Research Article
Influence of an integrated rehabilitative treatment on the modification of body representation in patients affected by Unilateral Spatial Neglect

Maurizio Falso1*, Michela Delpero2 and Eleonora Cattaneo2
1Middle Cares Rehabilitation Unit, Fondazione Madonna del Corlo, Lonato (Bs), Italy
2Section of Neurological Rehabilitation, Clinical Institute Città di Brescia, Brescia, Italy
*Address for Correspondence: Maurizio Falso, MD, Physical Medicine & Rehabilitation, Middle Cares Rehabilitation Unit, Fondazione Madonna del Corlo, Corso Garibaldi 3, 25017, Lonato (Bs), Italy, Tel: 349.4971729; Email: [email protected]
Dates: Submitted: 19 November 2018; Approved: 10 December 2018; Published: 11 December 2018
How to cite this article: Falso M, Delpero M, Cattaneo E. Influence of an integrated rehabilitative treatment on the modification of body representation in patients affected by Unilateral Spatial Neglect. J Nov Physiother Rehabil. 2018; 2: 087-100. DOI: 10.29328/journal.jnpr.1001023
Copyright License: © 2018 Falso M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: : NSU; Body schema; Rehabilitative treatment of NSU.
Abbreviations: NSU: Unilateral Spatial Neglect; MMSS: Mini Mental Status Scale; MI: Motricity Index; TCT: Trunk Control Test; FAC: Functional Ambulation Category; BIT: Behavioural Inattention Test; PRC: Postural Reaction Control; UL: Upper Limb; LL: Lower Limb
Abstract
Background: In line with the so-called “embodiment concept”, human bodily experience is characterized by the immediate feeling that our body is localized in a certain position in space and that the self is localized within these body limits.
Aim: To verify in a cohort of patients affected by unilateral spatial neglect (NSU) secondary to cerebrovascular damage the possible correlation between a comprehensive neuromotor/neuropsychological rehabilitative treatment and the modification of body representation.
Setting: A rehabilitation institute for the treatment of neurological gait disorders and neuropsychological failures.
Methods: 12 patients (7 males, 5 females; mean age 60 ± 2yy) affected by NSU secondary to cerebral stroke and recovered in the Neurological Rehabilitation Section of the Clinical Institute Città di Brescia were recruited for the aim of this study. In accordance with our inclusion criteria we recruited 4 patients affected by ischemic stroke and 8 patients affected by haemorragic stroke; 9 patients of our study group arrived from a coma state period. Recruited patients underwent at time T0 (hospitalization day) to a functional impairment evaluation (Motricity Index = MI; Trunk Control Test = TCT; Functional Ambulation Category = FAC) and to a neuropsychological evaluation (Behavioural Inattention Test = BIT; Representional drawing; Personal Neglect evaluation scale); each evaluation was repeated in the same way at time T1 (intertime between 2 and 4 months after hospitalization) and time T2 (inter time between 5 and 6 months after hospitalization). At time T0 each patient began an individualized integrated (motor and neuropsychological) rehabilitative treatment course.
Results: In all patients recruited a statistical significant modification was observed for the MI LL left, the TCT and the FAC; no significant statistical modification was observed for the MI UL left, the MI UL and the MI LL right. The t-test showed a significant statistical modification of the personal neglect evaluation scale while no significant statistical modification was defined for the spontaneous human figure drawing test proceeding from time T0 to time T1. The spontaneous drawing of the human figure showed an individual different trend and modification in all patients recruited. A correlation analysis was made comparing the mean value of all motor scales (G1) with the mean value of all neuropsychological scales (G2) and no statistical significant correlation was observed between G1 (T0) and G1 (T1), G1 (T0) and G2 (T0), G1 (T0) and G2 (T1), G2 (T0) and G1 (T1), G2 (T0) and G2 (T1), G1 (T1) and G2 (T1). A second correlation analysis was made comparing all single motor scales with the neuropsychological scales, for the group made by 12 patients and the group made by 5 patients. For the group made by 12 patients, we observed the subsequently significant correlations: MI UL left (T0) correlates with MI LL left (T0); MI LL left (T0) correlates with MI LL left (T1); MI UL left (T1) correlates with MI LL left (T1); MI LL left (T1) correlates with FAC (T1); TCT (T1) correlates with FAC (T1). For the group made by 5 patients, we observed the subsequently significant correlation: TCT (T2) correlates with FAC (T2). In the group made by 12 patients, the mean amelioration of the time related normalized (T0-T1) motor scales is equal to 49% while to 63% was observed for the neuropsychological scales. The mean amelioration of the neuropsychological scale proceeding from time T0 to T1 is equal to 26% with an increase equal to 57% proceeding from time T1 to T2. The neurocognitive amelioration can be observed especially between the 5th and 6th month from the ischemic cerebral damage with a mean increase from 26% to 57%.
Conclusions: It would certainly make sense to treat patients with NSU from the neuropsychological point of view in the long term and from the neuro-motor point of view in the first 3-4 months after stroke; in all this, we cannot exclude that an improvement of the visuo-spatial exploration, emphasized by the neuropsychological treatment, can positively influence also patient’s motor outcome.
