Research Article
Perceptive and Rehabilitative Muscle Recruitment Facilitation Secondary to the use of a Dynamic and Asymmetric Spine Brace in the treatment of Adolescent Idiopathic Scoliosis (AIS)

Maurizio Falso1*, Laura Forti2, Silvia Iezzi3, Gloria Cottali4, Eleonora Cattaneo5, Marco Zucchini6 and Franco Zucchini6
1Middle Cares Rehabilitation Unit – Fondazione Madonna del Corlo - Lonato (Bs), Italy
2Middle Cares Rehabilitation Unit – Fondazione Richiedei – Gussago (Bs), Italy
3PhT Freelance – Bergamo, Italy
4PhT Freelance – Iseo, Italy
5Section of Neurological Rehabilitation, Clinical Institute Città di Brescia, Brescia, Italy
6Poliortopedia Srl, Brescia, Italy
*Address for Correspondence: Maurizio Falso (MD), Physical Medicine and Rehabilitation, Middle Cares Rehabilitation Unit – Fondazione Madonna del Corlo – Corso Garibaldi 3, 25017, Lonato (Bs), Italy, Tel: 349.4971729; Email: [email protected]
Dates: Submitted: 15 May 2018; Approved: 01 June 2018; Published: 04 June 2018
How to cite this article: Falso M, Forti L, Iezzi S, Cottali G, Cattaneo E, et al. Perceptive and Rehabilitative Muscle Recruitment Facilitation Secondary to the use of a Dynamic and Asymmetric Spine Brace in the treatment of Adolescent Idiopathic Scoliosis (AIS). J Nov Physiother Rehabil. 2018; 2: 054-079. DOI: 10.29328/journal.jnpr.1001021
Copyright License: © 2018 Falso M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Adolescent idiopathic scoliosis; Spine brace; Paraspinal muscles myoelectric activity
Abstract
Background: Supporting our adolescent people in realizing his/her self ability to reorganize and to establish a cross-linked paraspinal muscle control can be considered the most effective approach for muscle rehabilitation in adolescents affected by “AIS. Aim of this study was to evaluate the SEMG activity of paraspinal erector muscles by using an innovative dynamic and asymmetric spine brace called “BRIXIA” in the conservative treatment of patients affected by adolescent idiopathic scoliosis (AIS).
Methods: Five patients affected by adolescent idiopathic scoliosis were recruited for the aim of this study in line with an informed consent and simple inclusion criteria. Each patient underwent a first task-specific evaluation at time T0 and T1 and a secondary experimental course at time T2, T3 and T4. After a first postural and total spine X-ray evaluation, recruited patients began to use our innovative spine brace called BRIXIA (time T0 and T1). During the second experimental phase, a SEMG bilateral activity of the trunk large rhomboid, the latissimus dorsi and the quadratus lumborum was investigated without spine brace, by using a common Chenêau brace and afterwards the dynamic BRIXIA spine brace, with the acquisition of the so-called RMS SEMG Ratio value. The SEMG measurements were acquired in six study conditions: a. SiRP=Sitting Resting Position; b. SiRCP=Sitting Recruiting Position with a so-called pneumothorax thrust; c. StRP = Standing Resting Position; d. StRCP = Standing Recruiting Position; e. BA = Anterior Trunk Bending; f. BARC = Anterior Trunk Recruiting Bending. At the end of this SEMG evaluation, each patient received (for a daily use around 18 hours per day) the final version of the BRXIA spine brace and began an individualized educational postural rehabilitative treatment course (time T2). At time T3 and T4 a second and third SEMG assessment was made without using a spine brace and by using BRIXIA, with each patient evaluated in a resting condition and realizing a self-made cross-linked postural correction. Finally, a functional, radiographic and postural evaluation were made to define and quantify an amelioration and modification of patients’ postural attitude at the end of a combined rehabilitative and device supported treatment.
Findings: A comparative analysis of our SEMG data acquired in six study conditions showed different trends in all patients recruited proceeding from time T2 to time T5. Particularly, we observed at time T2 an homogeneous grade of paraxial muscle recruitment acquisition, expressed by the RMSsEMG ratio index, without using spine brace (53,3%) and by using Chêneau and BRIXIA brace (46,7%); specifically, a 57,14% of our patients used BRIXIA brace and a 42,86% Chêneau brace; the most homogeneous response was acquired in BA study condition; a symmetric paraxial muscle recruitment acquisition without using spine brace was observed in an 80% of our patients; the most grade of not homogeneous muscle activity response was observed in SiRP and StRCP study conditions; at time T3, an homogeneous grade of symmetric paraxial muscle recruitment activity, expressed by the RMSsEMG ratio index, was observed by using BRIXIA brace (56,7%); all patients recruited (100%) showed in SiRCP study condition the most homogeneous and symmetric paraxial muscle recruitment by using BRIXIA brace; in SiRP and StRCP study condition this trend was observed in an 80% of our patients with a reversion of this trend in StRP and BRAC conditions; at time T4, an immodification of the grade of symmetric paraxial muscle recruitment acquisition, expressed by the RMSsEMG ratio index, was observed in a 56,7% of patients who were using BRIXIA brace; all patients recruited (100%) showed in BARC study condition the most homogeneous and symmetric paraxial muscle recruitment by using BRIXIA brace, while in SiRP condition this trend was observed in an 80% of our patients. In a comparative and time-related analysis between our clinical and RMS data, Cobb angle trend showed a statistical significant correlation with RMS data, acquired at time T4 in BARC condition and without BRIXIA brace, and similarly with RMS data acquired at time T4 with BRIXIA brace. In line with the Visual Postural Analysis trend, our rehabilitative model showed a sensible capacity to modify patient’s individual sense of posturality, to increase the acquisition of cross-linked self-correction strategies and to induce a progressive rebalancing between the anterior and posterior kinetic muscle chains recruitment. These rehabilitative principles were perfectly in line with the perceptive and pro-rehabilitative value of our innovative BRIXIA brace.
Interpretation: This study will underline the professional attitude of all physiotherapists to use in a critical and task-specific way our dynamic and asymmetric spine orthesis called “BRIXIA”. This innovative brace allows to achieve: a. an individualized peripheral neuromodulation of patient’s sense of postural attitude (peripheral perceptive re-modulation of paraxial muscle recruitment); b. a neurorehabilitative re-learning device of postural self-correction strategies (peripheral neurosensitive facilitation of a dynamic process of motor corticalization device-related); c. an increase of patient’s quality of life in term of appearance and relational sense (life-impact device-related).
