centre Of Pressure
Abstract
Background: The use of a custom-made orthotic plantar device is referenced as a true sensor-motor facilitation tool for the control of the postural orthostatic and orthodynamic position in patients with Parkinson’s disease.
Aim: To outline the postural and kinematic effect of a pro-ergonomic multilayer foot insole versus a custom-made carbon-kevlar dynamic foot insole in a cohort of patients affected by extrapyramidal disease.
Setting: A rehabilitation institute for the treatment of neurological and orthopaedic gait disorders.
Methods: A sample of 8 patients (mean age of 82.6), of whom 4 affected by Parkinson’s disease (P) and 4 by Parkinsonism (PS) were recruited for the aim of this study. In line with our inclusion criteria (clinical-functional diagnosis of Parkinson’s disease or Parkinsonism, Webster scale ≤ 20, Mini-mental State Examination (MMSE) ≥ 18), the study design developed in 2 times:
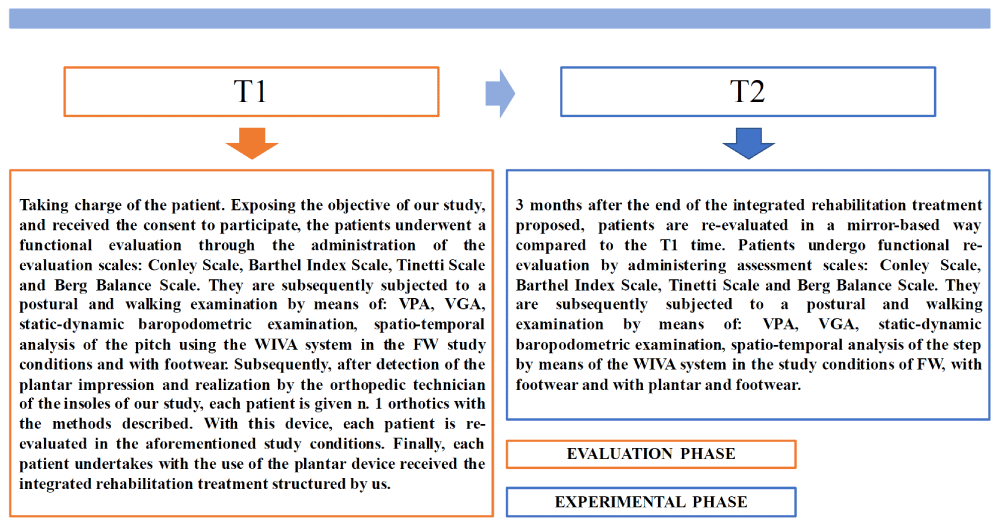
a. time T1 (or evaluation time), in which recruited patients affected by Parkinson’s disease or Parkinsonism were evaluated at the Hospital and Noble Resting House Paolo Richiedei through an accurate functional (Conley scale, Barthel Index scale, Tinetti scale and the Berg Balance Scale), postural evaluation (VPA) and walking examination (VGA, baropodometric evaluation, kinematic gait evaluation through WIVA system); to each group of patients of our study were therefore entrusted 4 foot-insoles, of which 2 synthetic and 2 carbon-kevlar custom-made foot-insoles called PRODYNAMIC; at the end of this step, patients started with our integrated rehabilitative treatment course.
b. time T2 (or experimental time; 90 days from T1), a new clinical-instrumental evaluation of each patient was performed, repeating the clinical-functional and instrumental evaluation performed at the time T1 in a specular way; this assessment was performed in FW condition, with personal footwear and previously acquired foot-insoles used during the evaluation at the T1 time.
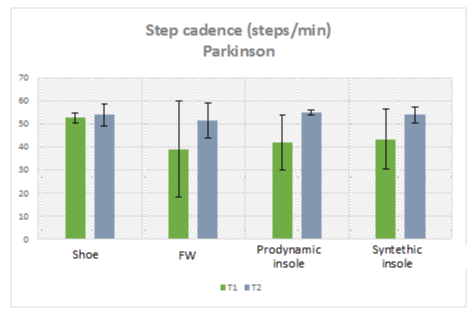
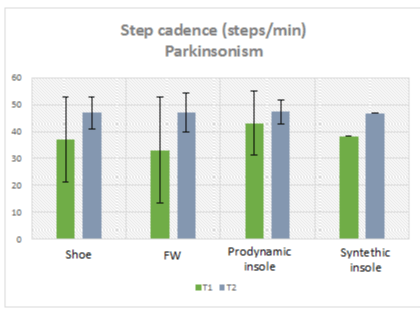
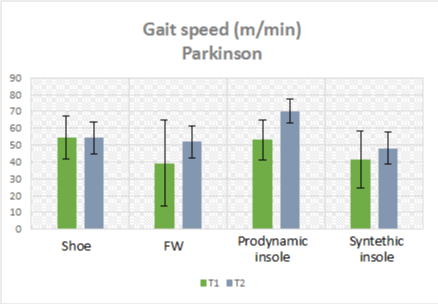
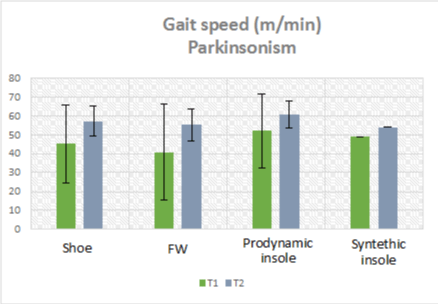
Results: Most of our patients have been able to find benefit from the use of the plantar orthosis and integrated rehabilitation treatment so as to bring some modifications within personal postural attitude, recording an improvement but not uniform change within the sample. The results obtained by comparing the VPA at time T1 and at time T2 explain how patients affected by both clinical forms tend to establish incorrect postural attitudes due to stiffness and appearance of hypertonic plasticity, which become then structured and only partially modifiable. There was a general performance improvement in line with the VGA: within the P.B group, we observed with the use of the Prodynamic insole a partial or even complete normalization of the dynamic heel-contact phase, a better alignment of the COP in its excursion from the 1st to the 2nd rocker phase of the step, a notable facilitation to the inertial thrust in progress in the 3rd and 4th rocker phase, an improvement in the eccentric control of the patellofemoral alignment in the acceptance phase of the so-called load-response in stance and, finally, the acquisition of a more physiological propulsion structure of the trunk basin unit with an improvement of the clearance and fixation skills in the sequential phases of the step. This trend was evident but not uniform in the other groups considered. Analysis of the evolution of the degree of functionality in the daily life activities expressed by the Barthel index, passing from time T1 to the time T2, showed an improvement and consistent change in all groups considered within our study that we can find in a more or less way for the other clinical outcome data. An objective time-related and intra-group comparison of the raw static and dynamic baropodometric data acquired in our 4 study conditions showed different time-related trends for the two groups taken into consideration. A specific WIVA profile was found for each pathology group, highlighting different trends passing from time T1 to time T2 in particular of the gait cadence and gait speed. In particular, in the “Prodynamic” study condition the gait cadence shows in the Parkinson group a significant increase from time T1 to time T2, passing respectively from an average value of 41.9 ± 11.7 to 54.9 ± 1.1; patients of the Parkinsonism group showed a value of the average gait cadence at time T1 higher than the other study conditions at the same evaluation time, with an increase of this data from T1 to T2, passing from 43.1 ± 11.8 to 47.4 ± 4.4. If we consider the gait speed time-related trend, in the “Prodynamic” study condition at T1 the gait speed in Parkinson patients is similar to that recorded in the “shoe” study condition; in Parkinsonism the gait speed recorded at time T1 is higher than that recorded in the other study conditions; at time T2 there is a less evident increase in speed compared to that observed in patients with Parkinson’s.
Conclusion: In today’s management of the profile of complexity of extrapyramidal pathology, the association of several health figures is of fundamental importance, with professional profiles and diversified skills, in such a way as to be able to guarantee a comprehensive management of the patient. From this point of view, the figure of the orthopedic technician will be able to play a new role within the rehabilitation team, which will be responsible for the best possible functional response (deriving from an optimal integration between orthotic and rehabilitation treatment) of patients with Parkinson’s disease.
Introduction
Extrapyramidal syndrome is one of the most frequent chronic-progressive diseases in the population between 55 and 89 years of age [1,2]. The definition of this syndrome underlies a series of movement disorders that find common denominator in an alteration of the extrapyramidal system and its components responsible for regulating the postural adjustments that accompany the voluntary movement. From a pathophysiological and etiopathogenic point of view, patients with extrapyramidal syndrome can be classified as patients with Parkinson’s disease or Parkinsonism [3-6].
For both conditions, the incidence rate increases with age, with a slightly higher risk for males and for females and with a rather homogeneous geographical distribution [7-9]. It goes from a total prevalence (every 100 in-habitants) of 0.9%, between individuals between the ages of 65 and 69, to 5.1%, between those aged between 85 and 89 for parkinsonism, with a consensual overall prevalence from 0.6 to 3.5% for Parkinson’s disease [10-13].
The clinical manifestations that correlate Parkinson’s with Parkinsonism, make it difficult to formulate a correct and immediate diagnosis. The orthostatic and orthodynamic postural instability would seem to be a real demonstration and constant confirmation in the framing of the Parkinsonian patient, representing the expression of an altered sensor-motor integration of the afferent and efferent nerve information, responsible for processing the reactions postural support of each patient. The progressive impairment of the central nervous systems responsible for the control of the balance is the main cause of disability in Parkinsonian patients, exposing them to a high risk of falling and influencing his quality of life.
In this sense, the impact of the motor and a psychosocial impairment appears to be very important: “the extrapyramidal patient has a greater fear of falling than a healthy individual of the same age” and remains influenced to such an extent that it is conditioned negatively in his daily life and in the restriction of participation in contextual relations activities with the milieu [14-16].
Distinguished by a syndromic picture with a high degree of complexity (resulting from the association of motor, cognitive and psychological symptoms), the Parkinsonian patient requires global care, for which he appears completely anachronistic not entrusting him to the co-management of a multidisciplinary team. In this perspective, the figure of the physiotherapist stands out, as the promoter of a suitable lifestyle and as the true creator of an individualized rehabilitation path of multitask management of the complex Parkinsonian syndromic picture. Some studies have shown that the extrapyramidal patient typically slows down during the course of his life a reduced activation of orthostatic and orthodynamic support postural responses both in feedback and in feedforward as well as an intrinsic difficulty in performing tasks in “dual-task performance” [17-20]. Alterations in the sensor-motor control of these functions appear to be irrefutable at present with studies that over the years have wanted to highlight the fundamental role that in this context may have orthostatic and orthodynamic plantigrade support of a Parkinsonian patient [16,21,22].
With this in mind, the studies by Jenkins ME et al. [12], and of Qui F et al. [16], wanted to highlight the importance of sensorimotor stimulation of the sole of the foot as a tool for the afferent remodulation of the control strategies of patient’s antigravity support reactions. The use of a custom-made orthotic plantar device is referenced by them as a true sensor-motor facilitation tool for the control of the postural orthostatic and orthodynamic position in the patient with Parkinson’s disease. In both studies the results obtained, were compared with the use of a conventional slab and those obtained with the use of a custom-made foot-insole facilitator; the data suggest that the use of a facilitating insole can be considered a low-cost and effective treatment strategy for optimizing the postural responses and gait of the patient suffering from Parkinson disease, providing evidence on the role that the somatosensory system plays in the instauration of the postural instability of patient which, however, has not been observed in Parkinsonism. Similarly, Lirani-Silva E. et al. [21], observed in their pilot study how the continuous use of textured insoles for one week benefits plantar sensation and gait in patients with PD. Their results underlinded the hypothesis that enhanced somatosensory feedback to the sensory system result in an improved motor output of gait in patients affected by PD.
None of these studies has clearly delineated the effects of the different foot-insole materials on the kinematic gait parameters nor the specific use of carbon as a device able to influence the quality of the step and the orthodynamic stability in patients with PD.
The aim of this study was to outline the postural and kinematic effect of a pro-ergonomic multilayer foot insole versus a custom-made carbon-kevlar dynamic foot-insole in a cohort of patients affected by extrapyramidal disease.
Materials and Methods
Participants
In line with our inclusion and exclusion criteria, we selected a sample of 8 patients, of whom 4 affected by Parkinson’s disease (P) and 4 by Parkinsonism (PS), at the Hospital and Rest Home Paolo Richiedei of Gussago. The age of our patients varied between 72 and 91 years, with a mean age of 82.6yy (+/− 5.4). Table 1 summarizes the profile of our sample, recruited in March 2018, with acquisition of personal data, such as age, gender, weight, height, footwear number and diagnosis of Parkinson’s or Parkinsonism, obtained at the time of taking in charge of each. Patients were recruited after a physiatric assessment and underwriting of the informed consent for participation in the study. Recruited patients did not require the law by an internal or external hospital ethics committee, given the non-bloody nature of the proposed study model. In order to make the study sample as homogeneous as possible in its characteristics, we have adopted inclusion and exclusion criteria in the selection of our patients.
| Table 1: Analytical sample description (from own elaboration). | ||||||
| Paziente | Gender | Age | Weight (kg) | Height (cm) | Footwear number | Parkinson (P) or Parkinsonism (PS) |
| A.B. | F | 84 | 52 | 158 | 38 | P |
| L.S. | M | 72 | 85 | 170 | 40 | PS |
| M.S | F | 83 | 79 | 163 | 37 | P |
| F.S | M | 79 | 66 | 175 | 43 | P |
| L.V. | F | 83 | 60 | 155 | 37 | PS |
| M.U. | M | 84 | 73 | 171 | 40 | PS |
| G.I. | M | 91 | 78 | 178 | 41 | PS |
| R.I. | F | 85 | 59 | 160 | 38 | P |
Inclusion criteria
• Clinical-functional diagnosis of Parkinson’s disease or Parkinsonism;
• Webster scale ≤ 20;
• Mini-mental State Examination (MMSE) ≥ 18.
Exclusion criteria• Clinical-functional diagnosis not compatible with Parkinson’s disease or Parkinsonism;
• Webster scale ≥ 21;
• Mini-mental State Examination (MMSE) <18
Study design and outcome measures
The study design (Figure 1) developed in 2 times:
Time T1 (evaluation time): recruited patients affected by Parkinson’s disease (P) or Parkinsonism (PS) were evaluated at the Hospital and Noble Resting House Paolo Richiedei through an accurate functional (Conley scale, Barthel Index scale, Tinetti scale and the Berg Balance Scale), postural evaluation (VPA) and walking examination (VGA, baropodometric evaluation, kinematic gait evaluation through WIVA system), first in free-walk (FW) and subsequently with personal footwear; to each group of patients of our study were therefore randomly delivered 4 foot-insoles, of which 2 synthetic and 2 carbon-kevlar custom-made foot-insoles called PRODYNAMIC; at the end of this step, patients started with our integrated rehabilitative treatment course.