Introduction
The mental representation of our body allows us continuously to perform small and large gestures of daily life. Only when such gestural behaviors are altered by central neurological damage do we really realize how important they are in our daily activities. Disorders of body representation may be of psychopathological origin or a consequence of central neurological damage. A careful analysis of the literature [1-6] shows an unclear distinction between body schema and body image.
In 1935 Schilder stated: “the body image is the mental framework that we make of our body and the way our body appears to us; in addition to the sensory inputs that reach the brain, there is also the immediate experience of the existence of a body unit that, in addition to being perceived, is something more than a perception, that is a body schema; this body schema is not only a perception but a three-dimensional image that each has of himself, which in addition to the perception of the senses involves patterns and mental representations, even though it is not just a representation“.
In a recent review, Pernigo and Moro (2008) [5], observed that, next to clinical studies on patients with disorders of body representation, interesting experimental techniques have been developed in recent years that have allowed the study of abnormal body perceptions in healthy subjects. In the attempt to outline a distinction between body image and body schema, important fronts of study and theorization of the possible effects deriving from integrated neurorehabilitative therapeutic approaches have opened up.
The aim of the following retrospective study was to verify in a cohort of patients affected by unilateral spatial neglect (NSU) secondary to cerebrovascular damage the possible correlation between a comprehensive neuromotor/neuropsychological rehabilitative treatment and the modification of body representation.
Materials and Methods
Participants
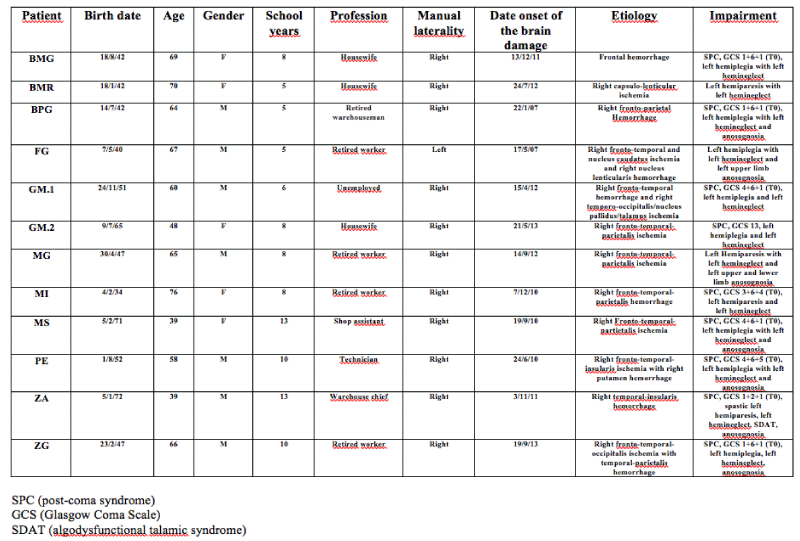
We selected our study group by performing a retrospective analysis of a court of patients affected by NSU secondary to hemisphere cerebral stroke and recovered in the Neurological Rehabilitation Section of the Clinical Institute Città di Brescia (Italy) in the period between 2007 and 2013. 12 patients affected by NSU secondary to cerebral stroke (7 males, 5 females; mean age 60 ± 2yy with an average amount of attended school years equal to 8.25yy ± 2.83; average score of Mini Mental Status Examination test equal to 20.67 ± 4.70) were recruited for the aim of this study. In accordance with our inclusion criteria (evidence of Unilateral Spatial Hemineglect, neuroradiological evidence of a right cerebral hemisphere stroke at basetime T0, intertime between the cerebral stroke event and the secondary hospitalization less than 1 month, MMSS score higher than 9, italian mother tongue), we recruited 4 patients affected by ischemic stroke and 8 patients affected by haemorragic stroke; 9 patients of our study group arrived from a coma state period. Table 1 resumes all clinical, daemographic and functional aspects of each recruited patient.
Table 1: Retrospective investigation and summary of personal data, date of the index event, etiology of brain injury, post-stroke functional impairment (own elaboration data).
Study design and outcome measures
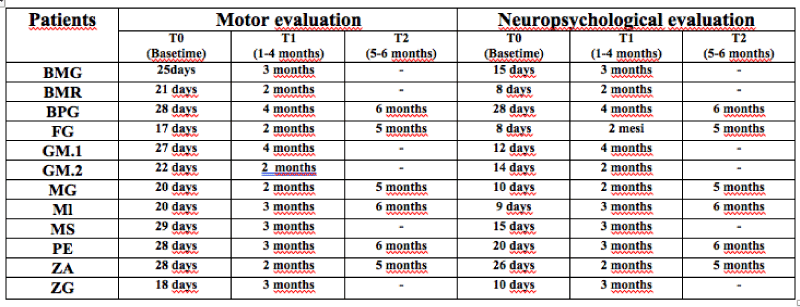
Recruited patients underwent at time T0 (hospitalization day)(Table 2) to a functional impairment evaluation (Motricity Index = MI; Trunk Control Test = TCT; Functional Ambulation Category = FAC) and to a neuropsychological evaluation (Behavioural Inattention Test = BIT; Representional drawing; Personal Neglect evaluation scale of Zoccolotti et al. [8], each evaluation was repeated in the same way at time T1 (intertime between 2 and 4 months after hospitalization) and time T2 (intertime between 5 and 6 months after hospitalization). At time time T0 each patient began an individualized comprehensive (motor and neuropsychological) rehabilitative treatment course.