Introduction
Adolescent idiopathic scoliosis (AIS) is one of the most common spine dysmorphism, which occurs in 1 to 4% of adolescent people with a prevalence in females who have a risk of curve progression 10 times higher than males [1-5]. Ginet Navarro said: “the attitude of a patient affected by adolescent idiopathic scoliosis is an attitude in front of life; the treatment of the first will change the second one”. In this way, Ginet Navarro evidenced the delicate psychological and social implication of this pathology in adolescents’ daily life. “Idiopathic” means that in an 80 to 85% of all scoliotic spine deformities an underlying cause cannot be defined. The three main determinants of progression of “AIS” are patient gender, future growth potential and curve magnitude at time of diagnosis. From a clinical point of view, “AIS” can be considered as a sign of a complex syndrome with a multifactorial pathogenesis. Multiple abnormalities have been found, yet none has been conclusively linked to all cases. Currently, around 43% of all idiopathic scoliosis forms showe a genetic predisposition, while other forms are secondary to multisegmental disperceptive disturbances and to neuromuscolar and dismetabolic deseases. Apart from its severity and modality of presentation, first of all idiopathic scoliosis allowes the upright posture expressed by a maladaptive form of trunk muscle balance. Secondary, the compensoratory profile of AIS is always secondary to an asymmetric paraspinal muscle activity. Third, we cannot ignore how “AIS” origin is influenced by the adaptive and defensive biomechanical role of the anterior and posterior trunk muscle chain. Many conservative or more invasive treatment options are available for adolescent idiopathic scoliosis but “prevention” (primary, secondary and tertiary prevention) remains one of the most important educational goals that clinicians need to realize. From this point of view, the postural rehabilitative treatment remains the basic option in the preventive treatment attitude for “AIS”. Supporting our adolescent people in realizing his/her self ability to reorganize and to establish a coss-linked paraspinal muscle control can be considered the most effective approach in adolescents affected by “AIS”. A clinical review of Berdishevsky and et al. [6] allows to compare, in line with the European SOSORT guidelines, different rehabilitative educational approaches. To support and to guide the effectiveness of a cross-linked paraspinal muscle control during an educational rehabilitative treatment of “AIS”, different studies tried to describe the SEMG signals of the trunk muscles in braced and unbraced conditions under different muscle contractions and underlying to different trunk excercises [7-13]. Kwok et al. [14] proposed a very original and significative point of view to support the purpose of our study. Evaluating the myoelectric activity of paraspinal muscles in adolescents with idiopathic scoliosis during habitual standing and sitting positions, the authors observed that RMS (root-mean-square) SEMG values of the paraspinal muscles reflect the spine curvature situation of adolescents with AIS. Particularly, a stronger average RMS SEMG value (muscle activation and recruitment amplitude) was found on the convex side of the affected muscle regions of spine: correction and an educational re-learning of posture as instructed by expert physiotherapists can help to achieve a more balanced RMS SEMG ratio in the paraspinal muscle recruitment of adolescent people with AIS. The aim of this study was to evaluate the grade and modality of cross-linked SEMG activity of paraspinal erector muscles by using an innovative dynamic and asymmetric spine brace called “BRIXIA” in the conservative treatment of patients affected by adolescent idiopathic scoliosis (JIS).
Methods
Subjects
Five patients (females; mean age 13,2 +/- 3.03yy) affected by adolescent idiopathic scoliosis and evaluated in the Ambulatory of Severe Infant Movement and Age Development Disorders of the Clinical Institute of Città di Brescia were recruited for the aim of this study. An informed consent and simple inclusion criteria (under 18 years old, affected by juvenile idiopathic scoliosis with a single or double spine curve and own angle of spine rotation, able to a re-learning and educational postural rehabilitative course, radiographic evidence of Adolescent Idiopathic Scoliosis, Risser ≤ 3; Cobb degrees ≥15°) were considered. At baseline (time T0), a clinical and functional evaluation of all patients was made (Tables 1,2). We recruited patients affected by AIS only and candidated to use our dynamic and asymmetric spine brace called “BRIXIA”, provided by the Prosthetic and Orthothic Lab - Poliortopedia S.r.l (Brescia).
| Table 1: Overview of the study population: age, gender, Risser classification and Cobb degrees. | ||||
| Name | Age | Gender | Risser Classification | Cobb angle |
| N.M | 12 | F | 2-3 | 28° |
| F.L | 17 | F | 4 | 14° |
| E.P | 15 | F | 2-3 | 28° |
| M.F | 12 | F | 2 | 28° |
| S.S | 9 | F | 0-1 | 20° |
| Table 2: Overview of the study population: presence or absence of menarche, use of orthodontic devices, use of glasses, radiographic identification of type of main and compensative spine curve and angle of spine rotation in anterior trunk bending. | ||||||
| Name | Menarche | Orthodontic Device | Glasses | Type of main curve | Type of conservatory curve | Angle of spine rotation |
| M.N. | No | Yes | No | Thoracolumbar left convex “S italica” | Thoracic right convex and cervical left convex | 11° |
| L.F. | Yes | No | Yes(myopia and astigmatism) | Thoracic right convex | Lumbar left convex | 9° |
| P.E. | Yes | Yes | No | Thoracolumbar right covex | // | 9° |
| F.M. | No | No | No | Thoracolumbar left “S italica” | Thoracic right convex | 13° |
| S.S. | No | Yes | Yes(myopla) | Thoracolumbar left convex “S italica” | Thoracic right convex | 10° |
Study design and evaluation procedure
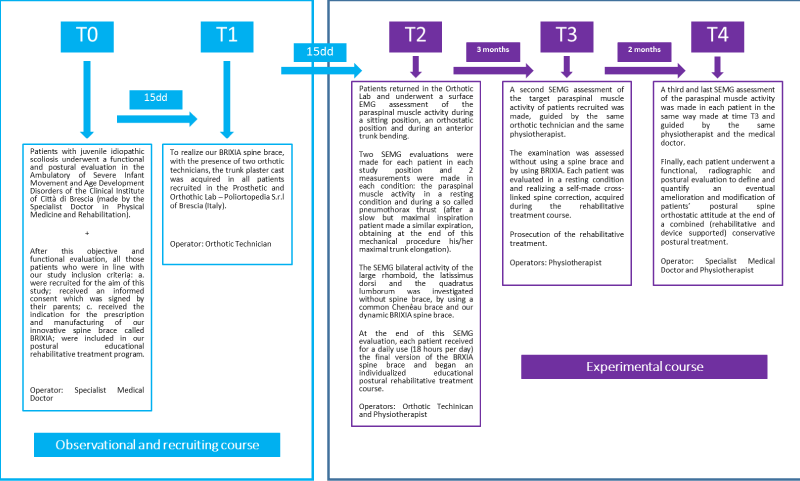
In line with a personalized operating flow-chart (Figure 1), each patient underwent a first task-specific evaluation and recruiting course at time T0 and T1 and a secondary experimental course at time T2, T3 and T4.