Time T2 (experimental time): after 3 months (90 days from the time T1), a new specular clinical-instrumental evaluation of each patient was performed; this assessment was performed in FW condition, with personal footwear and previously acquired foot-insoles used during the evaluation at the T1 time.
Functional and instrumental outcome measures
Outcome measures considered valid for the clinical-functional and instrumental monitoring of the integrated orthopedic-rehabilitation treatment proposed by us on the recruited patients were as follows:
• Visual Postural Analysis (VPA)
• Visual Gait Analysis (VGA)
• Functional scales
- Conley Scale, for the assessment of the risk falling
- Barthel Index Scale, for the evaluation of autonomy in daily life activities
- Tinetti Scale, for the evaluation of balance and gait
- Berg Balance Scale, for the evaluation of equilibrium reactions
• Baropodometric items
- Static load response percentage (%)
- Average static pressure (Kpa)
- Surface static plantar support (cm2)
- Dynamic step total area (cm2)
- Orthodynamic step duration (m/sec)
• WIVA system kynematic items
- Gait speed (m/sec)
- Gait cadence (steps/min)
- Stride length (% cycle lenght)
- Stance phase duration on the right and left (% cycle)
- Swing phase duration on the right and left (% cycle)
- Double gait support duration (% cycle)
Study devices and evaluation procedures
• Visual gait analysis
Visual Gait Analysis is an assessment tool that allows us to evaluate the quality of the gait pattern and the patient’s gait through a visual reference. The possible alterations of the gait cycle, analyzed through observation, allow the acquisition of specific data of our interest, such as: the quality of the ground support, the quality of the stance phase and the push-off phase, the dynamic assessment of knees and trunk-pelvic unit and, finally, the quality of the orthomorphism plantar attitude. These parameters, obtained during the first evaluation at time T1, were compared with similar data, obtained at time T2 according to the same procedures, in order to evaluate the effectiveness of the device. Patients under examination underwent at time T1 and time T2 to an objective evaluation of the analytical gait pattern with footwear and with a synthetic and a Prodynamic foot-insole, focus our attention on:
- profile of the heel contact phase on the right and left side;
- profile of the stance phase of the step on the right and left side;
- profile of the biomechanical knee functional excursion bilaterally;
- profile of the hip-trunk unit attitude.
• Visual postural analysis
In our study we used the Visual Postural Analysis, as a tool for assessing the postural attitude of each patient, in order to evaluate any changes made by the use of the orthotic device and integrated rehabilitative treatment. Through this evaluation it is possible to identify postural attitudes and defects of each patient, realizing a snapshot of what is the initial postural attitude (time T1) of each patient by using personal footwear compared with the respective data recorded during the final evaluation with foot insoles and personal footwear (time T2). Recruited patients were subjected at T1 time and T2 to an objective evaluation of trunk postural assessment in toto in anterior-posterior and latero-lateral position, with footwear and with synthetic foot insole and the Prodynamic insole, focusing attention on:
- shoulder and right and left hip alignment (in AP);
- degree of symmetry and/or asymmetry of the so-called size triangles (in AP);
- alignment of the head-neck-trunk unit (in AP);
- assessment of the orthostatic plantigrade support at rest (in AP);
- alignment of cervical lordosis, dorsal kyphosis and lumbar lordosis (in LL).
• Baropodometry
The bardopodometric examination is presented as a device capable of objectifying and quantifying the extent and modality of the plantar support, in term of ground reaction pressure analysis of patient’s static or dynamic foot print. For the purposes of our study we used the EPS + R baropodometric platform of LORAN ENGINEERING (Figure 2).
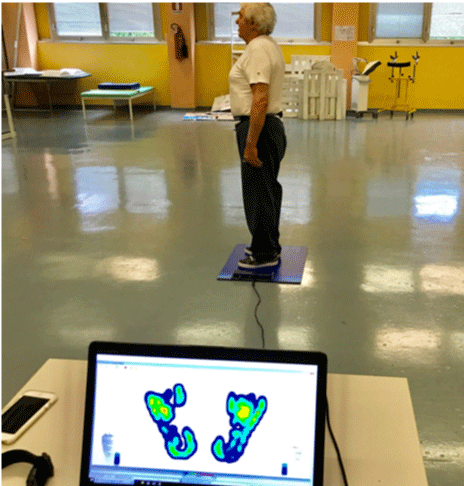
The device uses a computerized system of orthostatic and dynamic analysis of the single foot and can also be used for indirect analysis of patient’s postural alignment. EPS + R is easy to transport and little influenced in acquiring the baropodometric data from environmental factors. From the procedural point of view and in line with the design of our study, each patient under examination was invited to position himself on the baropodometric platform, with his arms at his body sides (Figure 3); the patient is asked to look at a fixed point in front of the horizon and to remain still for 1 minute.
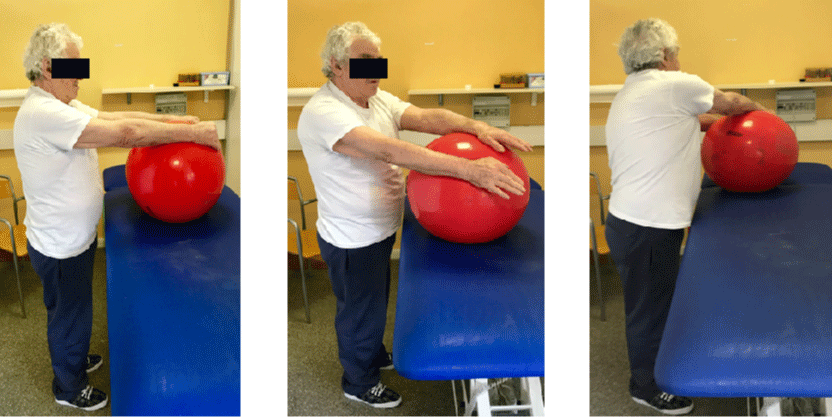
Figure 3: Patient’s postural assessment during the baropodometric data acquisition in orthostatic condition (from own elaboration).
In this orthostatic condition 3 data of our interest will be acquired:
- right and left average plantar pressure
- right and left percentage of plantar load
- right and left plantar surface support
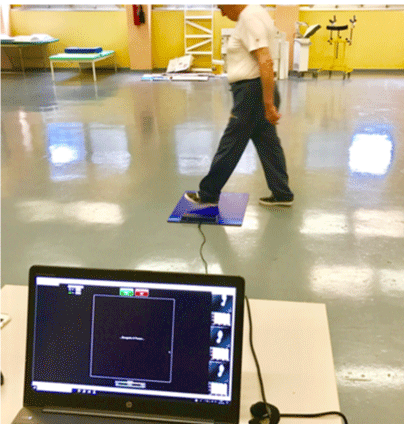
Acquired these static baropodometric data, patient was taken down from the platform and positioned at a distance of about 5 meters from it; each patient (Figure 4) was therefore required to walk on and step on it in orthodynamic monopodal support, continuing the path for another 5 meters passing the platform.
Figure 4: Patient’s orthodynamic assessment during the baropodometric data acquisition (from own elaboration).
At the end of the path, patient will be asked to re-execute this procedure trampling the platform with the contralateral foot during the unconditional walk required; the walking procedure will be repeated for about 30 seconds in order to allow us to acquire the orthodynamic load on the platform with both feet. In this test condition 3 data of our interest will be acquired:
- duration of the right and left step;
- orthodynamic right and left plantar pressure;
- total area of the right and left step in orthodynamic condition.
This evaluation was carried out at time T1 in free-walk and with personal footwear and secondary with a synthetic/PRODYNAMIC foot-insole and footwear, and at the time T2 in free-walk, with synthetic/PRODYNAMIC foot-insole and suitable footwear, and personal footwear without an insole.
• WIVA system
WIVA system sensor consists in a simple device that allowes a quick and simple measurement of spatio-temporal gait parameters. The WIVA sensor is a wireless device (Figure 5) consisting of: a. triaxial accelerometer; b. Triaxial gyroscope; c. Magnetometer.
The WIVA sensor is able to communicate with the software of our computer using a Bluetooth connection. The spatio-temporal data, acquired with this device, represent the result of a software comparison with normative data well-known and still defined for each gait parameter. For the aim of this procedure, the device will be positioned on level L5 of patient’s spine and secured by an ergonomic belt allowing free body movement.
In each of our study condition, each patient is instructed to walk with the WIVA system applied on the lumbar region at a spontaneous but constant walking speed, a linear path of 10 meters going, 10 meters in return and again 10 meters outward, for total distance of 30 meters. Spatio-temporal indicators considered valid for our assessment of the path are:
- Gait speed (m/sec)
- Gait cadence (steps/min)
- Stride length (% cycle length)
- Stance phase duration on the right and left (% cycle)
- Swing phase duration on the right and left (% cycle)
- Double gait support duration (% cycle)
This evaluation was performed at the time T1 in free-walk and with personal footwear, with synthetic/ PRODYNAMIC foot-insoles and at the time T2 in free-walk, with synthetic/PRODYNAMIC foot-insoles, and with personal footwear without the use of the device.
• Foot-insole device
For the purposes of our study we used 2 different orthotic insoles (synthetic and PRODYNAMIC foot-insole); each of them has different technical characteristics (Table 2) and different manufacturing procedures.
| Table 2: Comparison of the technical and functional characteristics of a synthetic and PRODYNAMIC foot-insole (own elaboration). | ||
| Structural properties | Synthetic foot-insole | PRODYNAMIC foot-insole |
| Basic building material | EVA | CARBON-KEVLAR |
| Coating material | EVA | EVA |
| Consistency | + DUCTILE - ELASTIC |
- DUCTILE + ELASTIC |
| Enough under dynamic load | LOW | HIGH |
| Prodynamic facilitation and step modulation | LOW | HIGH |
| Production speed | HIGH | LOW |
• Traditional semi-finished foot-insole in synthetic material
The synthetic insole used (Figure 6) is a simple semi-finished foot-insole with a facilitating support for the arched vault; it is a prefabricated foot-insole (NOT CUSTOM-MADE) and once the measure suitable for the patient has been identified, it will be adapted to patient’s plantar orthomorphism.
Having identified the anthropometric correspondence with the length of the patient’s foot, the device in raw form is milled; in this way the foot-insole in raw form will acquire a thickness lower than the initial cast and with a shape compatible with that of patient’s footwear. At the base of the shaped foot-insole (Figure 7) thicknesses or pins facilitating the pronation or supination of the backfoot and therefore of the plantar helix can be inserted.
• PRODYNAMIC custom-made foot-insole in carbon-kevlar material
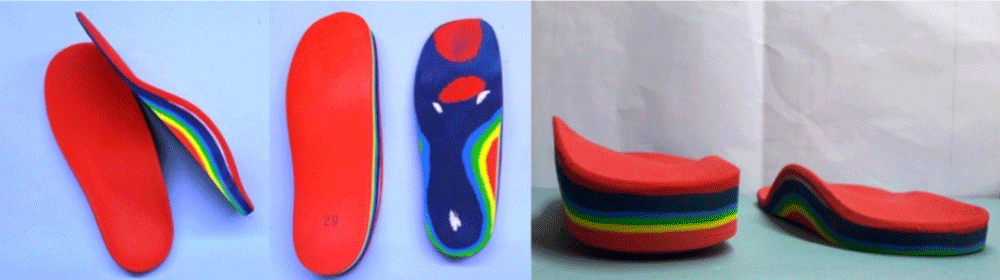
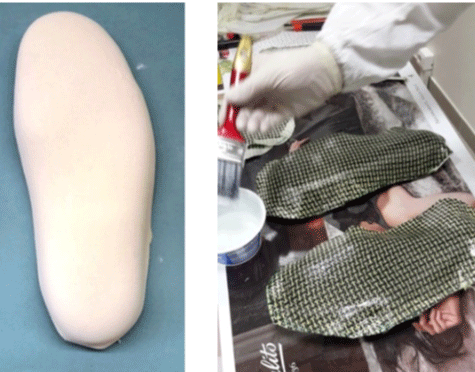
The foot orthosis, which we call PRODYNAMIC (to emphasize the intrinsic properties of dynamic facilitation of the gait step), can be framed as an innovative type of custom-made foot-insole (Figure 7a) and not of semi-finished origin, consisting of a body of 2mm thick carbon-kevlar (made from a positive plaster previously made on patient’s plantar footprint and functionally adapted according to medical indications to the purposes to which it will be responsible; this goal can be achieved through insertions of so-called “foot-pins” for pronation/supination facilitation and/or plantar inversion/eversion with a consensual greater or lesser anticipation of the retrometatarsal stopping), covered by a basal multilayer support and by EVA on the surface. The modality of acquisition of the plaster cast, the extraordinary adaptability to the anthropometric and functional characteristics of the foot, as well as the perfect alchemy of interaction in force between the materials that make it, make it a unique product of its kind.
Figure 7a: Multidirectional and plurisegmental framing of the finished PRODYNAMIC footbed (from own elaboration).
The manufacturing of a PRODYNAMIC foot-insole consists of 10 well-defined sequential steps that are unique in their kind.
STEP 1
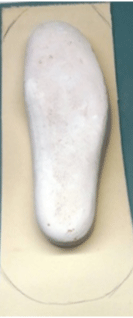
Step 1 begins with the acquisition of the plaster cast from the impression obtained with phenolic foam (Figure 8a); after having worked it with the addition of the necessary corrections, the technician selects the material to be used as the basis for the orthosis. The manual changes and corrections, made by the orthopedic technician before proceeding with the realization of the carbon kevlar shell, consist of the creation of thrust and containment areas aimed at the physiological alignment of the hindfoot and correct dynamic excursion of the center of pressure of the foot (COP) as well as absolute respect for the anthropometry of patient’s foot.
Figure 8a,b: Method of acquisition of the plantar mold using phenolic foam and EVA plate image and positive of the detected plaster (from own elaboration).
In the image the plaster cast is visible, after processing and next to it a sheet of EVA that will form the base of the foot insole (Figure 8b).
EVA plate image and positive of the detected plaster (from own elaboration).