Table 2: Resume of the time-related motor and neuropsychological evaluation of each patient recruited (own elaboration data).
Motor impairment evaluation items
Motricity Index (MI): This is an ordinal-type scale that, according to Collin & Wade’s studies, classify post-stroke motor impairment. Motricity is investigated, on both sides, through the request for fundamental movements for the daily life activities. For the upper limb, the ability to perform a pinch grip, flexion of the elbow and abduction of the shoulder are analyzed. The ankle dorsiflexion, knee extension and hip flexion are examined for the lower limb.
The maximum achievable score for each limb is 100.
The test is performed with the patient sitting on the edge of the bed, with the feet not touching the floor.
• Area of assessment: functional mobility.
Trunk Control Test (TCT): This is an ordinal scale that allows the assessment of balance and control of the trunk. The evaluated tasks are the postural supine-seated passage, turn in the supine position, on the healthy side and on the affected side and maintain the sitting position without supports for 30 seconds. Depending on how each of the four required tasks are performed, a score is assigned, differentiating between a movement that needs help from an assistant and a self-sufficient movement with or without the need to cling to the bed .The total sum of the scores can reach a maximum score of 100.
. Area of assessment: functional mobility.
Functional Ambulation Category (FAC): The FAC is a tool for measuring the ambulatory capacity developed in 1986 by Holden M.K. and colleagues. It is an ordinal scale comprising five classes. This subdivision takes into account specific criteria, related to both the functionality of the path and the characteristics of the surface of the ground where it is practiced.
. Area of assessment: functional mobility, gait.
Neuropsychological impairment evaluation items: The evaluation of each patient was conducted by a single neuropsychologist in the Neurological Rehabilitation Department and in the presence of each single patient recruited in our study. Each patient of the study sample was subjected by the Neuropsychologist alone to a battery of tests for a total duration of 1 hour of evaluation, data collection related to each test and task-specific treatment of each patient. The data collected at the end of the sequential administration of the tests chosen for the purposes of our study were archived on a special file, individually appointed for evaluation tests. At the end of the study period and the collection of the selected neuropsychological data, they were processed and submitted to statistical analysis in the presence and sharing of the study physiotherapist for the delineation of the expected results.
For the aim of the study, a test belonging to the BIT (Behavioral Inattention Test) battery was taken into consideration: the spontaneous drawing of the human figure forming part of the representative drawing. This test is the most “representative”, in that the patient has to access his own internal representations of the human person before drawing it.
Representational drawing:
Task: This subtest consists of three tests. The patient is asked to draw a clock, then a human figure, and finally a butterfly on three different sheets, A4 size. The drawings are made to run on three different sheets.
Instructions: 1. “I would like you to draw freehand on this sheet: the big dial of a watch. Put the clock numbers and set an hour. “2.”Draw the figure of a man or woman seen from the front”. 3. “I would like you to draw a butterfly”
Score: The score to be assigned is 1 for each drawing if it appears substantially symmetrical.
Personal hemineglect evaluation scale:
The examiner evaluates three tasks:
1. The subject is given a comb (or brush) and is asked to comb:
“Can you show me how to comb your hair?”
2. Subject-Woman: a powder case is supplied to the subject and is delivered to the subject asked to get inspired: “Does he show me how to put the powder?” Subject-Man: a razor with a safety cap is provided and he is asked to shave: “Does he show me how to use the razor?”
3. The subject is asked to wear glasses: “Does he show me how to put on his glasses?”
The number of “blows” to the right and left must be counted in order to arrive at a judgment on the symmetry of execution of the task.
The score reflects the level of asymmetry in the exploration of personal space: 0 is the absence of asymmetry, 1 mild, 2 moderate, 3 severe right-left asymmetry in the exploration of personal space.
No feedback should be given on the correctness of the task or to encourage completion of the service.
1. Combing score / 3
2. Get the Beard / Powder score / 3
3. Put the Spectacles score / 3 Maximum score: 9, Cut off: 2
Score attribution:
0 (Normal performance): the subject combs / shaves / powder on both sides of the head / face without evident asymmetries or however its performance is explicable in terms of its left plegia. The subject puts on the glasses correctly.
1 (slight deficit): the subject combs / shaves / powder on both sides but completes the left side only after an obvious hesitation. The subject puts on the glasses incorrectly (left) but corrects his performance after a hesitation.
2 (Medium Deficit): the subject combs / shaves / only powder on the right side and in the center but omits in a clear way the left side of the head / face in a way not justifiable by the use of one hand. The subject wears the glasses incorrectly on the left pavilion, but the lenses are sufficiently centered on the eyes.
3 (severe deficiency): the subject combs / shaves / only powder the right part of the head / face.