Figure 1: Model of our personalized study operating flow-chart design with an observational phase (blue line marked) and an experimental phase (red line marked) (own elaboration).
Observational and recruiting course
a. T0 (baseline)
Patients with adolescent idiopathic scoliosis underwent a functional and postural evaluation in the Ambulatory of Severe Infant Movement and Age Development Disorders of the Clinical Institute of Città di Brescia (made by the Specialist Doctor in Physical Medicine and Rehabilitation). The postural evaluation was made in static and dynamic condition and in three postural attitudes: orthostatic trunk attitude, anterior bending trunk attitude and in a clinostatic attitude to measure lower limb lenght. An ortostatic radiographic spine exam was also required in all those patients who showed a significant asimmetric trunk postural attitude to confirm the presence of a spine dysmorphism and to quantify Risser index and Cobb degrees. After this objective and functional evaluation, all those patients who were in line with our study inclusion criteria: a. were recruited for the aim of this study; b. received an informed consent which was signed by their parents; c. received the indication for the prescription and manufacturing of our innovative spine brace called BRIXIA; d. were included in our rehabilitative treatment program.
b. T1 (15 days from baseline T0)
To realize our BRIXIA spine brace, a trunk plaster cast was acquired in all patients recruited in the Prosthetic and Orthothic Lab - Poliortopedia S.r.l of Brescia (Italy).
Experimental course
a. T2 (15 days from time T1)
Patients returned in the Orthotic Lab and guided by the orthotic technician and the physiotherapist underwent a surface EMG assessment of the paraspinal muscle activity during a sitting position, an orthostatic position and during an anterior trunk bending. Two SEMG evaluations were made for each patient in each study position and 2 measurements were made in each condition: paraspinal muscle activity in a resting condition and during a so called pneumothorax thrust (after a slow but maximal inspiration patient made a similar expiration, obtaining at the end of this mechanical procedure his/her maximal trunk elongation). The SEMG bilateral activity of the large rhomboid, the latissimus dorsi and the quadratus lumborum was investigated without spine brace, by using a common Chenêau brace and wearing our dynamic BRIXIA spine brace. At the end of this SEMG evaluation, each patient received for a daily use (18 hours per day) the final version of the BRXIA spine brace and began an individualized postural rehabilitative treatment course.
b. T3 (90 days from time T2 and beginning of the rehabilitative treatment course)
A second SEMG assessment of the paraspinal muscle activity was made, guided by the same orthotic technician and the same physiotherapist. The examination was assessed without using a spine brace and by using BRIXIA. Each patient was evaluated in a resting condition and realizing a self-made cross-linked spine correction, acquired during the rehabilitative treatment course.
c. T4 (60 days from time T3)
A third and last SEMG assessment of paraspinal muscle activity was made in each patient in the same way made at time T3 and guided by the same physiotherapist and medical doctor. Finally, each patient underwent a functional, radiographic and postural evaluation to define and quantify an eventual amelioration and modification of spine orthostatic attitude at the end of a combined (rehabilitative and device supported) conservative postural treatment (Figure 1).
Outcome measures
Clinical-functional outcome measures
- Cobb degrees of the main scoliotic curve (radiographic acquisition)
- Spine rotation degrees (acquired with the Adams test, positioning the scoliometer below the main spine humpback)
- Visual postural analysis (VPA)
- Recruited patients underwent an objective orthostatic postural evaluation focusing the attention to:
a. Shoulder and hip alignment
b. Symmetric or asymmetric relation between trunk sides
c. Alignment of the head-neck-trunk unit
d. Alignment of the binocular vision
e. Plantar support alignment
f. Alignment of the psysiological spine curves
- Posterior body muscle chains elasticity
Measurement of the finger floor distance (FFD) in a self-controlled maximal flexed trunk position (anterior trunk bending).
Surface EMG (SEMG)
A third and last SEMG assessment of the paraspinal muscle activity was made in each patient in the same way made at time T3 and guided by the same physiotherapist and the medical doctor. Finally, each patient underwent a functional, radiographic and postural evaluation to define and quantify an eventual amelioration and modification of patients’ postural spine orthostatic attitude at the end of a combined (rehabilitative and device supported) conservative postural treatment.
The SEMG measurements of the posterior paraspinal muscle chain activity of each patient were acquired during:
1. SiRP (Sitting Resting Position)
2. SiRCP (Sitting Recruiting Position with a so called pneumothorax thrust: after a slow but maximal inspiration patient made a similar expiration, obtaining at the end of this mechanical procedure his/her maximal trunk elongation
3. StRP (Standing Resting Position)
4. StRCP (Standing Recruiting Position)
5. BA (Anterior Trunk Bending)
6. BARC (Anterior Trunk Recruiting Bending)
In line with the SENIAM instructions, the SEMG electrodes were placed bilaterally onto the paraspinal muscles, namely, large rhomboid, latissimus dorsi and quadratus lumborum. The SEMG raw data were averaged by using the root mean square (RMS) to obtain the average amplitude of the the EMG signal of each target muscle activity. The RMS SEMG ratio of each patient was calculated using the following equation (Kwok et al., 4):
RMSsEMG Ratio is an index of the symmetric SEMG activity of the target muscles, in which when the ratio is 1, the pairs target muscles showe an identical SEMG activity from the concave and convex side of the spine; if the ratio is less than 1, the concave side of the paraspinal muscle has stronger SEMG activity than the convex side; if the ratio is larger than 1, the concave side of the paraspinal muscle has weaker SEMG activity than the convex side. For the aim of this study, this equation was used to assess the effectiveness of the suggested positions for the scoliosis patient: the study positions are effective if the ratio is closer to 1 compared to the ratio acquired for the normal postures.