STEP 2
The base material (EVA plate) (Figure 9) is cut out, overflowing from the plaster mold, to allow the subsequent appropriate wrapping.
The image presented in figure 10 shows the successful cutting of the EVA sheet, the angles of which will subsequently be beveled in order to allow a better wrapping of the plaster cast; the final product that will be obtained (wrapping EVA sheet and cast plaster cast) is now ready to be placed in a preheated oven for about 40 seconds.
STEP 3
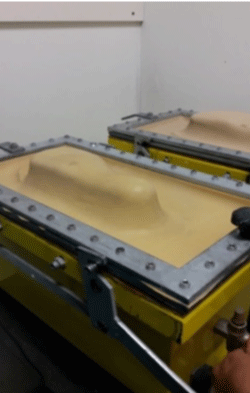
After being heated, the processing material (EVA) is more ductile and soft, becoming ready for thermoforming: the basal layer is placed on the plaster mold, previously positioned inside the vacum (Figure 11).
STEP 4
The positioning of the mold covered in the vacuum allows us to place it in a vacuum condition (Figure 12), a condition that will allow its thermoforming; the material is left in the machine for about 5 minutes and, once cooled, the vacuum is opened with extraction of the resulting product.
STEP 5
Figure 13 shows the result of the thermoforming; in it, the edges of the base layer will be lowered and thinned with the use of the cutter; this process will allow us to obtain greater adherence between the raw product and the gypsum shape.
STEP 6
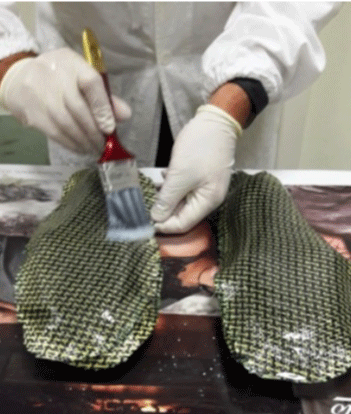
Once the base layer has been obtained, the corresponding and overlapping cropping of a sheet of carbon-kevlar fabric is carried out; this material consists of strands of carbon woven with aramidic threads (Figure 14). This type of fabric allows to obtain laminates with excellent mechanical qualities, rigidity and impact resistance. The resin is the fundamental component that promotes the hardening of carbon-kevlar. Before its use, the chosen resin, consisting of two components, is mixed; in this mixing operation no errors must be made on the dose of the two components; a minimum calibration error of the dosages would cause a lack of hardening of the carbon-kevlar shell that will be realized.
Figure 14: Thermoformed EVA on plaster cast and positioning of the first layer in kevlar-carbon (from own elaboration).
STEP 7
The mixture thus made of resin is applied by means of a brush (Figure 15) on the carbon-kevlar surface affixed to the plaster cast; this part of the processing must be carried out at temperatures not lower than 8°C; in the processing; 2 sheets of fabric are used for gypsum to obtain a more resistant and long-lasting body.
Figure 15: Application of the resin after the second application of the kevlar-carbon layer (from own elaboration).
STEP 8
Once the second layer of fabric has been applied and impregnated with resin, a sheet of pvc is placed on top of it. The material and the form are placed in the vacum (Figure 16), inside which the material is pressed; thanks to the vacuum that is created, all the possible formations of air bubbles, that can compromise the correct realization and final conformation, are thus avoided. To obtain complete hardening of carbon-kevlar, it is necessary to wait 5 hours.
STEP 9
After at least 5 hours of the hardening phase, the vacum is opened. The final product that will be obtained is a carbon-kevlar shell which, after being milled, is glued to the base layer previously made of EVA (Figure 17) and placed again in the vacum.
STEP 10
Once the base layer of the carbon-kevlar shell is joined, a 1cm thick material is glued (UNI 10902 density 0.23 kg/dm3, ISO 7619 40/50 Shore A hardness) which will give stability to the plantar orthosis. On this last layer of material, the plan is made. In the image, the prodynamic plantar is terminated in all its components (Figure 18).
• Technical-functional comparison profile between PRODYNAMIC foot-insole with carbon and PRODYNAMIC foot-insole with carbon-kevlar shell.
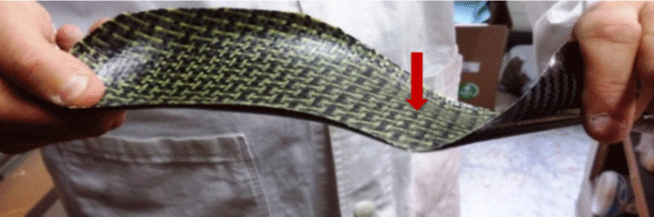
In the following images are compared two different materials, useful to realize a PRODYNAMIC foot-insole: carbon and carbon-kevlar. The point indicated by the arrow in figure 19, is the point of greatest load, at that exact point the material is a twist (torsion-wing) that in the pushing phase reaches its maximum level.
Figure 19: Carbon shell only with indication of the torsion wing at the head of the metatarsal head and of the structural elasticity in torsion of the body (from own elaboration).
The difference is visible; the carbon shell is more rigid and this lack of elasticity favors the break if the material is subjected to a constant weight and torsion. The advantage of carbon-kevlar is the greater elasticity despite the strength of the material (Figure 20). This aspect avoids the breaking of the same body, consequently it increases the duration of the use of the plantar orthosis.
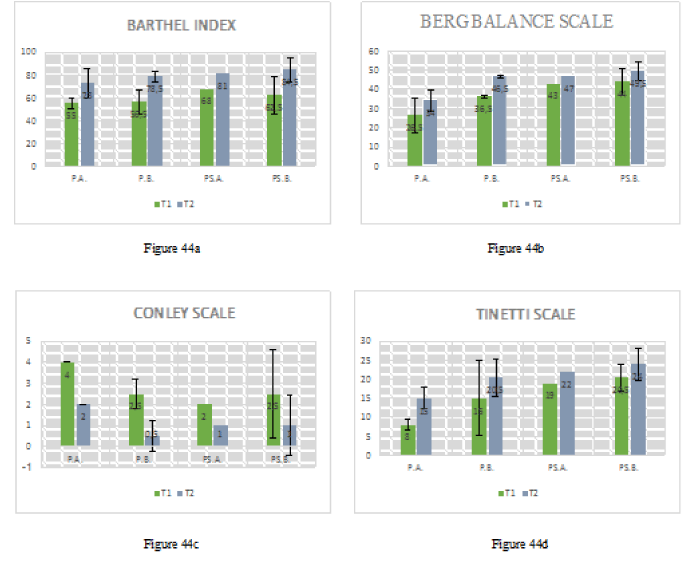
Integrated rehabilitative treatment protocol: Patients of our study sample were subjected from time T1 (after the first clinical-functional assessment) to a standardized rehabilitation treatment program. In particular, each patient underwent intensive hospital rehabilitative treatment, for the first 30 days taking part in 5 weekly rehabilitative sessions at the Hospital and Nursing Home Paolo Richiedei. From the 30th to the 60th day patients were followed on an outpatient basis with a rehabilitative treatment of 2 weekly sessions; the last 30 days of rehabilitative treatment provide 1 session per week with a program of exercises to be performed at home. Each session consists of a 1-hour treatment, conducted at the hospital gymnasium without and with orthotics, training the patient in a growing range of body sensitization exercises, muscle lengthening/relaxation, stabilization and proproprioceptive facilitation of postural control.
The proposed rehabilitation treatment model has set goals, previously established by the physiatrist and shared with the reference physiotherapists. The fundamental moments of the aforementioned treatment plan are:
• consciousness and body awareness (cognitive-behavioral training and correct muscle relaxation);
• increase of postural skills, with improvement of feedback and feedforward postural control and decrease in the number of falls per month;
• education in the use of the orthosis;
• constant monitoring of the foot-insole appropriateness;
• constant monitoring of patient’s compliance and adherence level with the performance of the exercises proposed and learned, with step by step evaluation of the results achieved;
• improvement of autonomy in the execution of daily life activities and reduction of fear of falling.
The choice of exercises, proposed to each patient, must necessarily take into account: a. the degree of progress of the disease; b. the skills of the individual; c. patient’s personal characteristics and interests. For the purpose of our study, we considered the following macro-areas of rehabilitative intervention:
• Area of intervention A: management and preliminary preparation of the patient
1. Body awareness and muscle relaxation
The rehabilitation session begins by inviting the patient to place himself on his back on the bed (Figure 20), with his head resting on the pillow, his eyes closed, his upper limbs supported with the palms of both hands facing upwards. From this position we require the patient to take a series of deep breaths, inhaling from the nose and exhaling from the mouth, in such a way as to induce global relaxation. We require the patient to concentrate consecutively on different parts of the body, becoming aware of their respective position and facilitating the progressive relaxation of the muscles.
2. Afferential stimulation of the foot sole
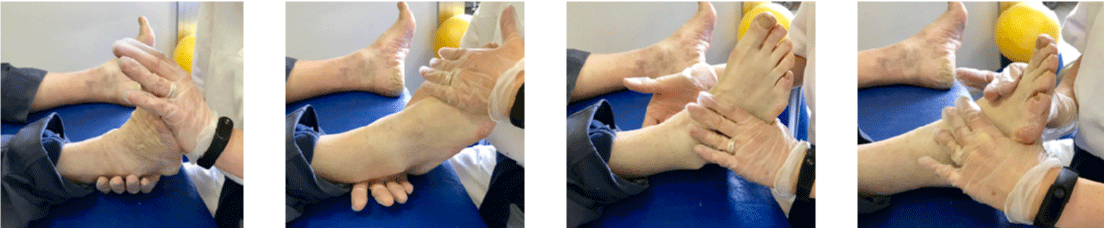
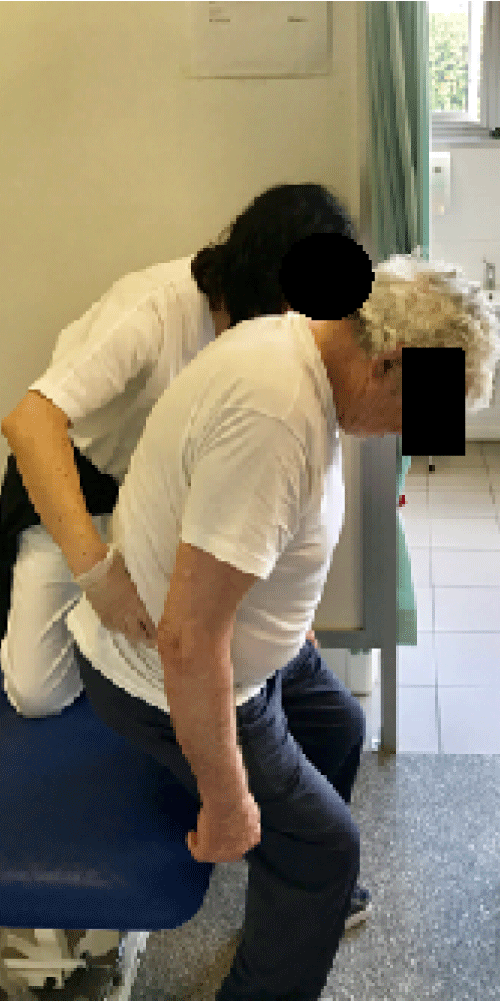
The patient is placed in a supine position on the bed. The therapist, through a manipulation, performs a manual stimulation of the plant of both feet (Figure 21) starting from the heel, proceeding along the entire plantar vault, up to the metatarsal heads and fingers, providing a series of tactile stimuli, useful for the re-acquisition of a correct awareness of the plantar support.
3. Passive, active assisted and active mobilization of the tibio-tarsic, on all motion plans granted
The therapist proposes a passive, active assisted and active mobilization of the ankle joint (Figure 22), on all movement planes granted in order to guarantee the greatest possible freedom in the degrees of articular movement. This type of exercise is designed to keep the joint free in such a way as to guarantee patient's maximum freedom during walking and during the activation of balance strategies. The ultimate aim is to improve the quality of the approach to the ground and the stability of the patient due to an easier activation of gait cycle.
Figure 22: Passive, active assisted mobilization of the ankle joint in flexion-extension and prone-supination (from own elaboration).
4. Peri-articular tissue manipulation
In order to make the ankle joint free, in addition to the aforementioned joint mobilization, the therapist performs a manipulation of the peri-articular tissues of the ankle (Figure 23), applying a different pressure on patient’s skin, depending on the plan tissue on which he wants to work.
5. Proprioceptive orthostatic plantar stimulation exercise with facilitation cues support
Patient is asked to keep the station upright by using support facilitation, in free-walk condition (without footwear) (Figure 24). Different types of thickness are supplied, of different nature and consistency; patient is asked to place his or her feet, forefoot, midfoot and heel on the proposed surfaces consecutively, and to describe the sensation given by the plantigrade support depending on the material used and the part of the foot placed on the support device.
Figure 24: Orthostatic plantar proprioceptive stimulation exercise with support facilitation cues (from own elaboration).
• Area of intervention B: “muscle chain remodeling”
1. Rebalance of the anterior and posterior cervico-brachial kinetic chain
The proposal of this type of exercise is intended to relax and inhibit the musculature related to the anterior and posterior cervico-brachial kinetic chain (Figure 25). The therapist, placed behind the patient, applies a pulling of the head and maintains the position for a few seconds, before returning to the initial position. For a specific treatment of the trapezius muscles the patient’s head is inclined (at first right, then left) and a distraction is applied between the head and the shoulder opposite to the direction of the inclination, slow and modulated; for the specific remodulation of the sternocleidomastoid muscles the head is placed in rotation (first to the right then to the left) initially applying a distraction between the rotated head and shoulder opposite the direction of rotation to act on the clavicle, and subsequently applying a traction on the breastbone, to remodulate the sternal portion of the muscle. All these maneuvers must be performed slowly, modulating traction, following the patient’s respiratory rhythm, according to the same procedures described above.
Figure 25: Re-modulation of the anterior and posterior kinetic-brachial kinetic chain (from own elaboration).
Rebalance of the axial anterior/posterior muscular kinetic chain
• Rebalancing of the axial posterior kinetic chain: the patient, placed in a supine position on the bed, carries both lower limbs to the chest and maintains position for a few seconds (Figure 26).
• Rebalancing of the axial anterior kinetic chain: the patient, placed in the prone position, carries out an extension of the rachis, unloading the weight on both elbows and forearms. The exercise is very complex in its execution for patients in which the camptcormic attitude is structured.