The subject puts the glasses incorrectly on the left pavilion and the lens on the left is not centered on the eye.
Clinical and functional evaluation model of stroke patients
After a global evaluation of patient’s primary daily living and care-giving needs, the physiatrist analyzed the neuropsychological and neuromotor profile of each patient recruited, focusing his attention on:
. Neuropsychological disfunctions
a) Aphasia: a general evaluation of patient’s speech functions;
b) Apraxia: a general evaluation of patient’s task-specific gestural profile;
c) Agnosia: a general evaluation of patient’s personal, peripersonal and extrapersonal visual and motor exploration;
. Swallowing disfunctions
a) Selective lips and toungh motor function;
b) Deglutition test with liquids and solids;
. Neuromotor disfunctions
a) Clinostatic postural assessment;
b) Passive multisegmental joint and muscle tone assessment;
c) Active limb muscle recruitment evaluation with a particular attention to the kinestesic profile of limb movement;
d) Superficial and deep multisegmental sensibility statement evaluation
e) Postural Reaction Control (PRC) evaluation from lying to sitting position; feedback and feedforward trunk postural control evaluation, focusing the attention on patient’s individual sense of position;
f) Starting from a functional core-stability control, Postural Reaction Control (PRC) assessment from sitting to standing position with or without aids;
g) Starting from a functional control of core-stability, orthostatic and orthodynamic performance assessment, focusing the attention on patient’s orthostatic proprioceptive and gait cycle control with or without aids.
Neuropsychological evaluation model of post-stroke hemineglect and body image
In line with our standardized and daily neuropsychological evaluation procedure of the hemineglect and body image, in which we analyze the peripersonal hemineglect (B.I.T = Behavioural Inattention Test and Sentences lecture) [9,10], the personal hemineglect [8], the extrapersonal hemineglect (Environment description) [8] and the anosognosia (Anosognosia evaluation scale) [11], we focused our attention on two evaluation items: a. the personal hemineglect evaluation scale; b. the human figure drawing, which represents a part of the so-called “Representational drawing test” of the BIT battery.
Neurorehabilitative treatment procedure
At time T0 and the end of each patient’s functional evaluation, the physiatrist:
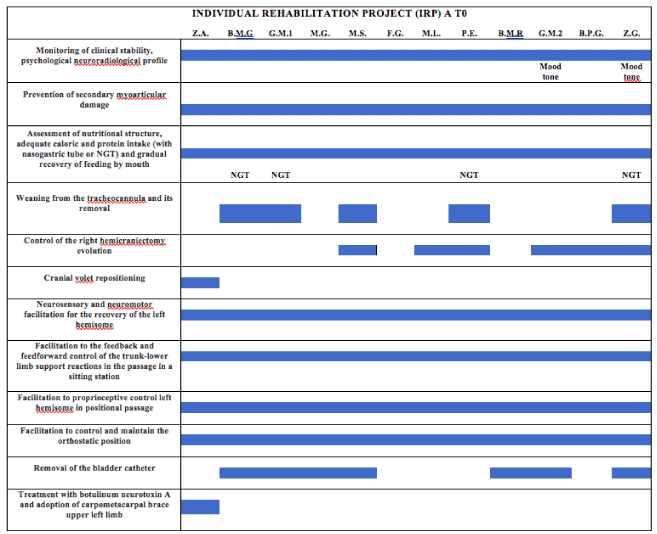
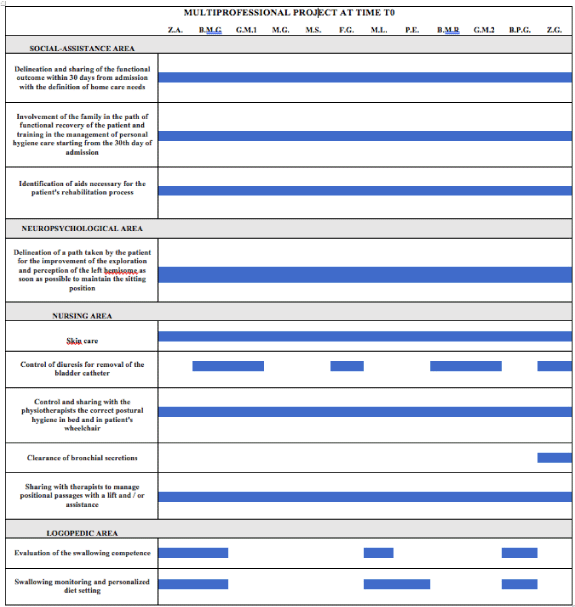
a) drawed up an individual rehabilitative project for each recruited patient with related functional goals (Table 3a).