Clinical and observational evaluation procedure
Recruited patients were evaluated acquiring clinical and observational measurements:
- at time T2 and T4, Cobb degrees of the main scoliotic curve (radiographic acquisition), spine rotation degrees (acquired with the Adams test, positioning the scoliometer below the main spine humpback), the visual postural analysis (VPA)
- at time T2 and T4, the finger floor distance (FFD) in a self-controlled maximal flexed trunk position (anterior trunk bending)
SEMG evaluation procedure
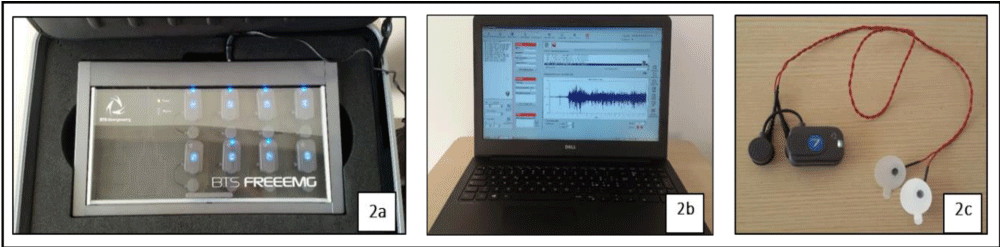
Each patient underwent at baseline and at each follow-up evaluation of our study design to a SEMG evaluation. We used for the SEMG acquisition a polygraphic EMG system (FREEEMG by BTS Bioengeneering - USA) (Figure 2a). The device uses a data acquisition system (Figure 2b), around 20 skin probes coupled with SEMG electrodes in wireless way or by using singular cables (Figure 2c)
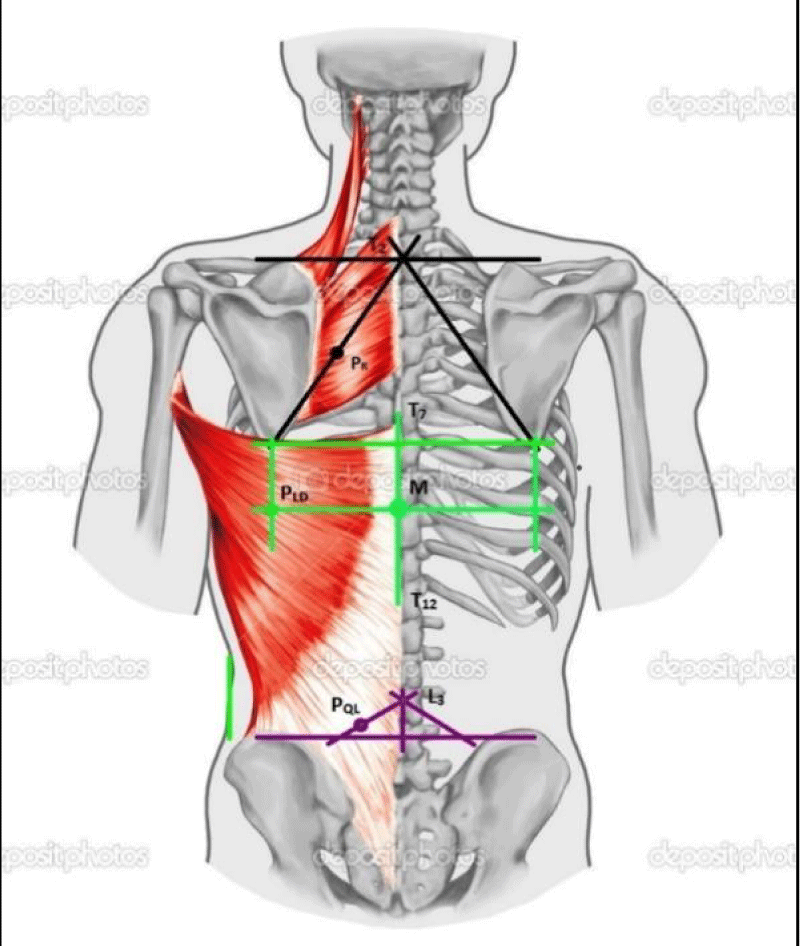
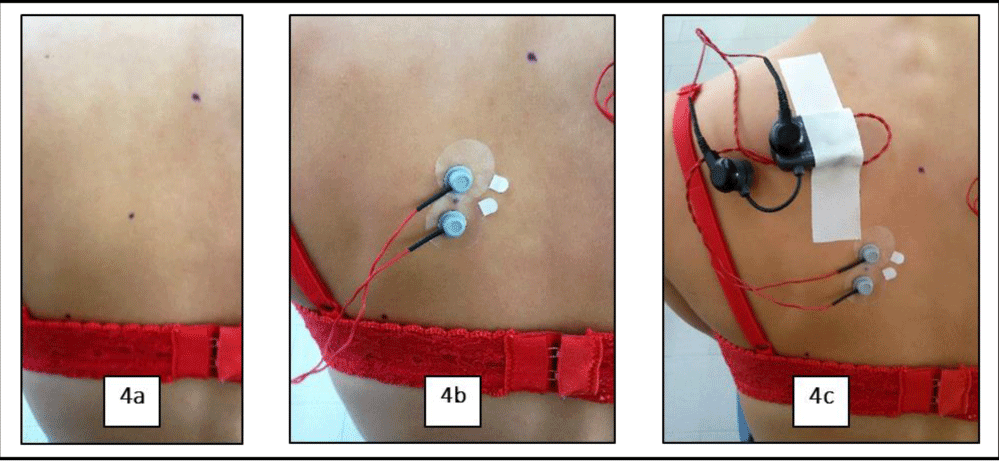
For an optimal EMG acquisition, the back skin was scratched lightly before positioning our type of electrodes. In line with guidelines, codified by Stegemans and Hermens [12], the electrodes were placed by the physiotherapist onto the paraspinal target muscles, namely, large rhomboid, latissimus dorsi and quadratus lumborum (Figure 3).
Figure 3: Identification of the paraspinal muscle regions for the electrodes positioning (own elaboration).
Two electrodes were placed on each target muscle, previously identified, from edge to edge of the electrode collars in the direction of the muscle fibers (Figures 4a-4c).
Figure 4: Placement procedure of the SEMG electrodes on target paraspinal muscle regions (own elaboration).
The sampling rate was established at 1000Hz; the raw EMG signal was digitally rectified, filtered (band-pass, 20-450Hz). The duration of EMG acquisition was established at least 20 seconds at the beginning of each motor task of our study design.