3. Rebalancing of the flexion-extensor and adductors/abductors of the lower limbs
In order to remodulate the kinetic flexion chain of the lower limbs, the therapist passively flexes patient’s hip, keeping the knee extended and bringing the ankle into dorsiflexion, until the patient feels tension, without feeling pain; the patient maintains the position for a few seconds.
The remodeling of the extensor chain takes advantage of the same principles: the patient placed on the edge of the bed in the supine position, with a lower limb outside the bed, the contralateral flexed with the foot resting on the surface, is passively brought by the therapist in position with extended hip (or in a neutral position) and flexed knee. In figure 27, on the other hand, the modalities of execution of the rebalancing exercises of the adductive/abductive kinetic chain of the lower limbs are shown.
Figure 27: Rebalancing of the flexion-extensor and adductors/abductors of the lower limbs (from own elaboration).
4. Active mobilization of the spine in all the motion plans granted
This last exercise involves active mobilization of the spine in rotation, inclination and flexion-extension.
• Area of intervention C: pro-proprioceptive and motor reinforcement of the “core-stability”
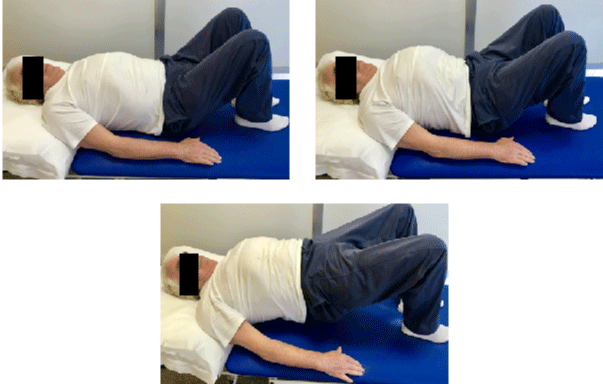
1. Facilitation exercises for the anti-gravity control of the trunk and stabilization of the pelvis through the achievement and maintenance of the bridge position, after active mobilization of the pelvis in anti/retroversion.
The patient is placed on his back (Figure 28), with the lower limbs flexed, feet resting on the bed, upper limbs resting on the bed or, in case he has more skills, crossed on his chest; after having the patient perform a retroversion of the pelvis, he is asked to activate the hip extensors, lifting the buttocks from the bed, and unloading the weight on the back-foot. Holds the position for a few seconds, and slowly returns to the initial position.
2. Facilitation exercises for the anti-gravity control of the trunk and stabilization of the pelvis maintaining the bridge position and performing rotation movements of the pelvis
Maintaining the position of the “bridge” according to the modalities described above, the patient is asked to perform movements of rotation of the pelvis on the right and on the left.
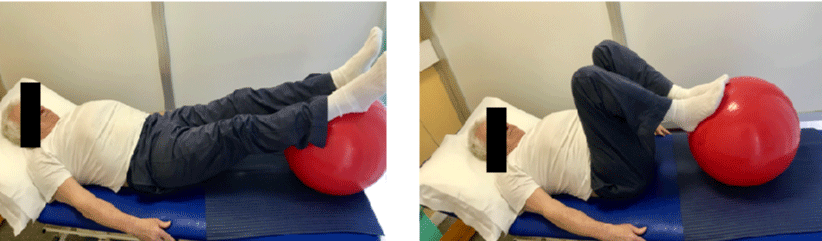
3. Exercises to strengthen the muscular recruitment of the lower-middle abdominal rectum
Patient is positioned supine on the bed, placed both lower limbs on a ball (Figure 29), is asked to activate the middle-lower abdominal rectum by bringing the ball close to the body and slowly returning to the initial potion.
Figure 29: Facilitation to strengthen the muscular recruitment of the lower-middle abdominal rectum (from own elaboration).
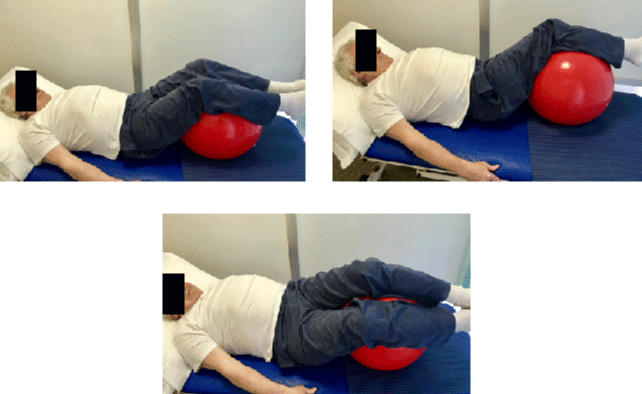
4. Reinforcement exercises for large and small oblique muscle recruitment
The patient is placed in a supine position on the bed with the lower limbs resting on a ball as shown in figure 30.
Figure 30: Reinforcement exercises for large and small oblique muscle recruitment (from own elaboration).
The exercise involves rotating the lower limbs alternately to the right and left, returning slowly to the neutral position. The exercise allows the recruitment of the large oblique and the small contralateral oblique.
5. Reinforcement exercises at the junction and fixation of the basin through the execution of the stop-stand
Patient placed in an upright position (Figure 31); starting from this position the stop-standing is performed; guiding the patient initially in the retroversion of the pelvis and subsequently in anteversion to reach the sitting position.
The execution must be slow and modulated, so as to guarantee a coordinated eccentric contraction of the core and of the antigravity muscles.
6. Proprioceptive control exercises in feedback and feedforward of the trunk-pelvis unit to be performed with the patient seated on the Bobath ball and requiring linear acceleration of the extension spine
The patient sitting on a Bobath ball (Figure 32), forced to control the pelvic basin unit at the proprioceptive level, requires linear acceleration in extension of the rachis with activation of the transversus of the abdomen.
Figure 32: Core pro-activation exercise, through execution of a linear acceleration in extension of the spine (from own elaboration).
• Area of intervention D: reinforcement of orthostatic balance reactions
1. Exercise of facilitating the movement of the load in an upright position
The patient, placed in an upright position, is invited to move the load alternately on the lower right limb and on the lower left limb, using a suitable support base, under the guidance of the therapist.
2. Static balance reinforcement exercise by keeping the standing station with a narrow base (feet together)
The patient keeps the standing station with a narrow base (feet together) for a few minutes. Once a stability condition is achieved, the patient is required to perform reaching with the upper limbs.
3. Static equilibrium reinforcement exercise through maintenance of the tandem/semi-tandem position associated with self-destabilization (feedforward postural control)
The therapist instructs the patient to maintain the tandem / semi-tandem position under static conditions. Once a stability condition is reached, flexion / extension, adduction / abduction with both upper limbs are required, either alternately or simultaneously.
4. Exercise of self-destabilization (feedforward postural control) by maintaining the standing position in semi-mono-podalic assessment, associated with the execution of movements of the upper limbs.
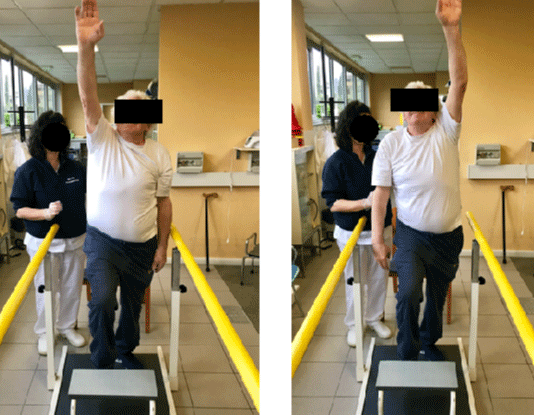
The patient placed in a semi-mono-breech position, with one foot resting on a step (Figure 33), is invited to maintain the position. Once stability is achieved, an indication is given to bring the upper limbs up and up alternately and quickly.
Figure 33: Exercise of self-destabilization (feedforward postural control) by maintaining the standing position in semi-mono-podalic assessment, associated with the execution of movements of the upper limbs (from own elaboration).
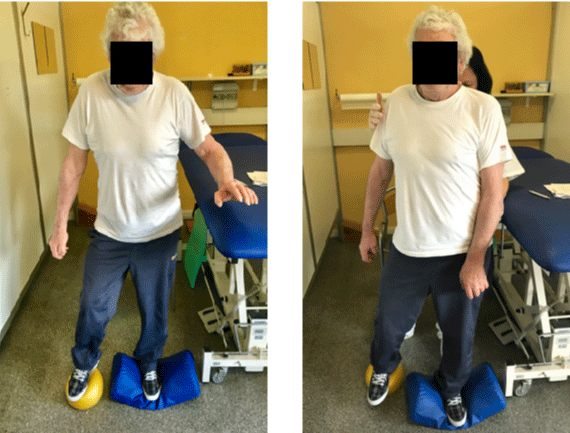
5. Exercise of self-destabilization (feedforward postural control) by maintaining the orthostatism in a mono-podalic position on an unstable surface, associated with the execution of movements of the contralateral lower limb resting on a ball.
The patient is placed in a standing position in a mono-podalic load on an unstable surface (Figure 34). The lower limb that is not resting is placed on a ball. The patient’s task is to maintain the balance while moving the ball forward and back. The destabilization within this exercise requires a good control of the equilibrium reactions both in feed-back (external destabilization) and in feedforward (self-destabilization induced by the movement of the lower limb not in loading).
Figure 34: Exercise of self-destabilization (feedforward postural control) by maintaining the orthostatism in a mono-podalic position on an unstable surface, associated with the execution of movements of the contralateral lower limb resting on a ball (from own elaboration).
6. Proprioceptive exercise of induced destabilization (postural feedback control) by maintaining the orthostatism in bi-podalic load on unstable surface
The patient is placed in an orthostatic position on an unstable oscillating surface (induced destabilization) (Figure 35). It is asked to keep the table as parallel as possible to the ground in order to improve the postural responses in feed-back, in particular in the regulation of the ankle activity.
Figure 35: Proprioceptive exercise of induced destabilization (postural feedback control) by maintaining the orthostatism in bi-podalic load on unstable surface (from own elaboration).
7. Proprioceptive exercise of induced destabilization (postural feedback control), by maintaining the orthostatism in mono-podalic load on unstable surface, associated with self-destabilization (feedforward postural control) by performing movements with the contralateral lower limb
The patient placed in an orthostatic position, in mono-podalic load on unstable surface, is asked to maintain the position. Once stability is achieved in this position, the patient should perform flexion movements of the hip and knee of the free limb in order to stimulate postural feedback and feedforward control.
Area of intervention E: resetting of the static and dynamic postural structure e of the kinesthetic profile of the movement
1. Proprioceptive control exercises in feedback and feedforward of the postural structure of the head-neck-trunk unit.
The patient is sitting on the couch, with his feet resting on the ground, his upper limbs relaxed, his pelvis and pelvis girdle aligned. The therapist poses posteriorly to the patient and accompanies the movements of flexion-extension, rotation and inclination of the head, verifying that the same selectively performs the motor task without the appearance of compensatory movements on the shoulder girdle, rachis or pelvis (Figure 36).
Figure 36: Proprioceptive control exercises in feedback and feedforward of the postural structure of the head-neck-trunk unit (from own elaboration)
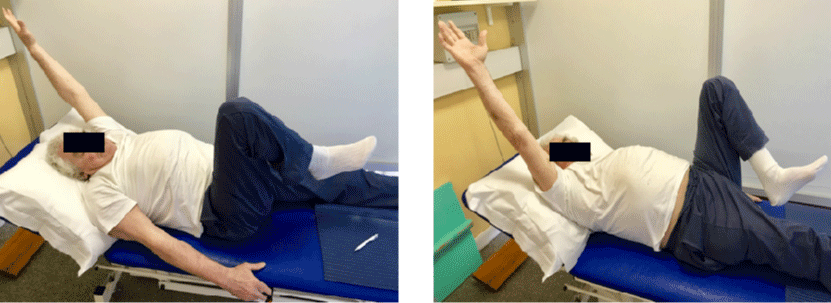
2. Exercise of proprioceptive control of the dynamic postural structure of the trunk-pelvis unit to be performed with the patient supine
Patient in the supine position, with lower limbs flexed and feet resting on the bed, keeps both upper limbs flexed to 90° in support of a stick. The two tracks are unwound, requiring the rotation of both knees to the right, and upper limbs, stick and head in the opposite direction. Then the opposite movement is asked. The movements described above are carried out alternately, for several repetitions (Figure 37).
Figure 37: Exercise of proprioceptive control of the dynamic postural structure of the trunk-pelvis unit to be performed with the patient supine (from own elaboration).
3. Exercise of coordination of the upper limbs and lower limbs to be performed with the patient supine
In order to improve the coordination between the upper and lower limbs, let the patient perform this exercise: the patient elevates the right upper limb and flexes the left lower limb simultaneously, then performing the opposite movement. The rhythm must be supported and the movement fluid (Figure 38).
Figure 38: Coordination of the upper limbs and lower limbs to be performed with the patient supine (from own elaboration).
4. Exercise of proprioceptive control in feedback and feedforward of the postural structure of the trunk-pelvis unit to be performed with patient in orthostatism.
The patient in an upright position rests the upper limbs on a ball resting on the bed properly raised as shown in figure 39. keeping the pelvis in neutral position requires an exercise to release the tracks, bringing the ball to the right and left, performing an isolated rotation of the trunk on the basin.
Figure 39: Exercise of proprioceptive control in feedback and feedforward of the postural structure of the trunk-pelvis unit to be performed with patient in orthostatism (from own elaboration).
5. Exercise of coordination of the path in synergy with a finalized reaching of the upper limbs
The patient is invited to walk with a ball in his hand. The goal of the exercise is to throw the ball with your right hand and take it with your left hand. This is a challenging coordination exercise that involves the following areas: bimanual activity, ambulation, feedback to feedback/feedforward balance, dynamic balance; it therefore requires great concentration on the part of the patient.
Area of intervention F: reinforcement of the orthodynamic equilibrium reactions
1. Exercise of strengthening of the orthodynamic equilibrium with introduction of facilitation cues (exercises of sensorimotor integration, auditory and visual)
Patient is invited to ambulate, alternately beating the hands anteriorly and posteriorly the trunk, so as to give himself a rhythm, as shown in figure 40. This is a hearing aid cues, as a scanned rhythm limits the presentation of freezing or motor slowdown while driving. It is a technique that the patient can use independently. As an alternative to hearing aid cues, visual cues can be used: in this case, adhesive tape is used to describe the path that the patient must perform.