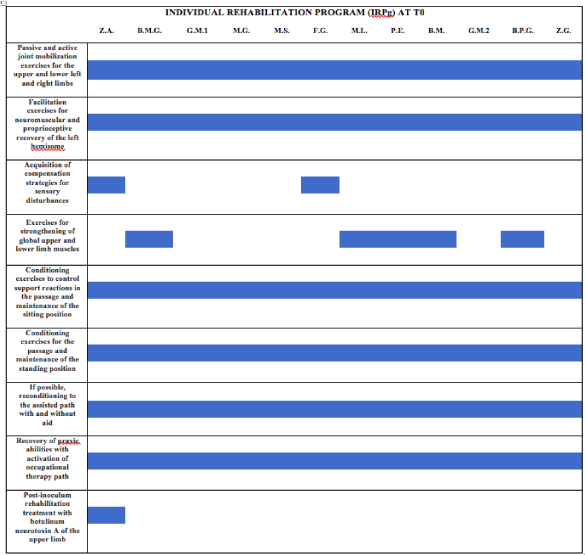
b) drawed up and individual rehabilitative exercises program for each recruited patient (Table 3b).
c) drawed up a multiprofessional rehabilitative project for each recruited patient with the identification of all professional figures needed to realize our functional rehabilitative goals (Table 3c).
Table 3a: Individual rehabilitative project for each patient at T0 time (in blue identification of proposed objective for each patient (own elaboration).
Table 3b: Individual rehabilitative program for each patient at T0 time (in blue identification of proposed exercises for each patient (own elaboration).
Table 3c: Multi professional rehabilitative project for each recruited patient with the identification of all professional figures needed to realize the functional rehabilitative goals (own elaboration).
Patients underwent to a neurorehabilitative treatment course for 6 times per week with a duration of 1hour per rehabilitative session per day.
Neuropsychological treatment procedure
Recruited patients underwent to a neuropsychological rehabilitative treatment for 3 times per week, with a duration of 1 hour per rehabilitative session, by using: a. visual performance exploration with paper material or a PC (personal computer); b. perception and spatial mind exploration; c. lecture training with visual cues positioned on the left side of the lecture page; d. drawing copy on matrix points; e. description of figures and real environments.
Data analysis
Data analysis was made using the statistical software SPSS. Time related (T0-T1) intra-group modification of all motor scales and neuropsychological scales were analyzed using parametric one-sample t-test with an unknown variance. The significance leve was set to p<0,05. Subsequently, the Pearson correlation coefficient (p<0,05) was used to analyze the correlation between motor and neuropsychological variables, considered as single scales or motor (G1) and neuropsychological (G2) grouped scales after their normalization. The normalization of the study variables was made by using a calculation of the proportion in order to bring all values to a numerical scale from 0 to 100; “0” indicates a minimum function while “100” maximum function. Finally, the mean percentage amelioration of motor and neuropsychological performance was analyzed proceeding from time T0 to time T1 in all 12 patients of our study group and proceeding from time T0 to T1 and time T1 to T2 in 5 patients of them. This amelioration was calculated as mean value of the amelioration percentage of all motor scales (G1) and neuropsychological scales (G2). For all 12 patients was also evaluated the time related (T0-T1) significant difference between the mean value of all G1 scales and G2 scales.
Results
Post-rehabilitative clinical-functional results
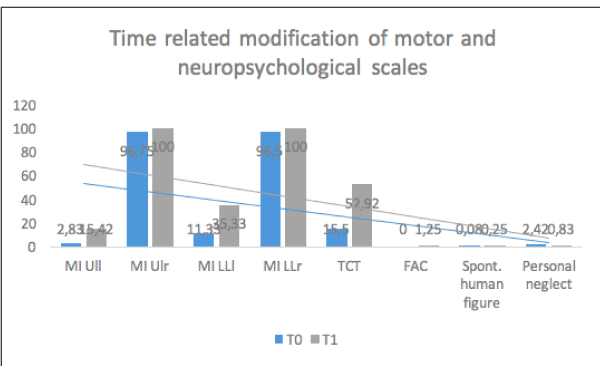
The parametric one-sample t-test evidenced in all 12 patients recruited a statistical significant modification proceeding from time T0 to time T1 for the following scales: MI LL left [t(11)=4,016; p<0,05], TCT [t(11) = 6,070; p<0,001], FAC [t(11)=5,000; p<0,001]. No significant statistical modification was observed for these following scales: MI UL left [t(11)=1,820; n.s.], MI UL right [t(11)=1,000 n.s.], MI LL right [t(11)=1,000; n.s.] (Figure 1).
Figure 1: Time-related modification (T0-T1) of mean values of motor and neuropsychological scales (own elaboration).
Post-rehabilitative neuropsychological results
The t-test showed a significant statistical modification of the personal neglect evaluation scale [t(11)=3,272; p<0,05], while no significant statistical modification was defined for the spontaneous human figure drawing test proceeding from time T0 to time T1 [t(11)=1,483; n.s.].