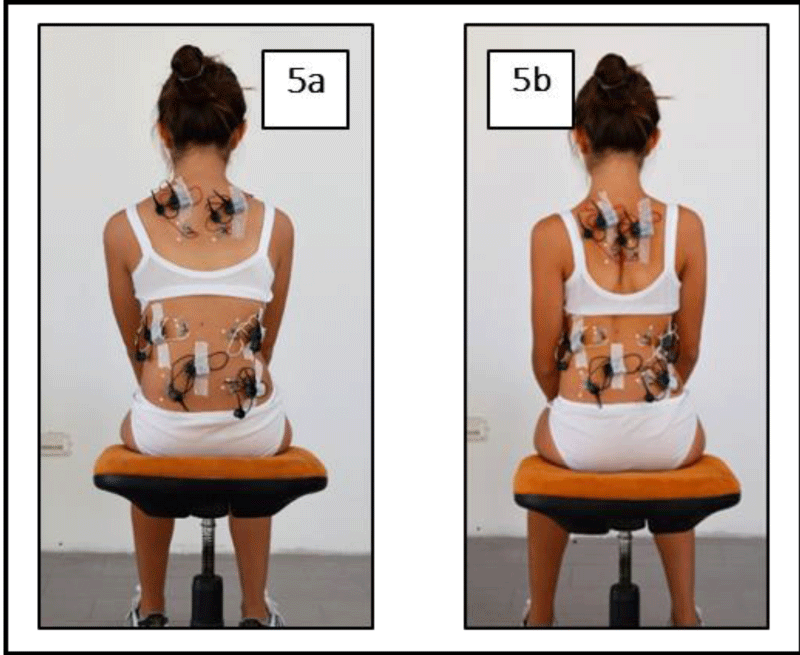
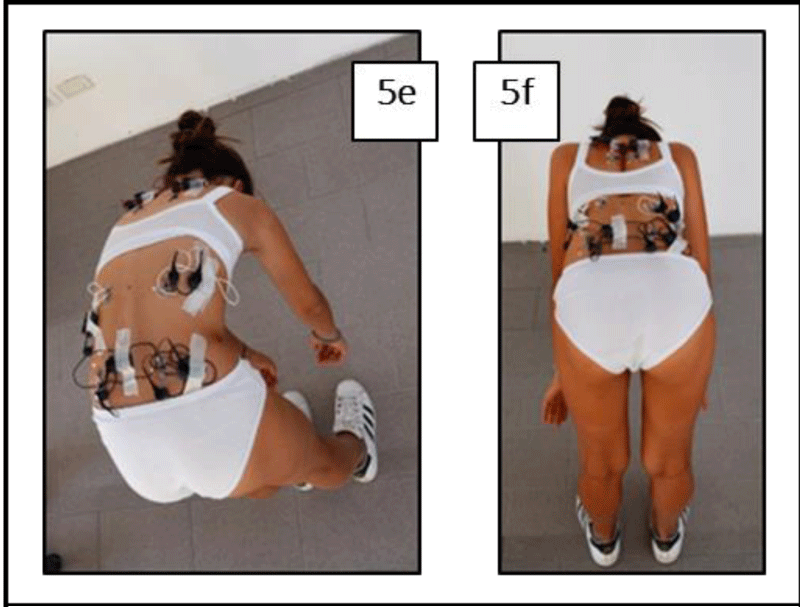
In line with this preliminary procedure, at time T2, T3 and T4 we proceeded with our SEMG assessment in six postural study conditions: a. SiRP = Sitting Resting Position (Figure 5a); SiRCP = Sitting Recruiting Position with a so called pneumothorax thrust (Figure 5b); StRP = Standing Resting Position (Figure 5c); StRCP = Standing Recruiting Position (Figure 5d); BA = Anterior Trunk Bending (Figure 5e); BARC = Anterior Trunk Recruiting Bending (Figure 5f).
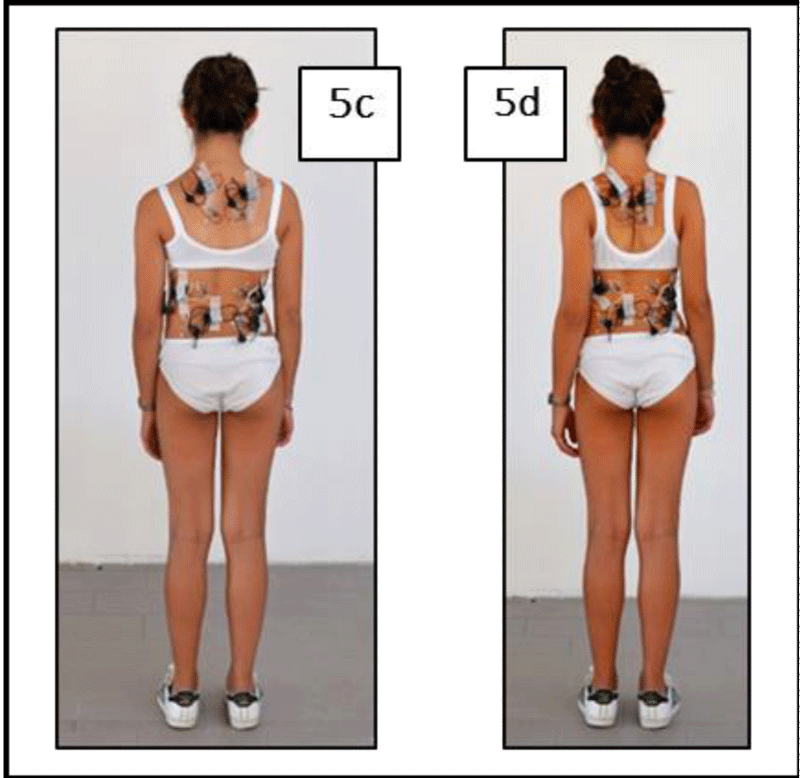
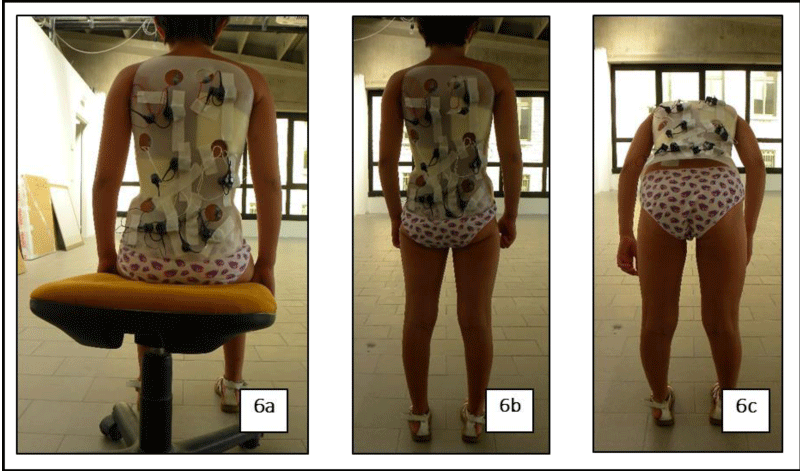
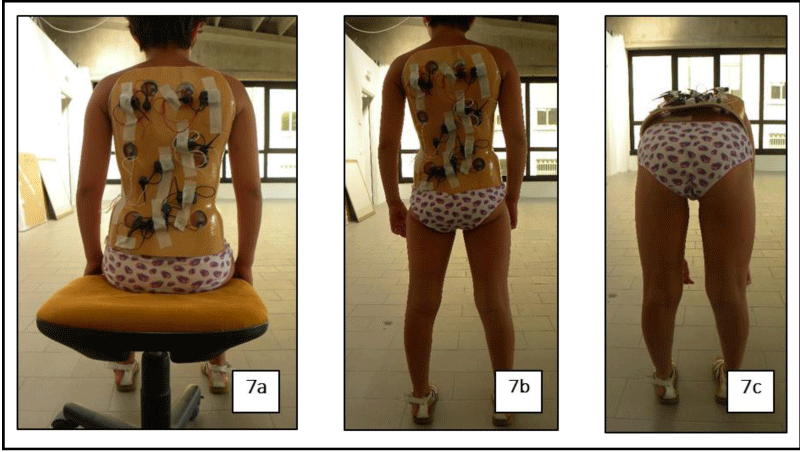
At time T2, each patient underwent a SEMG analysis without a spine brace, wearing a traditional Chêneau spine brace (a well-known static and symmetric spine brace) (Figures 6a-6c), and finally wearing our asymmetric and dynamic spine brace called “BRIXIA” (Figures 7a-7c). At time T3 and T4 the same SEMG analysis was made with and without BRIXIA brace.