Figure 40: Exercise of strengthening of the orthodynamic equilibrium with introduction of facilitation cues (exercises of sensorimotor integration, auditory and visual)(from own elaboration).
2. Exercise of strengthening of the orthodynamic equilibrium with a narrow support base (tandem gait)
It is an exercise in preparation for the increase of proprioceptive skills and of the orthodynamic equilibrium. The patient walks by placing one foot in front of the other in tandem gait (Figure 41).
3. Exercise of locomotor dexterity in variations of direction of the path and overcoming of obstacles
In this type of exercise, the patient must perform a path with obstacles of different nature and size, which can vary from session to session. Also the variation of direction is contemplated during the execution of this type of therapeutic exercise (Figure 42).
4. Exercise of locomotor dexterity in lateral gait
The patient is invited to perform a lateral gait, trying to keep the pelvis in neutral position as much as possible. It is an exercise of dexterity propedeutic to the acquisition of an effective dynamic balance, functional to daily life (Figure 43).
5. Exercise of locomotor dexterity in crossed lateral gait
The crossed lateral gait shown in the figure represents the next step in terms of difficulty and commitment of the proprioceptive system with respect to the lateral gait presented previously. The patient proceeds sideways alternately crossing the left and right lower limb and vice versa (Figure 44).
Statistical analysis
Statistical analysis was made using the SPSS statistical software. In relation to the smallness of our sample, we used the non-parametric Wilcoxon test (more suited to the analysis of small study samples) to delineate the time course from T1 to T2 (evaluation and rehabilitation inter-time) of the clinical-functional and instrumental data. The statistical analysis allowed us to highlight the trend of time-related variation, comparing the samples on the basis of the orthosis used and the underlying pathology, both at time T1 and after orthoses-rehabilitation treatment (time T2).
Results
VPA (Visual Postural Analysis) results
Recruited patients were subjected at T1 time and T2 to an objective evaluation of trunk postural assessment in toto in anterior-posterior and latero-lateral position (VPA or Visual Postural Analysis), with footwear and with synthetic foot insole and the Prodynamic insole, focusing attention on:
- shoulder and right and left hip alignment (in AP alignment);
- degree of symmetry and/or asymmetry of the so-called size triangles (in AP alignment);
- alignment of the head-neck-trunk unit (in AP alignment);
- assessment of the orthostatic plantigrade support at rest (in AP alignment);
- alignment of cervical lordosis, dorsal kyphosis and lumbar lordosis (in LL alignment).
In order to make a correct evaluation and differentiation of our results, recruited patients were divided into 4 different groups, according to the basic pathology and the type of orthotic device provided:
the P.A. group refers to those patients affected by Parkinson Disease, who were given the synthetic foot insole (patient P1 A.B. and P8 R.I);
the P.B. group refers to patients affected by Parkinson disease, who received the PRODYNAMIC foot insole (patient P3 M.S. and P4 F.S);
the PS.A. group refers to patients affected by Parkinsonism, who received the synthetic foot insole: to this category belong patient P5 (L.V.)(drop-out for aggravation of his clinical status and, therefore, not evaluable at the time T2) and P7 G.I;
the PS.B. group refers to patients affected by parkinsonism, who received the PRODYNAMIC insole (patients P2 L.S and P6 M.U).
The VPA profile acquired at time T1 and its variation trend defined at time T2 was accurately summarized in table 3.
| Table 3: Visual Postural Analysis (VPA). | ||||||
| Patient | Evaluation and condition time | Size triangles and scapolomeral cingulum |
Anterior-superior iliac spikes (ASIS) |
Head-neck unit | Plantar orthomorphism |
Postural attitude |
| P.A. group Patient P1 A.B. |
T1 | Asymmetry, with increased elevation of the left shoulder |
Asymmetry, with elevation of right ASIS | Head down, with anteposition; preternatural inflection on the left |
Hollow foot with minimal inflection in varus-supination with plantar flexed toes |
Accentuated dorsal hypercifosis, accentuated lumbar lordosis, flexion of the trunk on the pelvis, inclination of the left trunk |
| T2 | Unchanged asymmetry | Unchanged asymmetry | Improved preternatural inflection on the left |
Unchanged | Unchanged | |
| T2 with synthetic insole |
Lower left shoulder | Unchanged asymmetry | Improved preternatural inflection on the left |
Unchanged | Unchanged | |
| PS.B group Patient P2 L.S . |
T1 | Asymmetry, with elevation of right shoulder | Asymmetry, with increased elevation of left ASIS |
Standard alignment | Hollow foot, in particular extra-rotated left foot |
Dorsal hypercifosis, lumbar lordosis rectilinization, very slight inclination of the right trunk |
| T2 | Asymmetry amelioration, with decreased right shoulder elevation |
Asymmetry amelioration | Unchanged | Residual left foot extra rotation | Improved alignment of the trunk on the pelvis on the sagittal plane, inclination of the unmodified right trunk |
|
| T2 with Prodynamic insole |
Improvement of the asymmetry, only mentioned left shoulder elevation |
Less evident asymmetry | Unchanged | Residual left foot extra rotation | Improved alignment of the trunk on the pelvis on the sagittal plane, inclination of the slightly improved right trunk | |
| P.B. group Patient P3 M.S. |
T1 | Asymmetry, with slight elevation of right shoulder |
Asymmetry, with elevation of right ASIS | Head down, with anteposition; slight preternatural inflection on the right |
Hollow foot with valguspronation inflection of the back-mid foot |
Dorsal hypersensitivity, rectilinear lumbar stretch, flexion of the trunk on the pelvis |
| T2 | Ameliorated asymmetry | Ameliorated asymmetry | Postural attitude ameliorated |
Foot alignment ameliorated | Improved trunk relationship against gravity, disappearance of trunk flexion on pelvis |
|
| T2 with Prodynamic insole |
Residual asymmetry, right shoulder elevation just accentuated |
Residual asymmetry, elevation of iliac spine not detectable |
Improved anteposition, better alignment, disappearance right inflection |
Slightly improved rear-tomidfoot alignment in hollow foot | Improved trunk relationship against gravity, disappearance of trunk flexion on pelvis |
|
| P.B. roup Patient P4 F.S. |
T1 | Asymmetry amelioration | Improved asymmetry, elevation reduction of the right iliac spine |
Improved asymmetry, elevation reduction of the right iliac spine |
Hollow foot with minimal inflection in varus-supination of the back-midfoot |
Accentuated dorsal hypercifosis, rectilinear lumbar tract, flexion of the trunk on the pelvis lateral inflection of the left trunk |
| T2 | Maintained asymmetry, more aligned right shoulder |
Improved asymmetry, elevation reduction of the right iliac spine |
Maintained before the head, reduced the flexion of the head on the neck, disappearance left |
Slight hind-midfoot rearrangement in hollow foot |
Improved general postural attitude, dorsal hypercifosis, improved trunk flexion on the pelvis, lateral inflection of the left trunk still evident |
|
| T2 with Prodynamic insole |
Asymmetry amelioration | Asymmetry amelioration | Slightly improved head inclination, isappeared flexion, disappearance left inflection |
Hind-midfoot alignment ameliorated |
General postural attitude amelioration | |
| PS.B. group Patient P6 M.U |
T1 | Asymmetry with increased elevation of right shoulder |
Asymmetry, with elevation of left ASIS | Anteposition of the head, slight right rotated | Hollow foot, with rigid right toe, with minimal inflection in valgus-pronation of the backmidfoot |
Dorsal hypercifosis, rectilinear lumbar stretch, flexion of the trunk on the pelvis tilt of the left trunk |
| T2 | Improved asymmetry, slight reduction of right shoulder elevation |
Improved asymmetry, left SIAS residual elevation | Reduced head anteposition, reduced right head rotation |
Slight improvement of the rear-to-midfoot alignment in the hollow foot with the rigid right toe |
Dorsal hypercifosis and lumbar tract unchanged, improved trunk flexion on the pelvis and inclination of the left trunk |
|
| T2 with Prodynamic insole |
Improved asymmetry, reduced right shoulder elevation |
Slight asymmetry, with slight elevation of right ASIS |
Standard alignment | Hollow and swollen foot, with overload of the first left metatarsal |
Dorsal hypercifosis, normo lumbar stretch posed | |
| PS.A. group Patient P7 G.I. |
T1 | Slight asymmetry, with hinted right shoulder elevation |
Asymmetry amelioration, right hip elevation reduction |
Standard alignment | Hollow and swollen foot, with overload of the first left metatarsal |
Dorsal hypercifosis, normo lumbar stretch posed |
| T2 | Slight asymmetry, with hinted right shoulder elevation |
Asymmetryamelioration, right hip elevation reduction | Unchanged | Unchanged | Unchanged | |
| T2 with synthetic insole |
Unchanged | Unchanged | Unchanged | Unchanged | Unchanged | |
| P.A. group Patient P8 R.I. |
T1 | Slight asymmetry, with slight elevation of right shoulder |
Slight asymmetry, with slight elevation of right ASIS |
Standard alignment | Hollow and swollen foot, with overload of the first left metatarsal |
Dorsal hyperciifosis, normo lumbar stretch posed |
| T2 | Size Triangles symmetric, reduced elevation, anteposition of the right shoulder remains |
Slightly improved asymmetry, left SIAS residual elevation |
Better alignment of the head on the neck, reduced flexion and reduced anteposition |
Improved hind-midfoot alignment in hollow foot |
Global postural attitude amelioration |
|
| T2 with synthetic insole |
Unchanged | Unchanged | Unchanged | Unchanged | Unchanged | |
A general objective comparison, following the subdivision of patients in the previously described groups, showed that:
− within the P.A. group the results were clearly different between the patient P1 and P8; in particular, the former benefited, in postural terms, in a less striking way than the orthoses-rehabilitative treatment obtaining slight results in the symmetrization of the scapular girdle and in the improvement of the alignment of the head-neck unit on the frontal plane for which the left inflection recorded at time T1 has improved; on the contrary, patient P8 showed a general improvement of the most evident posture referable to the increase in symmetry of the triangles of the size, of the shoulder and hip tracks, of the alignment of the head-neck unit, as an expression of a rebalancing to the kinetic chain, a partial improvement of the hind-midfoot alignment thanks to the use of the plantar orthosis, and to the rebalancing of the kinetic chains;
− for patients belonging to the P.B group the results show a more homogeneous trend within the sample taken into consideration; infact, both patients registered, at time T2, a global improvement and an ergonomic remodulation of the overall symmetrical postural attitude in its articulation tracks, more tonic in the control of gravity and more suited to a good and satisfying quality of life;
− for patients belonging to the PS.A group the results give us information on a modest improvement in the symmetry of the triangles of the size, of the scapular girdle and of the pelvic girdle;
− for patients belonging to the PS.B group instead, a more evident improvement in the parameters evaluated compared to the previous group was recorded; in fact, an improvement was observed in the asymmetry of the scapular and pelvic girdles, the alignment of the head-neck unit and the anti-gravity skills of the trunk registered in the “postural attitude” section, in which we observed a better alignment of the trunk on the frontal plane and on the sagittal plane.
In general we can summarize that most of our patients, belonging to the study sample, have been able to find benefit from the use of the plantar orthosis and integrated rehabilitation treatment so as to bring some modifications, even if not particularly radical, within personal postural attitude, recording an improvement but not uniform change within the sample.
It is necessary to underline that, since Parkinson’s disease and Parkinsonism are progressive pathologies, patients affected by both clinical forms tend to establish incorrect postural attitudes due to stiffness and appearance of hypertonic plasticity, which, depending on the staging of the pathology, become then structured and only partially modifiable. The results obtained by comparing the VPA at time T1 and at time T2 provide a clear mirror of this reality, highlighting an improvement of the only partial general postural conditions for each patient according to their clinical picture and the progression of the disease.
These results were more evident during the evaluation of T2 with synthetic foot-insole/PRODYNAMIC as shown in table 3, whose efficacy differences have been previously described for each group, reinforcing the thesis according to which an adequate afferent stimulation of the foot-sole, ensuring proprioceptive information that is fundamental for postural control, can influence the overall postural attitude, even if limited, in the patient suffering from Parkinson’s disease or Parkinsonism.
VGA (Visual Gait Analysis) results
The objective evaluation of the analytic-global gait cycle was performed at time T1 and T2. The dynamic profile of the each step was analyzed, during the two evaluations, with footwear and with SYNTETHIC/PRODYNAMIC foot-insole, focusing on the excursion of the heel-contact phase, the stance-phase, the push-off phase, the dynamic attitude and eccentric control of the knee and of the behavior of the trunk-pelvis.
From a general objective comparison, following the subdivision of patients in groups described in the previously, there was a general performance improvement. In particular:
− within the P.A group we can highlight a partial improvement (less evident for P1 A.B.) of the VGA in the considered parameters, from time T1 to time T2; this improvement was more evident during the evaluation at time T2 with synthetic insoles, secondary to a relative facilitation provided by the orthotic device during the walk;
− within the P.B group the results were more striking; infact, there was a significant improvement between time T1 and time T2 with the Prodynamic insole in all the predefined parameters; more particularly we observed, in both patients belonging to the group, a partial or even complete normalization of the dynamic heel-contact phase, a better alignment of the COP in its excursion from the 1st to the 2nd rocker phase of the step, a notable facilitation to the inertial thrust in progress in the 3rd and 4th rocker phase provided by the orthotic device, an improvement in the eccentric control of the patellofemoral alignment in the acceptance phase of the so-called load-response in stance and, finally, the acquisition of a more physiological propulsion structure of the trunk basin unit with an improvement of the clearance and fixation skills in the sequential phases of the step;
− within the PS.A group a partial normalization of the foot alignment was observed during the heel-contact phase, and above all, the relative orthodynamic facilitation provided by the orthotic device (synthetic foot-insole) was detected during the push-off phase (4th rocker phase); the remaining parameters had a trend that was found to be substantially unchanged from the time T1 at the time T2 with synthetic foot-insoles;
− within the PS.B group the results showed with PRODYNAMIC foot-insoles use an improvement, from time T1 to time T2, of the dynamic foot alignment in the heel-contact phase and the alignment of the COP in its 1st to 2nd rocker step excursion; in a time-related comparison from T1 to T2, we observed with the PRODYNAMIC insole use the effectiveness of the inertial thrust facilitating progression in the 3rd and 4th rocker step phase in patients who had a more striking deficit; this attitude was accompanied by an improvement in the eccentric control of the knee in the load response step phase and by the acquisition of a better propulsive assessment of the pelvic trunk unit for both patients evaluated.