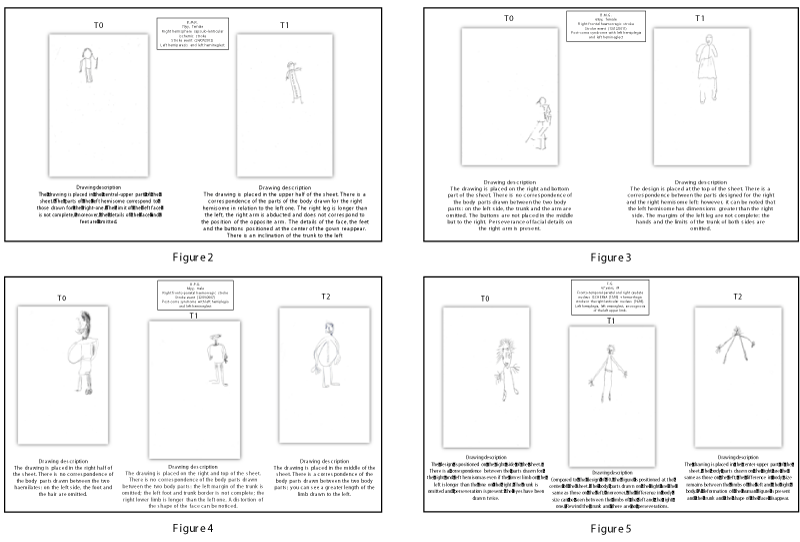
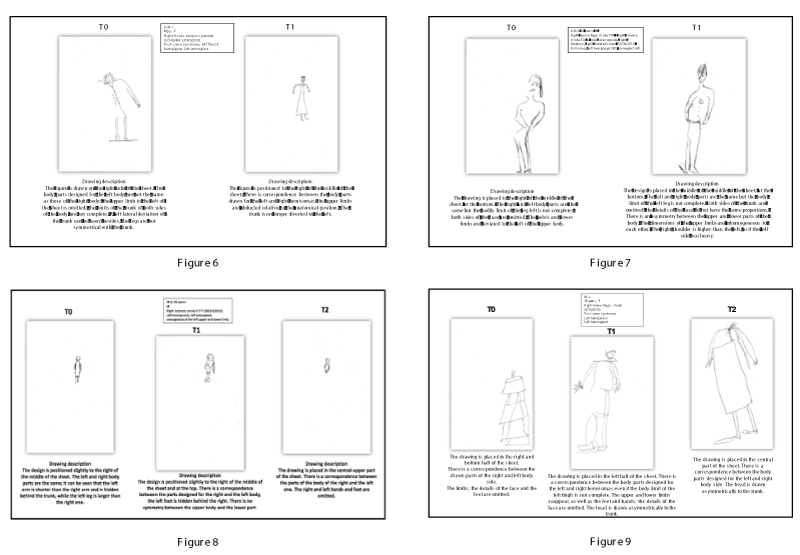
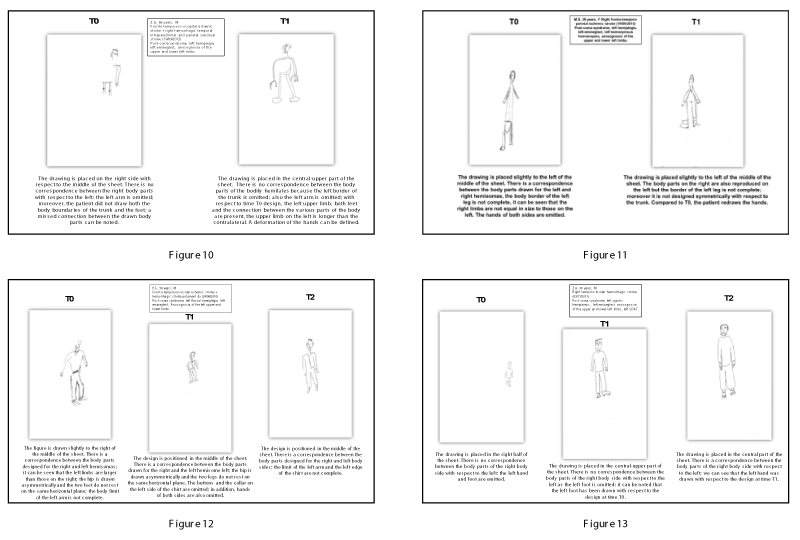
Comparative visual analysis of spontaneous drawing of the human figure
The spontaneous drawing of the human figure, which is part of the BIT has been assessed quantitatively through a score of 0-1 but also qualitatively taking into account two objective criteria: provision on sheet, proportions of the right and left body side (sprains, omissions, perseveration, allochiria of body parts). A visual comparative time-related analysis (time T0, T1 and T2) of spontaneous drawing of the human figure can be resumed for each patient from figures 2 to 13.
Comparative anlaysis of clinical/functional and neuropsychological data
A first correlation analysis was made comparing the mean value of all motor scales (G1) with the mean value of all neuropsychological scales (G2). Using the Pearson correlation coefficient no statistical significant correlation was observed between G1 (T0) and G1 (T1) [r=0,496; n.s.], G1 (T0) and G2 (T0) [r=-0,196; n.s.], G1 (T0) and G2 (T1) [r=-0,40; n.s.], G2 (T0) and G1 (T1) [r=-0,124; n.s.], G2 (T0) and G2 (T1) [r=0,408; n.s.], G1 (T1) and G2 (T1) [r=-0,077; n.s.]. A second correlation analysis was made comparing all single motor scales with the neuropsychological scales, for the group made by 12 patients and the group made by 5 patients. For the group made by 12 patients, we observed the subsequently significant correlations: MI UL left (T0) correlates with MI LL left (T0) [r=0,724; p<0,01]; MI LL left (T0) correlates with MI LL left (T1) [r=0,634; p<0,05]; MI UL left (T1) correlates with MI LL left (T1) [r=0,650; p<0,05]; MI LL left (T1) correlates with FAC (T1) [r=0,650; p<0,05]; TCT (T1) correlates with FAC (T1) [r=0,592; p<0,05]. For the group made by 5 patients, we observed the subsequently significant correlation: TCT (T2) correlates with FAC (T2) [r=0,901; p<0,05].