BRIXIA spinal brace: BRIXIA spinal brace can be considered as a conceptual evolution of the traditional Chêneau brace with some significant differences as: singular manufacturing process, structural plasticity and high proprioceptive and rehabilitative value in the treatment of AIS. If we consider all spinal braces used in the last thirty years, Brixia brace allows to increase patient’s:
• postural sense
• core stability with a secondary increase of feedback and feed forward balance control strategies
• cross-linked paraxial muscle recruitment with a strong lateral and rotational trunk corrective imprinting
• pneumothorax thrust during the trunk elongation self-correction
• dynamic 3-D trunk postural attitude self-correction inside the brace and during the rehabilitative postural treatment
Without paraxial push shells and escapes areas, BRIXIA allows to imprint mechanically and from a proprioceptive point of view a default trunk postural correction that the orthotic technician still realizes during the trunk plaster manufacturing. By using this kind of spine brace, patients does not feel empty areas between the skin and the device with a secondary increase of its proprioceptive value and inducing an immediate cross-linked trunk allignment self-correction. We consider BRIXIA spine brace as a “second skin” that trough its structural plasticity and high proprioceptive and rehabilitative value can dynamically help patients to learn postural and trunk alignment self-corrrection strategies. The time-related use and an eventual remanufacturing of this kind of spine brace follows a singular functional paradigm: “until my postural attitude will change also my second skin or my BRIXIA need to change”.
BRIXIA manufacturing procedure
The Brixia manufacturing process follows 8 steps:
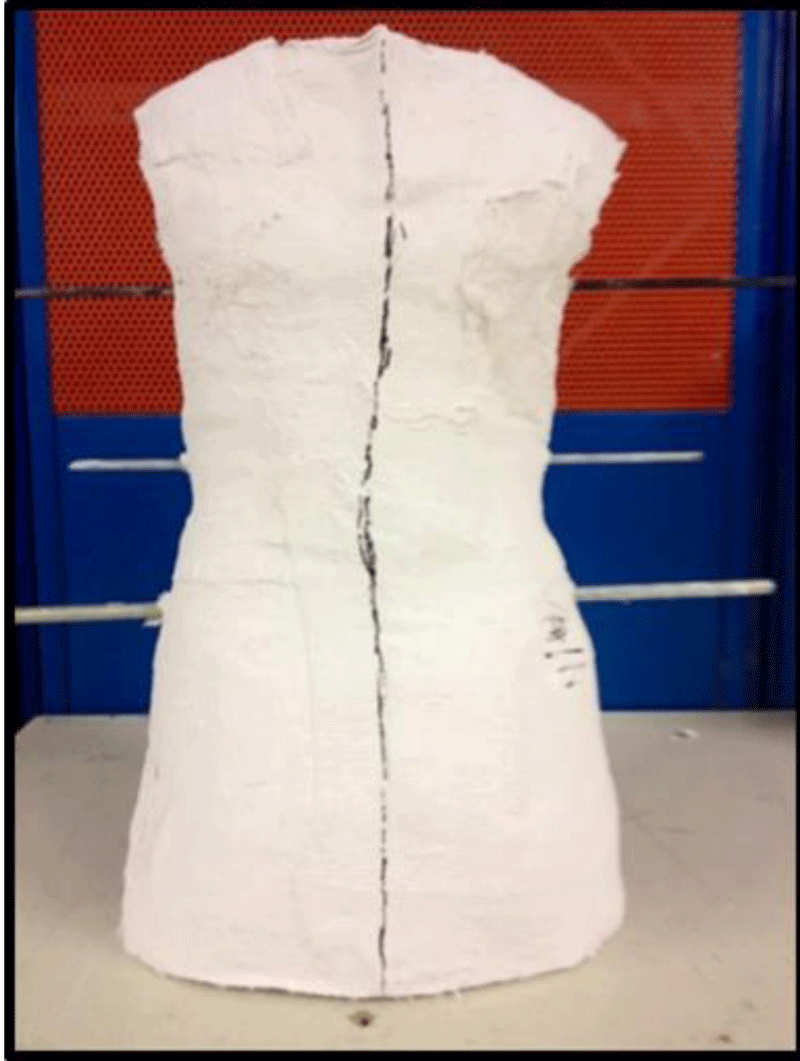
• step 1 – trunk plaster acquisition by using plaster bandages and realizing an accurate trunk cast (Figure 8);
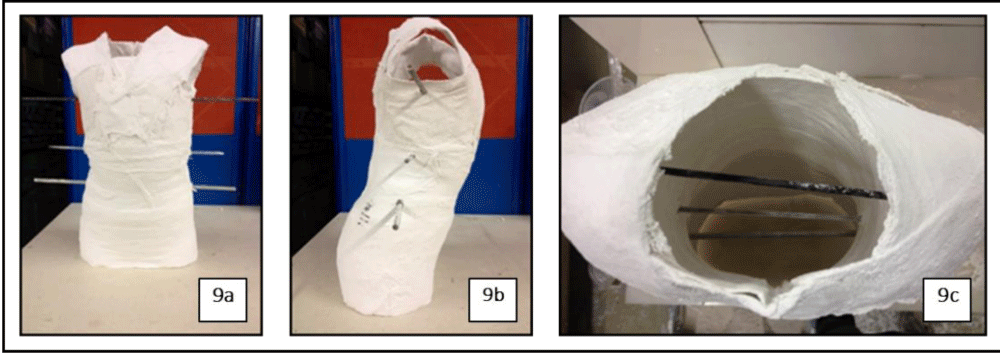
• step 2 – introduction of three horizontal metal bars in the plaster cast (1 through the axilla level, 1 through the dorsolumbar level and 1 through the iliac crest) to identify the rotational component of the scoliotic dysmorphism (Figures 9a-9c);
Figure 9a-c: Identification strategy to identify the rotational component of the scoliotic dysmorphysm on the trunk plaster (own elaboration).