Clinical-functional results
In order to perform a correct clinical-functional evaluation, the following assessment scales were considered for each patient, involved in the study at time T1 and time T2, to evaluate the variation trend:
• Barthel Index Scale, for the evaluation of autonomy in daily life activities;
• Berg Balance Scale, for the evaluation of balance reactions.
• Conley Scale, for assessing the risk of falling;
• Tinetti Scale, for the assessment of balance and gait
In particular:
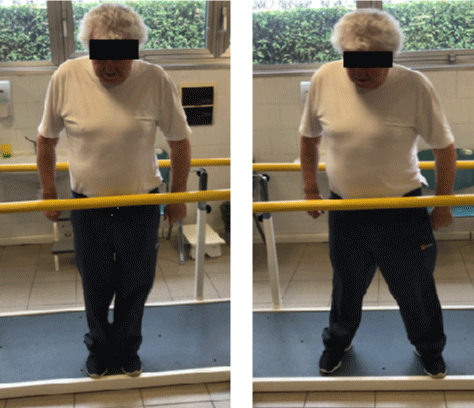
• analysis of the evolution of the degree of functionality in the daily life activities expressed by the Barthel index, passing from time T1 to the time T2, showed an improvement and consistent change in all groups considered within our study (Figure 44a);
• analysis of the evolutionary progress of the quality of static and dynamic balance control, expressed by the Berg Balance Scale, passing from time T1 to time T2, showed a more or less consistent improvement for all groups (Figure 44b) ;
• analysis of the objective evolutionary trend of the risk of falling and the perception of the fear of falling, expressed by the Conley scale, passing from time T1 to time T2, showed a more or less consistent improvement for all groups (Figure 44c) ;
• analysis of the objective evolutionary trend of the quality of the performance in the balance and gait control, expressed by the Tinetti scale, passing from time T1 to T2, showed a more or less consistent improvement for all study groups (Figure 44d).
Figure 44a,b,c,d. Evolutionary trend of the barthel Index, Berg Balance Scale, Conley Scale and Tinetti Scale passing from time T1 to T2 for each study group (from own elaboration).
Figure 44a-d: Evolutionary trend of the barthel Index, Berg Balance Scale, Conley Scale and Tinetti Scale passing from time T1 to T2 for each study group (from own elaboration).
Instrumental results
Static and dynamic baropodometric results: From an objective time-related and intra-group comparison (Parkinson’s disease and Parkinsonism) of the raw static baropodometric data acquired for each patient in the 4 predefined study conditions (FW or free walk, with footwear, with Prodynamic carbon-kevlar foot-insole orthosis or with synthetic foot-insole orthosis), a specific profile was detected for each related pathology group. In particular:
√ Static load response percentage (%)
- in the “footwear” study condition, at the time T1 the average levels of plantar load percentage relative to the group of Parkinson’s patients were higher on the left foot (53.97% on the left foot and 47.05% on the right foot); at time T2, after orthotic rehabilitative treatment, the load percentage was distributed more symmetrically between the two feet (52% on the left foot and 48% on the right foot); a similar trend was observed for patients affected by Parkinsonism passing from an average load distribution of 47.93% to 51.1% for the left foot and 52.07% to 48.9% for the right foot;
- in the “FW” study condition, at time T1 and in patients affected by Parkinsonism the average levels of the plantar static load were higher on the left foot rather than on the right foot (52.1% and 47.9% respectively) ; during the final evaluation, after orthotic rehabilitation treatment, values of 49.5% of load on the left foot and 50.5% on the right foot were recorded, indicating an improvement in load symmetry passing from time T1 to time T2; also for the Parkinsonism group a similar time-related trend of change can be highlighted, passing from average values for left and right foot respectively of 52.67% and 47.33% at the first evaluation, to values for left and right foot respectively of 50.13% and 49.87%;
- in the “Prodynamic foot-insole” study condition, at time T1 and in the Parkinson group a greater percentage of plantar load response was observed on the left foot compared to the right foot (respectively 52.25% and 47.75%); at time T2 there was an equal distribution in percentage of load response on both feet; for patients affected by Parkinsonism, there is a normalization of static plantar loading symmetry, passing from a percentage of average load on the left and right foot respectively of 47.95% and 52.05% at time T1, to a percentage of average load on the left and right foot respectively of 51.5% and 48.5% at time T2;
- in the “synthetic foot-insole” study condition, at time T1, the average load percentage values acquired in the Parkinson group were 56.55% on the left foot and 43.45% on the right foot; at the time T2 this trend underwent a variation in terms of percentage equal to 52.45% and 47.55% respectively on the left and right foot, indicating a slight improvement in the symmetrical distribution of plantar loading; as regards patients affected by Parkinsonism, the average load percentage detected at time T1 showed a condition of symmetry between the right and left foot with a trend that remained unchanged at time T2.
√ Average static pressure (kPa)
- in the “footwear” study condition, at time T1 the average orthostatic plantar pressure in the Parkinson group was higher on the left than on the right; at time T2 a greater increase was observed on the left foot than on the right; patients affected by Parkinsonism have shown a trend of time-related variation contrary to those with Parkinson’s; infact, at time T1, the mean value of the average orthostatic plantar pressure results higher on the left than on the right, recording a more or less equal decrease on the two feet at time T2;
- in the “FW” study condition, at time T1 the average orthostatic plantar pressure of patients with Parkinson’s showed overlapping average values for the right and left foot; at time T2, a downward trend was observed in the average orthostatic plantar pressure on the right foot, remaining unchanged on the left; for patients affected by Parkinsonism a trend was observed in increasing orthostatic plantar pressure on the right foot from time T1 to time T2 and a slight decrease on the left foot;
- in the “Prodynamic” study condition, at time T1, the average orthostatic plantar pressure was higher on the left than on the right in Parkinson’s patients with a trend that remained unchanged at time T2; the time-related variation trend of patients affected by Parkinsonism has instead shown a decrease in orthostatic plantar pressure in both feet at time T2;
- in the “synthetic foot-insole” study condition, at time T1 and in patients with Parkinson’s the average orthostatic plantar pressure was slightly greater on the left; Parkinsonism patients who used the synthetic insole recorded similar average values between the right and the left foot both at time T1 and at time T2.
√ Surface static plantar support (cm2)
- in the “footwear” study condition, at time T1 and in Parkinson’s patients, the static plantar support surface was slightly higher on the left foot; at time T2, following orthotic-rehabilitative treatment, this data showed a decreasing trend compared to time T1, reversing, however, the relationship between right and left foot; for patients affected by Parkinsonism there was a symmetrical increase in the static plantar support surface for both feet;
- in the “FW” condition, at the time T1 the average values of the static plantar support area for Parkinson’s patients were slightly higher on the left foot; passing from time T1 to time T2, after treatment, we see a slight increase in the static support area on the right and a slight decrease on the left; the mean values of the static plantar support area for patients with Parkinsonism were similar for the right and left foot at time T1, recording a significant trend of increase of the plantar surface bilaterally at time T2;
- in the “Prodynamic” study condition, at time T1, the surface static plantar support of patients with Parkinson’s was shown to be the same for the left and right foot; the time-related trend of variation showed a significant increase in the surface static plantar support bilaterally at time T2; patients with Parkinson’s disease showed higher orthostatic surface plantar support values at time T1; at time T2 there is a slight decrease in the static surface plantar support on the right with invariability on the left;
- in the “synthetic foot-insole” study condition, at time T1 the plantar support area is greater on the left foot than on the right in patients with Parkinson’s, with a trend of variation at time T2 decreasing the plantar support surface on the left; in patients affected by Parkinsonism a trend of bilateral variation was observed in increase of the orthostatic plantar surface support passing from T1 to T2.
An objective time-related and intra-group comparison of the raw dynamic baropodometric data acquired in the 4 study conditions of our work (free-walk, with footwear, with synthetic foot-insoles or with Prodynamic foot-insoles), showed different time-related trends for the two groups taken into consideration. In particular:
√ Dynamic step total area (cm2)
- in the “shoe” study condition, at time T1 and in Parkinson’s patients the average value of the total orthodynamic support area resulted slightly higher on the left; passing from time T1 to time T2 we observed an invariability of this trend on the right foot with a decreasing trend on the left; in patients with Parkinsonism at time T1 we recorded overlapping values on the left and on the right;
- in the “FW” condition, at the time T1 the dynamic step total area of Parkinson’s patients was higher on the right; passing from time T1 to time T2, after orthotic rehabilitation treatment we see a more or less symmetrical decrease on the right and left, with a trend slightly higher on the right; patients affected by Parkinsonism recorded a trend of decreasing variation bilaterally passing from time T1 to time T2;
- in the “Prodynamic” study condition, at time T1 and in patients with Parkinson’s disease, the dynamic step total area was higher on the left; this trend undergoes a bilateral decrease much more evident at time T2 on the left; patients affected by Parkinsonism have instead shown an average value of the dynamic step total area higher on the right, with a trend that remains unchanged at time T2;
- in the “synthetic foot-insole” study condition, at time T1 and in patients with Parkinson’s the dynamic step total area was equal on the right and left foot, recording a time-related variation trend, passing from time T1 to T2, growing on the right and slightly decreasing on the left; patients affected by Parkinsonism recorded a symmetrical bilateral increase of this data, passing from time T1 to time T2.
√ Orthodynamic step duration (m/sec)
- in the “footwear or shoe” study condition, at time T1 the orthodynamic step duration was almost symilar on the right and left in patients with Parkinson’s; a comparison between the values obtained at time T1 and the values obtained at time T2 underline an increase in the duration of the step on the right and a substantially unchanged on the left; patients affected by Parkinsonism have recorded an average value relative to the orthodynamic step duration slightly higher on the left; at time T2 a substantially unchanged trend can be observed on the right, and a decrease in the average value on the left;
- in the “FW” study condition, at time T1 the dynamic step duration in patients with Parkinson’s was higher on the left; passing from time T1 to time T2 we observed a substantially unchanged trend on the right and decreasing on the left; at time T1 the dynamic step duration of patients with Parkinsonism was equal on the right and on the left compared to a minimum greater value on the left; at time T2 we observe a bilateral and symmetrical increase in the dynamic step duration;
- in the “Prodynamic” condition, at the time T1 and in patients with Parkinson’s a slight increase in the step duration was observed on the right with a trend increasing at time T2 ipsilateral; patients with Parkinsonism have experienced a similar time-related trend.
- in the “synthetic foot-insole” study condition, at time T1 and in patients with Parkinson’s the step duration was greater on the right foot than the left, with a trend decreasing bilaterally at time T2; patients with Parkinsonism recorded an increasing trend in dynamic step duration on the left and unchanged on the right.
√ Dynamic mean plantar pressure (Kpa)
- in the “shoe” study condition, at the time T1 and in patients with Parkinson’s the dynamic average plantar pressure was almost superimposable on the right and on the left with a bilateral symmetrical variation trend at time T2; patients with Parkinsonism recorded a trend of opposite variation showing from time T1 to time T2 an asymmetric bilateral decrease in the mean value of the average orthodynamic plantar pressure on the right and on the left;
- in the “FW” study condition, at time T1 and in patients with Parkinson’s, the dynamic average plantar pressure was equal on the right and left; passing from time T1 to time T2, after using the orthosis and at the end of rehabilitative treatment, we are witnessing a slight more significant bilateral increase on the left; in patients with Parkinsonism there was, at time T2, an incremental variation trend on the right with invariability on the left;
- in the “Prodynamic” condition, at time T1 and in patients with Parkinson’s, the average orthodynamic plantar pressure was slightly higher on the left; this trend undergoes a slight increase at time T2 on the left side compared to the right foot; patients affected by Parkinsonism recorded a trend of variation of the average orthodynamic plantar pressure value increasing to the right with invariability to the left;
- in the “synthetic foot-insole” condition, at the time T1 and in patients with Parkinson’s, the dynamic average plantar pressure was equal to the right and left, with a trend of time-related variation decreasing at time T2 bilaterally; similar trend was observed in patients with Parkinsonism passing from time T1 to time T2.
WIVA system gait analysis results
With regard to the WIVA gait analysis of our sample, for each considered study condition (free walk, with footwear, with synthetic foot orthosis and Prodynamic foot orthosis in carbon-kevlar) a careful collection of raw patient-related data going from time T1 to time T2 was realized. Starting from the aforementioned data, for each predefined study condition and evaluation time considered it was possible to calculate the mean and standard deviation of the gait cadence, of the stance phase duration on the right and left, of the swing phase duration on the right and left, of the double gait support duration, of the stride length and of the gait speed.
From an objective time-related and intra-group comparison of the raw data acquired for each patient in the 4 predefined study conditions, a specific profile was found for each pathology group, highlighting different trends passing from time T1 to time T2. For the specific purposes of our study and focusing attention on the WIVA kinematic parameters with a more significant time-related change profile of our interest, we observed:
√ Gait cadence (steps/min) (Figures 45,46)
Figure 45: Trend of variation of average cadence values by study condition and by time for Parkinson and Parkinsonism (from own elaboration).
Figure 46: Trend of variation of average cadence values by study condition and by time for Parkinson and Parkinsonism (from own elaboration).
- in the “shoe” study condition the average path cadence value obtained from the raw data related to the Parkinson group at time T1 is slightly lower than the values calculated at time T2, going from an average cadence of 52.5 ± 2.3 steps per minute to an average rate of 53.8 ± 4.6; the trend of variation from time T1 to the time T2 is more evident for the Parkinsonism group in which it passes from an average cadence of 36.9 ± 15.8 obtained during the first evaluation to reach the value of 46.9 ± 5.8 obtained during the final evaluation;
- in the “FW” study condition, at time T1 the gait cadence of patients suffering from Parkinson’s disease is clearly lower than the speed detected at time T1 in the “footwear” condition; passing from time T1 to time T2, following orthotic-rehabilitative treatment, there is an important increase in the gait cadence: the average values, infect, pass from 39 ± 20.8 steps per minute to the first evaluation, to 51.3 ± 7.5; an analogous trend had the mean gait cadence of patients affected by Parkinsonism which increased from 33 ± 19.7 to 47 ± 7.3 steps per minute;
- in the “Prodynamic” study condition the gait cadence shows a significant increase from time T1 to time T2, passing respectively from an average value of 41.9 ± 11.7 to 54.9 ± 1.1; patients of the Parkinsonism group showed a value of the average gait cadence at time T1 higher than the other study conditions at the same evaluation time, with an increase of this data from T1 to T2, passing from 43.1 ± 11.8 to 47.4 ± 4.4;
- in the “plantar synthetic” study condition, patients of the Parkinson group showed an increase of the gait cadence from time T1 to T2, passing from a value of 43.3 ± 13 to 54 ± 3.4; the results obtained from the comparison between the “Prodynamic” and “synthetic foot-insole” study conditions were comparable; in patients with Parkinsonism, on the other hand, the mean value of the gait cadence shows a more evident increase from time T1 to T2 compared to the Parkinson group for the “Prodynamic” study condition, going from an average value of 38.4 to 46.8 steps per minute;
- it is also interesting to note that at time T2, for all the study conditions considered, the gait cadence showed more or less overlapping values for both study groups.