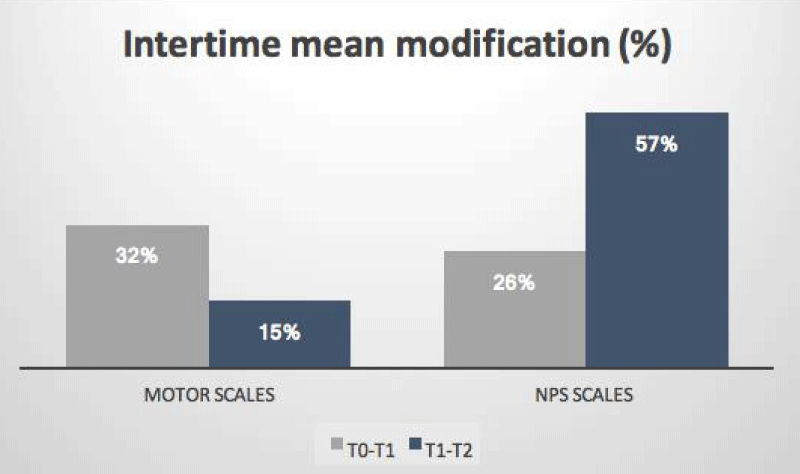
Time-related modification of clinical/function and neuropsychological data
In the group made by 12 patients, the mean amelioration of the time related normalized (T0-T1) motor scales is equal to 49% while to 63% was observed for the neuropsychological scales. Moreover, the t-test showed for the G1 motor scales a significant time-related (G1 T0-G1 T1) mean difference [t(11)=-5,629; p<0.001]. Similarly, the t-test showed for the G2 neuropsychological scales a significant time-related modification proceeding from time T0 to time T1 [t(11)=-2,405; p<0.05]. For the group made by 5 patients evaluated at time T0, T1, T2, we observed a mean amelioration of the motor scales equal to 32% proceeding from time T0 to T1 and equal to 15% proceeding from time T1 to T2. This result demonstrated that a motor impairment amelioration can be observed especially in the first 4 months from the ischemic cerebral damage with a decrease around the 5th and 6th month from the cerebral damage (mean amelioration from the 32% to 15%). The mean amelioration of the neuropsychological scale proceeding from time T0 to T1 is equal to 26% with an increase equal to 57% proceeding from time T1 to T2. This result demonstrated that the neurocognitive amelioration can be observed especially between the 5th and 6th month from the ischemic cerebral damage with a mean increase from 26% to 57% (Figure 14).
Discussion
Starting from a careful analysis of the literature, several neuropsychological studies [1,3] as well as considering the NSU as the inability to refer, respond, or orientate towards new or significant stimuli presented controlaterally to the cerebral lesion, is also considered as an alteration of body representation. The originality of our study stems from the fact that we have considered this particular aspect of neglect from a rehabilitative point of view, verifying the possible influence of a comprehensive rehabilitative-neuropsychological treatment on the body representation of our recruited patients. Furthermore, a singular aspect of our study is that we have examined an integrated rehabilitative-neuropsychological treatment approach and not just a rehabilitation method traditionally used in the treatment of NSU.
In line with the current literature, we believe that the statistically significant improvement of the clinical-functional data observed at the end of the integrated rehabilitation treatment can be interpretated as an expression of an improvement of the “body schema” achieved by our patients; in other words, we can interpretate this results as the consequence of an “interior remodeling” of the initiation and planning process of movements aimed at a purpose. The peripheral remodeling process of the body schema is now clearly identifiable in what experts call “central neuroplasticity”. We know that focused attention, conscious thinking, investigating in a relationship helps to reshape, at any moment of our life, the brain connections allowing us to bring integration into our “brain - mind” system. It is in this context that the importance of using exogenous stimuli, both motor and neurocognitive, is used to produce a remodeling of central synaptic connections that aim as much as possible towards pro-adaptive and non-maladaptive functional results. The modulated and controlled integration of both motor and neuropsychological facilitations have in a simple and procedural manner characterized our study leading to results that in addition to improving the motor performance of each patient of our sample have also wonderfully changed the central representation of their body schema.
Moreover, with the t-test we also highlighted the significant functional modification, secondary to our comprehensive rehabilitative treatment and proceeding from time T0 to time T1, of the left lower limb performance, of the trunk balance control and of patient’s gait cycle; no amelioration was observed for the left upper limb motor performance. In line with the literature [11], this post-rehabilitative response can be resumed as the expression of a central somatotopic representation of the body schema that would see the lower limb and trunk more sensitive to a functional treatment-related change (treatment-induced adaptive neuroplasticity).