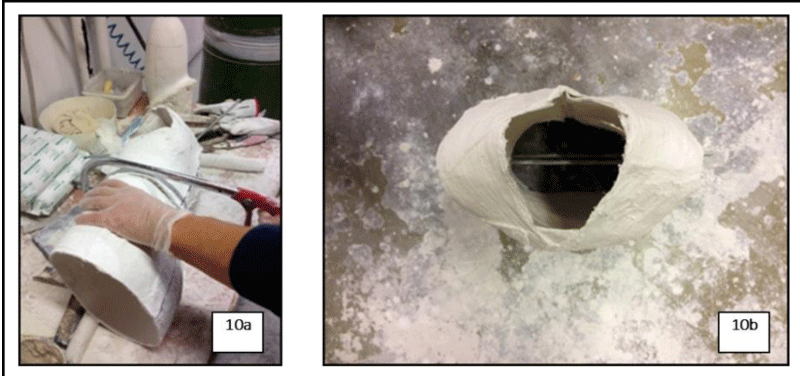
• step 3 – plaster cast cutting in three parts, with a secondary frontal realignment of each part to realize a secondary perfect frontal realignment of the metal bars and to define a correct trunk rotational attitude facilitation (Figures 10a,10b);
Figure 10a,b: Plaster cast cutting in three parts, with a secondary correct frontal realignment of each part of them (own elaboration).
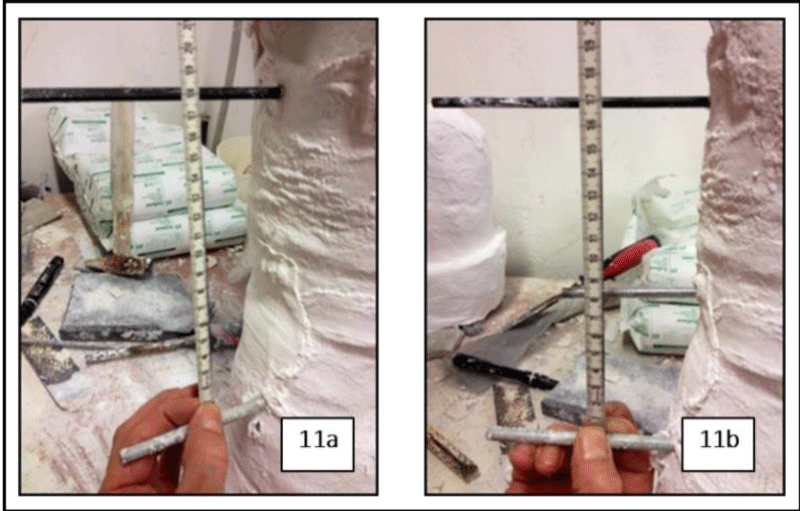
• step 4 – sagittal realignment and bilateral elongation of the plaster cast to realize a symmetric scapular and pelvic alignment facilitation (Figures 11a,11b);
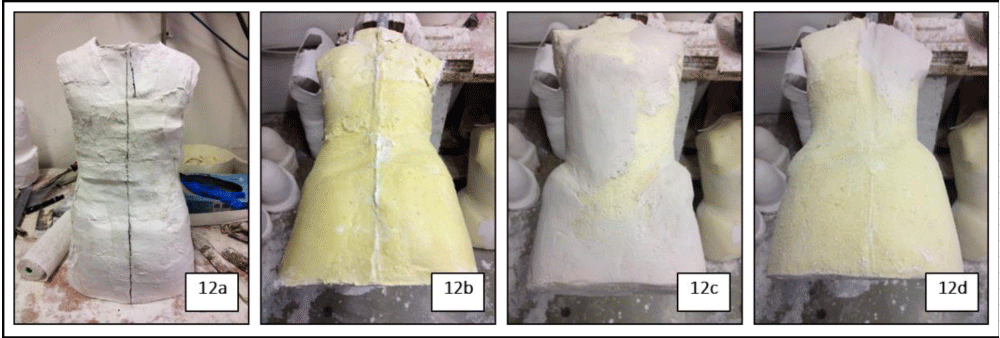
• step 5 – using the empty shaped plaster cast, a polyurethane (Pedilen) device will be realized; secondary the orthotic technician handly models the surface of this device to realize a uniform assessment of the anterior and posterior part of our spinal brace (Figures 12a-12d);
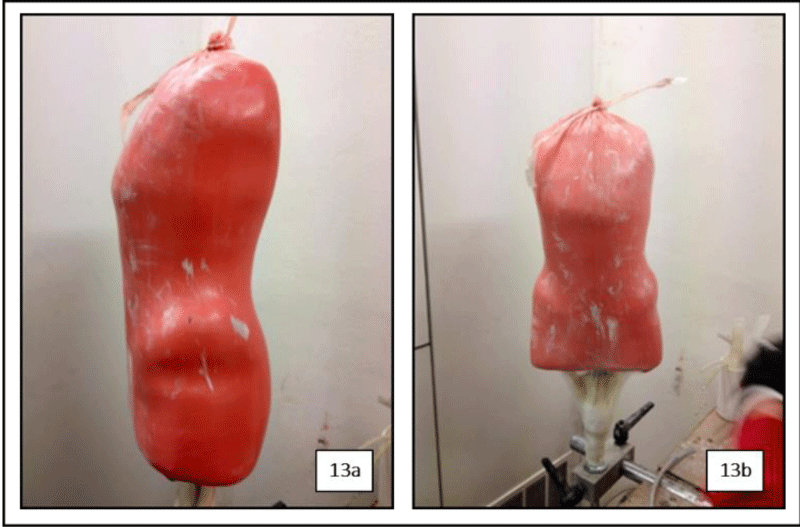
• Step 6 – the sponge mould realized will be perfectly covered with a heat-resistent plastic bag by using a vacuum pump and tied up in the upper extremity with a string; a second heat-resistent plastic bag will be used to cover the first one by preserving a little space between the two bags; at the end, an epoxy resine flow will be insert in the little space created between the two bags which were finally tied up in the upper extremity with a string (Figures 13a,13b);
Figure 13a,b: Example of an epoxy resin heat-resistent plastic bag manufacturing by using a vacuum pump (own elaboration).