In relation to a normative value equal to 54.3, equally distributed between men and women, the aforementioned data suggest that Parkinson’s patients we witness a general normalization of the average gait cadence value, more or less significant for each study condition considered and predominantly with the use of the PRODYNAMIC foot-insole; passing from time T1 to T2, a similar improvement trend was shown by patients suffering from Parkinsonism, even though they did not reach the level of Normality on a par with the first group.
√ Gait speed (m/sec) ( Figures 47,48)
- in the “shoe” study condition the average gait speed value for patients with Parkinson’s shows a pre and post-treatment rehabilitation trend unchanged before and after treatment; the mean value of gait speed in patients with Parkinsonism shows an increase going from T1 to T2 (45 ± 20.6 m/sec vs 57.2 ± 7.9 m/sec);
- in the “FW” study condition at time T1 the gait speed is lower than the same data recorded in the other predefined study conditions in Parkinson’s and Parkinsonism; passing from time T1 to time T2 there is an incremental time-related variation trend for both groups;
- in the “Prodynamic” study condition at T1 the gait speed in Parkinson patients is similar to that recorded in the “shoe” study condition; from time T1 to time T2, the speed of the path undergoes an important incremental trend; in Parkinsonism the gait speed recorded at time T1 is higher than that recorded in the other study conditions; at time T2 there is a less evident increase in speed compared to that observed in patients with Parkinson’s;
- in the “synthetic foot-insole” condition, patients with Parkinson’s showed an incremental course of gait speed passing from time T1 to time T2, even though the trend was lower than that observed in the “footwear” and “Prodynamic” study conditions; even in patients with Parkinsonism there was an increase in the average gait speed value from time T1 to time T2, although it remained less evident than in the same study condition of the Parkinson group.
Figure 47: Trend of variation of average gait speed values by study condition and by time for Parkinson and Parkinsonism (from own elaboration).
Figure 48: Trend of variation of average gait speed values by study condition and by time for Parkinson and Parkinsonism (from own elaboration).
In relation to a normative value equal to 74.4 m/min, equally distributed between men and women, the aforementioned data suggest that in the group of Parkinson’s patients we are witnessing a general improvement with a maximum peak at time T2 and more significant in the “PRODYNAMIC” study condition; passing from time T1 to T2, a similar improvement trend was shown by patients suffering from Parkinsonism, even though they did not reach the level of Normality on a par with the first group.
√ Stance phase duration (% cycle)
- in the “shoe” study condition at time T1 the duration of the stance phase in patients with Parkinson’s was slightly higher on the right; at time T2 there was a slight decrease in the duration of the stance phase on the right and a slight increase in the stance phase on the left; in Parkinsonism at time T1 the duration of the stance phase was higher on the left, with a slight decrease of this value at time T2 on the right and left (although the value of stance on the left remained higher);
- in the study condition “FW”, patients with Parkinson’s showed at the time T1 a same stance phase duration on the right and on the left, while still predominating the left side; going from time T1 to time T2, after orthotic rehabilitation treatment, we are witnessing a time-related trend substantially overlapping; in patients with Parkinsonism, at time T1 the duration of the stance phase was higher on the left; at time T2 an increase in the stance value was observed on the right, reversing the ratio between right and left recorded at time T1;
- in the “Prodynamic” study condition, in patients with Parkinson’s the mean value of the stance phase duration was greater on the left at time T1; this trend undergoes a decrease at time T2 on the left, and a slight increase on the right; patients affected by Parkinsonism recorded an average value at time T1 more or less overlapping between right and left, with modification of the trend at time T2;
- in the “synthetic foot-insole” condition, in patients with Parkinson’s at the time T1 the duration of the stance phase was higher on the left, with a trend of variation increasing on the right and a slight decrease on the left at time T2; in patients with Parkinsonism a higher value was detected at time T1 on the right with an invariable trend on the right and slightly decreasing on the left passing from time T1 to time T2.
In relation to a normative value equal to 60.3 (% cycle), equally distributed between men and women, the aforementioned data suggest that, in both groups of recruited patients and in the “footwear, FW and Prodynamic” conditions, we assist to a more or less significant normalization of the duration of the stance phase (% cycle) on the right and left; in patients with Parkinsonism alone, the duration of the stance phase was comparable between the right and left in the “footwear and synthetic foot-insole” conditions.
√ Swing phase duration (% cycle)
- in the “footwear” study condition at time T1, the swing phase duration of the swing of patients with Parkinson’s was slightly higher on the right; at time T2 the trend proved to be substantially unchanged; in patients with Parkinsonism, at the time T1, a longer swing phase duration was observed on the left, with a symmetrical trend on the right and left at time T2;
- in the “FW” condition at time T1, the swing phase duration was predominant on the right side in the Parkinson group; passing from time T1 to time T2, we see an important decrease of the aforementioned duration on the right and an increase on the left; in patients with Parkinsonism at time T1 an increase of the swing phase duration was recorded on the right with a trend that remained unchanged at time T2;
- in the “Prodynamic” study condition, at time T1, the swing phase duration is greater on the right for Parkinson’s patients; this trend undergoes an increase at time T2 on the left; in the Parkinsonism group the trend remained unchanged between the right and left, passing from time T1 to time T2;
- in the “synthetic foot-insole” condition, at time T1 the swing phase duration was higher on the right in patients with Parkinson’s, with a trend that remains unchanged on the left and decreases on the right passing from time T1 to time T2; in the Parkinsonism group there was a time-related trend substantially unchanged on the right and slightly decreasing on the left, passing from time T1 to time T2.
In relation to a normative value equal to 39.6 (% cycle), equally distributed between men and women, the aforementioned data suggest that in the group of patients suffering from Parkinson’s we witness a general normalization and symmetrization of the swing phase duration on the right and left in the “footwear and Prodynamic” study conditions; going from time T1 to T2, normalization trend between right and left has been highlighted by patients affected by Parkinsonism in the Prodynamic study condition.
√ Double gait support duration (% cycle)
- in the “shoe” study condition at time T1, Parkinson’s group patients showed a decrease in the mean value of the double gait support duration, passing from time T1 to time T2; patients affected by parkinsonism have experienced an exactly opposite variation trend;
- in the “FW” condition, at time T1 the double gait support duration in Parkinson’s group patients is clearly lower than double gait support duration detected at time T2; passing from time T1 to time T2, there is an increase of the double gait support duration; a similar trend was experienced by patients suffering from Parkinsonism;
- in the “Prodynamic” study condition, the double gait support duration shows an important decrease in the Parkinson group passing from time T1 to time T2; the Parkinsonism group shows a similar decrease passing from time T1 to time T2, but in a lower way;
- in the “synthetic foot-insole” condition, the double gait support duration showed a decrease passing from T1 time to T2 in the Parkinson group; patients affected by Parkinsonism recorded a more significant decrease of the double gait support duration in the Prodynamic condition, passing from time T1 to time T2.
In relation to a normative value equal to 9.5 (% cycle), equally distributed between men and women, the aforementioned data suggest that in the group of patients suffering from Parkinson’s we see an improvement in the double gait support duration, from time T1 to time T2, in the “footwear”, “Prodynamic” and “synthetic foot-insole” conditions, with a trend closer to normalization for the “Prodynamic” condition; patients with Parkinsonism instead showed an improvement trend, from time T1 to time T2, exclusively in the “Prodynamic” and “synthetic foot-insole” conditions, with an opposite trend in the remaining conditions of the study.
√ Stride lenght (% cycle lenght)
- in the “shoe” study condition, at the time T1 the average stride length appears to be slightly lower than the stride length detected at time T2 in the Parkinson group; for patients affected by Parkinsonism the trend of time-related variation of the stride length shows a slight increase passing from time T1 to time T2;
- in the “FW” condition and at time T1, in patients with Parkinson’s the stride length was less than the length detected at time T2; patients affected by Parkinsonism have shown a modification of the data passing from time T1 to time T2;
- in the “Prodynamic” study condition, patients with Parkinson’s showed a marked increase in the average stride length, passing from time T1 to time T2; in patients of the Parkinsonism group there was an increase in the stride length at time T2 more or less similar to that recorded in the “footwear” study condition;
- in the “synthetic foot-insole” study condition, in patients with Parkinson’s the stride length shows an improvement passing from time T1 to T2, even if it does not reach the values recorded with the Prodynamic foot-insole; in the Parkinsonism group we observed an improving and increasing trend in the average stride length, passing from time T1 to time T2, higher than that observed in Parkinson’s;
- it is interesting to note that, in the group of patients affected by Parkinsonism, the average stride length values are more homogeneous in the different study conditions than those detected for patients with Parkinson’s disease.
In relation to a normative value equal to 1.37 (% cycle length), equally distributed between men and women, the aforementioned data suggest that in the group of patients suffering from Parkinson’s we see an improvement and normalization of the average stride lenght, proceeding from time T1 to time T2, mainly in the “Prodynamic” study condition; patients affected by Parkinsonism have instead shown an improvement trend, from time T1 to time T2, in all study conditions with a greater normalization of this data at time T2 for the “synthetic foot-insole” study condition.
Discussion
In a modern management of the profile of complexity of extrapyramidal pathology, the association of several health figures is of fundamental importance. Within the team, responsible for the integrated management of the extrapyramidal patient, figures such as physiatrists, physiotherapists, occupational therapists, speech therapists and dieticians find their work available from the earliest manifestations of the disease. In the management of the extrapyramidal disease, rehabilitative therapy has an important role, proposing effective approaches, perfectly integrated with pharmacological treatments, which have opened new perspectives on the recovery of the motor function of the patient. With this in mind, a new frontier, not yet fully explored, can be represented by the use of a plantar orthotic device, previously prescribed by the physiatrist, as a true sensor-motor facilitator of the foot sole and a as tool for afferent remodeling of strategies to control antigravity support reactions. From a careful analysis of the current literature, we can draw important considerations and arguments for discussing our results:
- Qiu F and collaborators evaluated the efficacy of a textured foot-insole, noting that postural stability in orthostatism can be improved by increasing the somatosensory information received from the foot orthoreceptor/mechanoreceptors; the textured slabs used have proved to be significant for the reduction of postural oscillations both in orthostatism on a stable surface, and on unstable surfaces without the aid of the visual system, thus concluding that this device could represent a low cost means to improve postural stability in high-risk groups (Parkinson’s disease) [16];
- Jenkins ME and collaborators, studying the effect of facilitating orthotics, have overall found an improvement in the objective spatio-temporal parameters of the gait; in particular, a significant improvement in the duration of the stance phase and the supporting capacity of the limb during load acceptance was demonstrated, expressing a significant improvement in overall stability; furthermore, the facilitating orthosis device has normalized the timing of activation of the anterior tibial muscle, which translates into an improvement in the quality of the support to the ground, closer to normal; overall, these improvements represent an increase in overall stability and gait safety in this population [12];
- Lirani-Silva E and collaborators, analyzed the plantar sensation and gait assessments by using an optoelectronic device; recruited patients were studied in three moments (before and after one-week wearing a group specific insole –experimental group- and after one week wearing conventional insoles); the textured insole had half-sphere elevations placed in the distal phalanx of the hallux, heads of metatarsophalangeal joints and heel; results showed that the use of textured insole for one week improved plantar sensation and stride length; the data suggest that the continuous use of textured insoles for one week benefits plantar sensation and gait in patients with PD.
Going to analyze the specific purpose of the aforementioned studies it is clear how different study groups, engaged in understanding and planning the most appropriate strategies and modalities of care and education of the Parkinsonian patient, have understood the relationship between reduced somatosensory function and poor postural stability. It is emphasized that in both the above mentioned studies, the effectiveness of a synthetic foot-insole made of thermoformable material (EVA) was tested, in order to maximize the cutaneous-proprioceptive sensation along the podalic perimeter. The conclusion of these studies was, therefore, to delineate in a cohort of patients suffering from Parkinson’s disease the simple effect of mechanical stimulation of plantar receptors, objective parameters of the path and of orthostatic stability in conditions of disequilibrium. According to this line of thought, the aim of our study was to demonstrate the pro-proprioceptive value of a new model of dynamic orthosis (PRODYNAMIC foot-insole) in the process of remodeling the spatial and temporal gait parameters of a group of patients suffering from extrapyramidal pathology (Parkinson’s disease and Parkinsonism) and belonging to a standardized integrated rehabilitation treatment course. The dynamic plantar orthosis proposed within this study, infact, not only offers a better mechanical stimulation of plantar receptors; made by a carbon-kevlar shell, it expresses in its conformation and manufacturing methods, pro-functional and pro-dynamic properties unique in its kind: lightness, ductility, malleability and extraordinary “lever effect” properties (elastic return effect in response to the load); the effectiveness of this device with such characteristics has been compared with the now more well-known static properties of a conventional multi-layer pro-ergonomic plantar used in the reference sample. The results obtained within this study must be interpreted taking into consideration:
- the heterogeneity of the recruited patients;
- the different types of clinical manifestations of the two diseases considered, certainly influencing the different degree and intensity of treatment response proposed in our study;
- the different degree of disability resulting from the progression of the pathology, also influencing the different degree of response to the rehabilitation treatment;
- the necessary individuality in the planning of the rehabilitative treatment proposed to each patient of the sample that potentially could have produced a trend of response to the integrated not-uniform treatment.