From a neuropsychological outcome point of view, our comprehensive rehabilitative treatment model has clearly statistically influenced the exploration of personal/peripersonal space and of body awareness (perception of one’s posture and postural proprioception); in the same way, the treatment did not affect the time-related modification of the body image expressed by each patient through the Representional Drawing test and quantified by a score 0-1.
The discrepancy between objective and parametric performance secondary to the drawing test would lie: a. in the type of dichotomous score of the test used, which would make it less sensitive to the degree of assessment of a body image; b. in the low number of the study sample recruited.
The parametric correlational analysis between the clinical and functional scales adopted in this study could demonstrate how not only the recovery of the left lower limb motility and of the trunk control can influence the improvement of patient’s path, but also how (vice versa) the parametric quantification in the short and long term of these performances may be a predictive condition for a possible recovery of the pathway in patients affected by NSU. Contrarily, in line with the correlational parametric analysis between neuromotor and neuropsychological scales, the absolute lack of a relationship between the personal neglect trend and patient’s motor performances was observed. We can deduce that a high degree of personal neglect does not influence the performance of the spontaneous drawing of the human figure and vice versa; moreover, this lack of relationship between personal neglect and representative neglect (assessed by spontaneous design) may be in accordance with the clinical dissociation between these two types of neglect found in the literature [12]. We can also hypothesize that a negative score in the human figure’s drawing test may not be a predictive tool for the motility of the left hemisome; in other words, not necessarily if a patient has a motor scale with a low score, he also has a negative score in the spontaneous drawing of the human figure.
The long-term analysis (proceeding from time T0 to T2) of 5 patients of our sample, showed an interesting amelioration trend in both clinical/functional and neuropsychological profile, with increased motor performances especially found in the first 4 months after from the cerebral stroke event and an amelioration of patient’s neuropsychological profile after 4 months from the stroke event.
Further studies are needed to clearly outline the neuropsychological recovery times of patients affected by NSU, with the aim of defining the methods and timing of the most appropriate integrated treatment pathways to be proposed. If our study hypothesis were correct, it would certainly make sense to treat patients with NSU from the neuropsychological point of view in the long term and from the neuromotor point of view in the first 3-4 months after stroke; in all this, however we cannot exclude that an improvement of the visuo-spatial exploration, emphasized by the neuropsychological treatment, can positively influence also patient’s motor outcome.
References
- Gallagher S, Brosted S. Experimenting with phenomenology. Consciousness and Cognition. 2005; 15: 119-134. Ref.: https://goo.gl/UgwHJc
- De Vignemont F. Body schema and body image – pros and cons. Neuropsychologia. 2010; 48: 669-680. Ref.: https://goo.gl/UigtsX
- Coslett HB. Evidence for disturbance of the body schema in neglect. Brain Cogn. 1998; 37: 527-544. Ref.: https://goo.gl/4FuVDz
- Kammers MPM, Van der Ham IJM, Dijkerman HC. Dissociating body representations in healthy individuals: differential effects of a kinaesthetic illusion on perception and action. Neuropsychologia. 2006; 44: 2430-2436. Ref.: https://goo.gl/r4wP5s
- Moro V, Urgesi C, Pernigo S, Lanteri P, Pazzaglia M, et al. The neural basis of body form and body action agnosia. Neuron. 2008; 60: 235-246. Ref.: https://goo.gl/2Gd3vL
- Jackson SR, Buxbaum LJ, Coslett HB. Cognitive neuroscience of bodily representations: psychological processes and neural mechanisms. Cogn Neurosci. 2011; 2: 135-137. Ref.: https://goo.gl/1Fq9b4
- Zoccolotti P, Antonucci G, Judica A. Psychometric characteristics of two semi-structured scales for the functional evaluation of hemi-inattention in extrapersonal and personal space. Neuropsychological Rehabilitation. 1992; 2: 179-191. Ref.: https://goo.gl/mComgC
- Wilson B, Cockburn J, Halligan P. Development of behavioural test of visuospatial neglect. Arch Phys Med Rehabil. 1987; 6: 98-102. Ref.: https://goo.gl/PRrDjH
- Pizzamiglio L, Cappa S, Vallar G, Zoccolotti P, Bottini G, et al. Visual neglect for far and extra-personal space in humans. Cortex. 1989; 25: 471-477. Ref.: https://goo.gl/gmo24o
- Berti A, Làdavas E, Della Corte M. Anosognosia for hemiplegia, neglect dyslexia and drawing neglect: clinical findings and theoretical considerations. J Int Neuropsychol Soc. 1996; 2: 426-440. Ref.: https://goo.gl/Gc4eky
- Morasso P, Casadio M, Mohan V, Rea F, Zenzeri J. Revisiting the body-schema concept in the context of whole body postural focal dynamics. Front Hum Neurosci. 2015; 17: 9-83. Ref.: https://goo.gl/pKMD66
- Kerkhoff G, Schenk T. Rehabilitation of neglect: an update. Neuropsychologia. 2012; 50: 1072-1079. Ref.: https://goo.gl/NwkthN