Using a personalized study design, temporally divided into clinical and experimental evaluation phase, we subjected our patients to a space-time examination of the step using the WIVA system, using a multi-layer pro-ergonomic insole and comparing it with the PRODYNAMIC insole from us proposed in 4 specific study conditions at the time T1. We divided our sample into two distinct groups, which showed a different response to the orthoses and rehabilitative treatment. An objective time-related and intra-group comparison of the mean values obtained from the WIVA space-time raw data acquired in the four study conditions showed different trends passing from time T1 to time T2. In particular, there has been an improvement in all the study conditions of the cadence and the speed of the walk in a more or less symmetrical way for both groups. Patients with Parkinson’s disease also highlighted:
• a considerable increase in walking speed in the PRODYNAMIC plantar study condition, a value so far recorded closer to those considered as normal;
• it was observed, in the study condition with PRODYNAMIC foot-insole, a trend of symmetry and normalization of the duration of the stance phase on the right and left passing from time T1 to time T2 (pro-dynamic facilitation for peripheral remodulation of the duration of load distribution in stance);
• the ability of the PRODYNAMIC insole to induce a normalization of the duration of the swing phase (advancement), closer to the normal values, with consensual symmetry (facilitating the inertial thrust in advancement) appeared;
• the duration of the double support phase has undergone an important improvement trend in the prodigious plantar study condition;
• we also clearly and predictably observed an increase in the length of the step already starting from time T1 with an improvement trend at the time T2 by using PRODYNAMIC insole; an inverse trend of modification of this parameter we have observed in the FW condition passing from time T1 to time T2. With regard to the patients belonging to the pathology group Parkinsonism, the trend was substantially unchanged from time T1 at the time T2 for most of the parameters evaluated, with the exception of the patient P7 GI, belonging to the Parkinsonism group to which the insole was provided. From this result we can suppose that the best response to the orthoses-rehabilitative treatment, highlighted by the progress of the values acquired during the two evaluations of the spatio-temporal parameters of the path, is simply attributable to the individual characteristics of our patient.
To increase our objective point of view on the functional usefulness of the Prodynamic foot-insole, we also used a well-known static and baropodometric analysis of our sample patients. An objective time-related and intra-group comparison of the static baropodometric raw data acquired in our 4 study conditions showed different trends passing from T1 to T2. In particular:
- in both study-pathology groups, a more or less consistent symmetrization trend of the plantar load percentage was observed, passing from T1 to T2 in all study conditions; this trend is particularly highlighted in the “plantar prodynamic” study condition of Parkinson’s patients, reaching in this case a perfect symmetry of load between both feet which has more or less maintained even in the condition FW;
- the detection of the average static pressure of patients belonging to the Parkinson’s disease pathology group showed an incremental trend from time T1 to time T2 in the footwear condition; furthermore, from the time T1 in the prodynamic study condition, a trend of incremental symmetry of the parameter is observed with respect to the remaining conditions for the same evaluation time, which has remained more or less unchanged at time T2; the increase in the average level of plantar pressure in the condition of orthostatism can be considered an indication of a greater and better stimulation of plantar cutaneous receptors; patients suffering from Parkinsonism have instead obtained different results, with a decremental trend of the mean value of the static foot pressure in the footwear and synthetic conditions, which remains unchanged in the FW and Prodynamic conditions;
- interesting was the selective effect of the PRODYNAMIC insole in determining a trend in the symmetrization of the aforementioned parameters.
An objective time-related and intra-group comparison of the dynamic baropodometric raw data acquired in the four study conditions of our work, has also highlighted different trends passing from time T1 to time T2. In particular:
- the evolutionary trend of the population affected by Parkinson’s during the evaluation with a PRODYNAMIC foot-insole is evident; in particular, the decrease of the orthodynamic total support area on both feet was highlighted, passing from time T1 to time T2; this trend was revealed in the same way in FW condition and with the footwear passing from time T1 to T2, while it showed no significant change with the use of the synthetic foot-insole (absence of prodinamicity = absence of a dynamic baropodometric remodulation of the total plantar support area); patients with Parkinsonism showed a substantially unchanged trend proceeding from T1 to T2 for all study conditions considered;
A critical analysis of these baropodometric study results allowes to highlight:
- how the response to orthoses-rehabilitative treatment cannot be perceived and metabolised in a different way from subject to subject with the same treatment proposed;
- how the trend of the data found would demonstrate a greater value of the PRODYNAMIC insole in terms of pro-proprioceptive “facilitation” of the antigravity strategies control support reactions of patients affected by Parkinson’s disease; this answer;
- how the uniqueness and innovative way of manufacturing of the PRODYNAMIC custom-made foot-insole would tend to produce different answers regarding the spatio-temporal gait parameters;
- how the different response to orthoses-rehabilitative treatment, in force among the group of patients with PD and those with Parkinsonism, clearly reflects the different pathophysiology underlying the 2 conditions; patients belonging to the second group, infact, recorded a less evident or even unchanged improvement trend, passing from T1 to T2, compared to patients belonging to the first group; we can presume that the important heterogeneity of the physiopathologic and syndromic profile characterizing the Parkinson disease and Parkinsonism is an expression of a different compromise of the neurophysiological systems responsible for the modulation of the path and postural balance reactions.
With the aim of outlining the clinical impact of the rehabilitative treatment proposed, a clinical-functional evaluation was also performed proceeding from time T1 to T2 time by using the Barthel Index Scale, Berg Balance Scale, Conley Scale and Tinetti scale. In a non-disregarded manner, we could observe a more or less consistent improvement in all patients of our sample for all the outcome measures considered. We believe that the proposed rehabilitation path meets our expectations, succeeding in promoting and certainly not hindering the pro-functional and facilitation properties of the path inherent in the biomechanical characteristics of the PRODYNAMIC foot-insole. It appears possible to state how our study has succeeded not only in delineating points of collimation with the results obtained by the Jenkins ME group and collaborators [12], demonstrating an overlapping effectiveness of the facilities induced by the guided rehabilitative path, but also showed a strong point in comparing the functional value of the PRODYNAMIC plantar orthosis with respect to the use of a more conventional multi-layer pro-ergonomic foot-insole.
Using a simple and analytical off-line reassessment of the postural attitude (VPA = Visual Postural Analysis) and an equally analytical objective evaluation of the global dynamic gait assessment (VGA = Visual Gate Analysis), we were also able to demonstrate the pro-adaptive value of our dynamic foot orthesis with respect to the condition of baseline normality. In detecting from T1 to T2 a partial improvement in postural attitude, symmetries of size triangles, scapulohumeral girdles and of the anterior-superior iliac spines, we clearly underlined the pro-functional value of its response to rehabilitation treatment proposed, taking into account that the characteristic progression and structuring of parkinsonian symptomatology makes the postural attitude of the individual only partially modifiable. In detecting from T1 to T2 a partial normalization of the overall analytical gait schema of our sample patients, it is evident that the use of a propulsive high facilitation device (Prodynamic insole) has not only normalized the control of the stance and push-off phase of the step, but also managed to modify the control of the knee excursion and of the trunk-pelvis unit. Even more evident was the ability of the custom-made device used (Prodynamic insole) to facilitate a real process of gait re-learning, resulting from the modulable pro-dynamic properties of the orthosis used.
In summary, the baropodometric and kinematic analysis data obtained at the end of our study have highlighted the ability of the Prodynamic plantar to stimulate walking speed and step length that we have not observed using the conventional synthetic insole in a more or less similar manner in the two groups of recruited Parkinsonian patients (P and PS). Infact, results obtained in the Parkinson group clearly showed a more complex physiopathological and syndromic heterogeneity of this disease, demonstrating that a simple and isolated orthotic foot insole treatment could be ineffective in the remodulation of the balance strategies control and of the gait pattern. We believe that physiotherapist need to support in the future work their rehabilitative work by using with a critical point of view dynamic orthopedic systems (PRODYNAMIC FOOT-INSOLE) that allowes to reach 3 fundamental rehabilitative goals:
• peripheral neuromodulation of the gait cycle;
• rehabilitative facilitation of a modulable gait and postural re-learning process (embodyment re-modulation);
• improvement of the qualitative profile of the patient’s life.
It is clear that this innovative dynamic foot-insole called “Prodynamic” can be considered, in the treatment of patients with Parkinson’s, a low-cost strategy to improve postural stability and the quality of the gait pattern. The Figure of the orthopedic technician will therefore be able to play a new role within the rehabilitation team by offering innovative technical devices in the treatment of patients affected by Parkinson’s disease. The high profile of complexity and clinical-dysfunctional heterogeneity of Parkinson’s disease have certainly influenced the number of our study sample. For this reason, the design of our study included specific inclusion and exclusion parameters that led us to the strict selection of 2 specific groups of patients: Parkinson group and Parkinsonism group. In relation to the scholastic duration of our study, the 2 groups were certainly not numerous but at the same time homogeneous in their intrinsic characteristics and therefore ideal for analyzing their different response to the orthotic plantar treatment proposed in our study. In a future work, our aim will be to focus the proposed study model on a larger sample of studies although homogeneous in the characteristics that delineate the two types of extrapyramidal disease examined (PD and parkinsonism), in order to test the real statistical significance of the kinematic and clinical outcome parameters considered in this pilot study.
References
- Duncan GW, Khoo TK, Coleman SY, Brayne C, Yarnall AJ, et al. The incidence of Parkinson's disease in the North-East of England. Age Ageing. 2014; 43: 257-263. Ref.: https://tinyurl.com/y29nohjb
- Ylikotila P, Tiirikka T, Moilanen JS, Kääriäinen H, Marttila R, et al. Epidemiology of early-onset Parkinson's disease in Finland. Parkinsonism Relat Disord. 2015; 21: 938-942. Ref.: https://tinyurl.com/y43ejmet
- Chang A, Fox SH. Psychosis in Parkinson's Disease: Epidemiology, Pathophysiology, and Management. Drugs. 2016; 76: 1093-1118. Ref.: https://tinyurl.com/y5hksobx
- Raza C, Anjum R, Shakeel NUA. Parkinson's disease: mechanisms, translational models and management strategies. Life Sci. 2019; 226: 77-90. Ref.: https://tinyurl.com/yywh2v4z
- Ullah MF, Ahmad A, Bhat SH, Abu-Duhier FM, Barreto GE, et al. Impact of sex differences and gender specificity on behavioral characteristics and pathophysiology of neurodegenerative disorders. Neuroscience Biobehavioural Review. 2019; 102: 95-105. Ref.: https://tinyurl.com/y6zdcr6n
- Caggiu E, Arru G, Hosseini S, Niegowska M, Sechi G, et al. Inflammation, Infectious Triggers, and Parkinson's Disease. Front Neurol. 2019; 10: 122. Ref.: https://tinyurl.com/y6bqswq8
- de Lau LM, Giesbergen PC, de Rijk MC, Hofman A, Koudstaal PJ, et al. Incidence of parkinsonism and Parkinson disease in a general population: the Rotterdam study. Neurology. 2004; 63: 1240-1244. Ref.: https://tinyurl.com/y2dax3ol
- Caslake R, Taylor K, Scott N, Gordon J, Harris C, et al. Age-, gender-, and socioeconomic status-specific incidence of Parkinson’s disease and parkinsonism in northeast Scotland: the PINE study. Parkinsonism Relat Disord. 2013; 19: 515-521. Ref.: https://tinyurl.com/yyqjder5
- Hirsch L, Jette N, Frolkis A, Steeves T, Pringsheim T. The incidence of Parkinson’s disease: a systematic review and meta-analysis. Neuroepidemiology. 2016; 46: 292-300. Ref.: https://tinyurl.com/y5mq8x75
- De Rijk MC, Tzourio C, Breteler MM, Dartigues JF, Amaducci L, et al. Prevalence of parkinsonism and Parkinson's disease in Europe: the EUROPARKINSON Collaborative Study. European Community Concerted Action on the Epidemiology of Parkinson's disease. J Neurol Neurosurg Psychiatry. 1997; 62: 10-15. Ref.: https://tinyurl.com/y3uc9xxj
- Ascherio A, Schwarzschild MA. The epidemiology of Parkinson's disease: risk factors and prevention. Lancet Neurol. 2016; 15: 1257-1272. Ref.: https://tinyurl.com/yyu838tq
- Jenkins ME, Almeida QJ, Spaulding SJ, van Oostveen RB, Holmes JD, et al. Plantar cutaneous sensory stimulation improves single-limb support time, and EMG activation patterns among individuals with Parkinson's disease. Parkinsonism Relat Disord. 2009; 15: 697-702. Ref.: https://tinyurl.com/y6qzqyk8
- Dorsey ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, et al. Tanner CM. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007; 30; 68: 384-386. https://tinyurl.com/y5r8f5mn
- Rahman S, Griffin HJ, Quinn NP, Jahanshahi M. On the nature of fear of falling in Parkinson's disease. Behav Neurol. 2011; 24: 219-228. Ref.: https://tinyurl.com/y5ln6wsm
- Schoneburg B, Mancini M, Horak F, Nutt JG. Framework for Understanding Balance Dysfunction in Parkinson’s Disease. Movement Disorders. 2013; 15; 28: 1474-1482. Ref.: https://tinyurl.com/y6dkgmws
- Qiu F, Cole MH, Davids KW, Hennig EM, Silburn PA, et al. Effects of textured insoles on balance in people with Parkinson's disease. PLoS One. 2013; 8: e83309. Ref.: https://tinyurl.com/y3zejdrb
- Rinalduzzi S, Trompetto C, Marinelli L, Alibardi A, Missori P, et al. Balance dysfunction in Parkinson's disease. Biomed Res Int. 2015; 2015: 434683. Ref.: https://tinyurl.com/yyh29tql
- Laessoe U, Voigt M. Anticipatory postural control strategies related to predictive perturbations. Gait Posture. 2008; 28: 62-68. Ref.: https://tinyurl.com/y3anghy3
- Visser JE, Bloem BR. Role of the basal ganglia in balance control. Neural Plast. 2005; 12: 161-174. Ref.: https://tinyurl.com/y6mgk8kd
- Brown LA, Cooper SA, Doan JB, Dickin DC, Whishaw IQ, et al. Parkinsonian deficits in sensory integration for postural control: temporal response to changes in visual input. Parkinsonism Relat Disord. 2006; 12: 376-381. Ref.: https://tinyurl.com/y6xfqqgg
- Lirani-Silva E, Vitório R, Barbieri FA, Orcioli-Silva D, Simieli L, et al. Continuous use of textured insole improve plantar sensation and stride length of people with Parkinson's disease: A pilot study. Gait and Posture. 2017; 58: 495-497. Ref.: https://tinyurl.com/y4wv4m66
- Comber L, Galvin R, Coote S. Gait deficits in people with multiple sclerosis: A systematic review and meta-analysis. Gait and Posture. 2017; 51: 25-35. Ref.: https://tinyurl.com/y2bhufjb