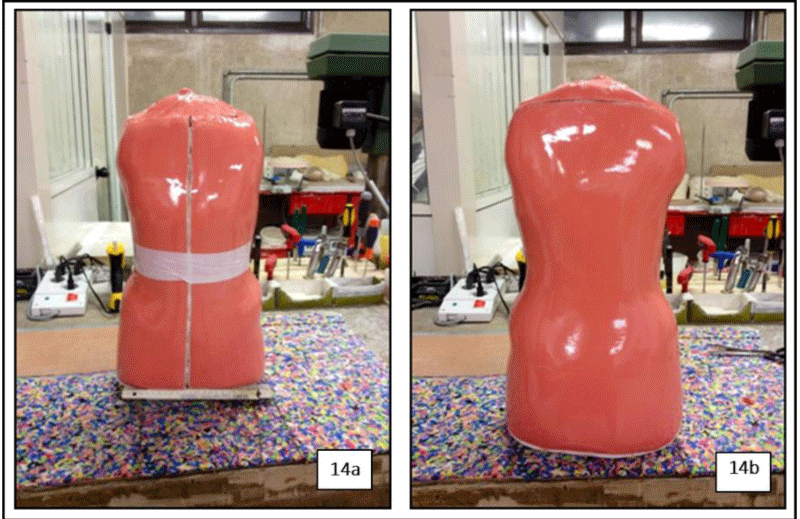
• step 7 – after 12 hours, the epoxy resine brace will be removed from the sponge mould with an anterior vertical midline engraving to allow the correct positioning of the upper limbs, the breast, the scapula and the clavicula bilaterally (Figures 14a,14b);
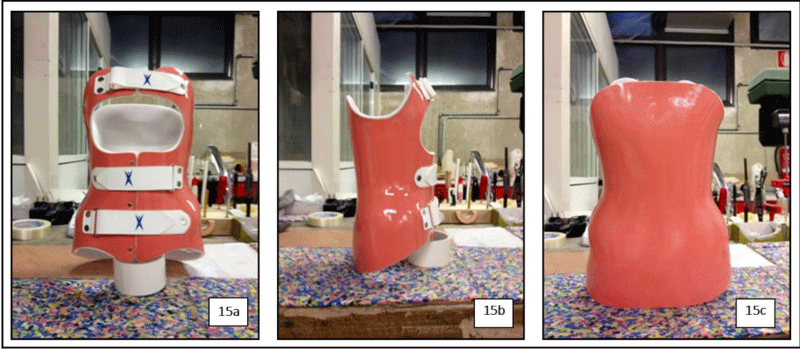
• step 8 – the brace will be covered inside with plastazote to obtaine the maximum wearing comfort, and finished with the anterior application of three plastic belts to allow the closing of the BRIXIA spine brace (Figures 15a-15c).
Figure 15a-c: Definitive version of BRIXIA brace in front, lateral and posterior view (own elaboration).
Rehabilitative approach
In line with the SOSORT indications, patients involved in our study and wearing BRIXIA brace were subjected to an integrated rehabilitation treatment path starting from time T2 (30 days from outpatient access).
Each recruited patient underwent at time T2 to a weekly rehabilitative treatment session, 1 hour duration per session, by using in the last 15 minutes of each rehabilitative session BRIXIA brace. During each rehabilitative session, patients were trained to a growing range of pro-proprioceptive exercises, facilitations to cross-linked and three-dimensional self-correction of the scoliotic spine and rebalance between anterior and posterior kinetic chains. Patients were also performed to repeat all exercises, acquired at home for 15-20 minutes/day with the supervision of their parents. To optimize and individualize our rehabilitative model, specific outcome goals were setup:
- development of patient’s individual sense of posturality (cognitive-behavioural training related to body position and correct muscles recruitment);
- acquisition of cross-linked self-correction strategies of the asymmetric axial orthostatic assessment on the frontal plane, fixation in elongation of the spine dorso-lumbar passage, focusing the attention on patient’s prevention and triggering of postural upstream and downstream compensations, training of pneumothoracic elongation thrust as a simple axial self-correction strategy, of the rib cage, derotation (often manually guided) of the right and/or left-handed spinous processes rotations and dorsal deciphotization and/or lumbar delordosization (also often manually guided);
- progressive rebalancing between the anterior and posterior kinetic muscle chains recruitment;
- daily correct management of BRIXIA brace and development of self-correction strategies acquired by using it;
- constant monitoring of the pro-corrective suitability of the corset with identification of any red-flags, that will be immediately communicated to the referring Physician for a possible structural adaptation of the brace (if possible and adviced) or a re-construction of it;
- constant monitoring of patient’s compliance and adherence to the execution of proposed and learned exercises.
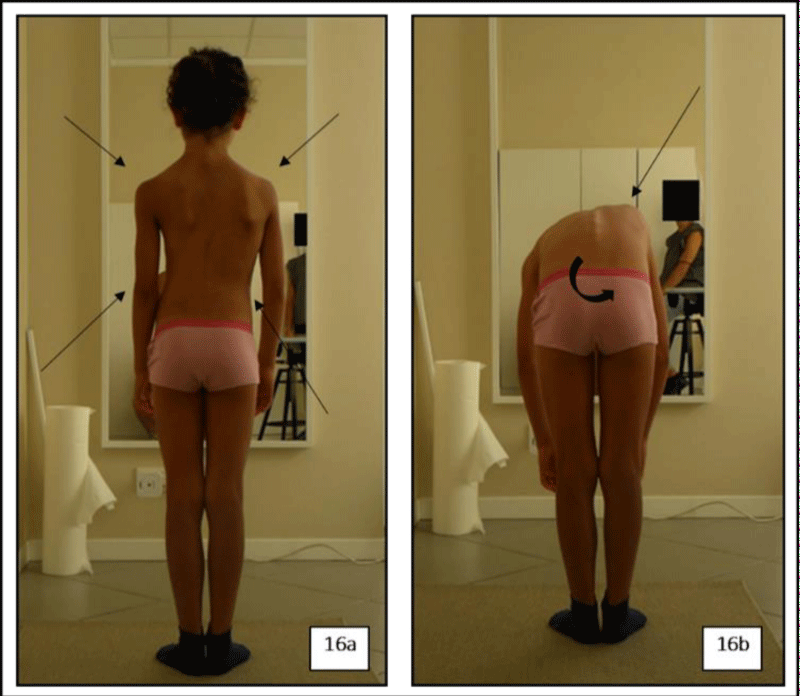
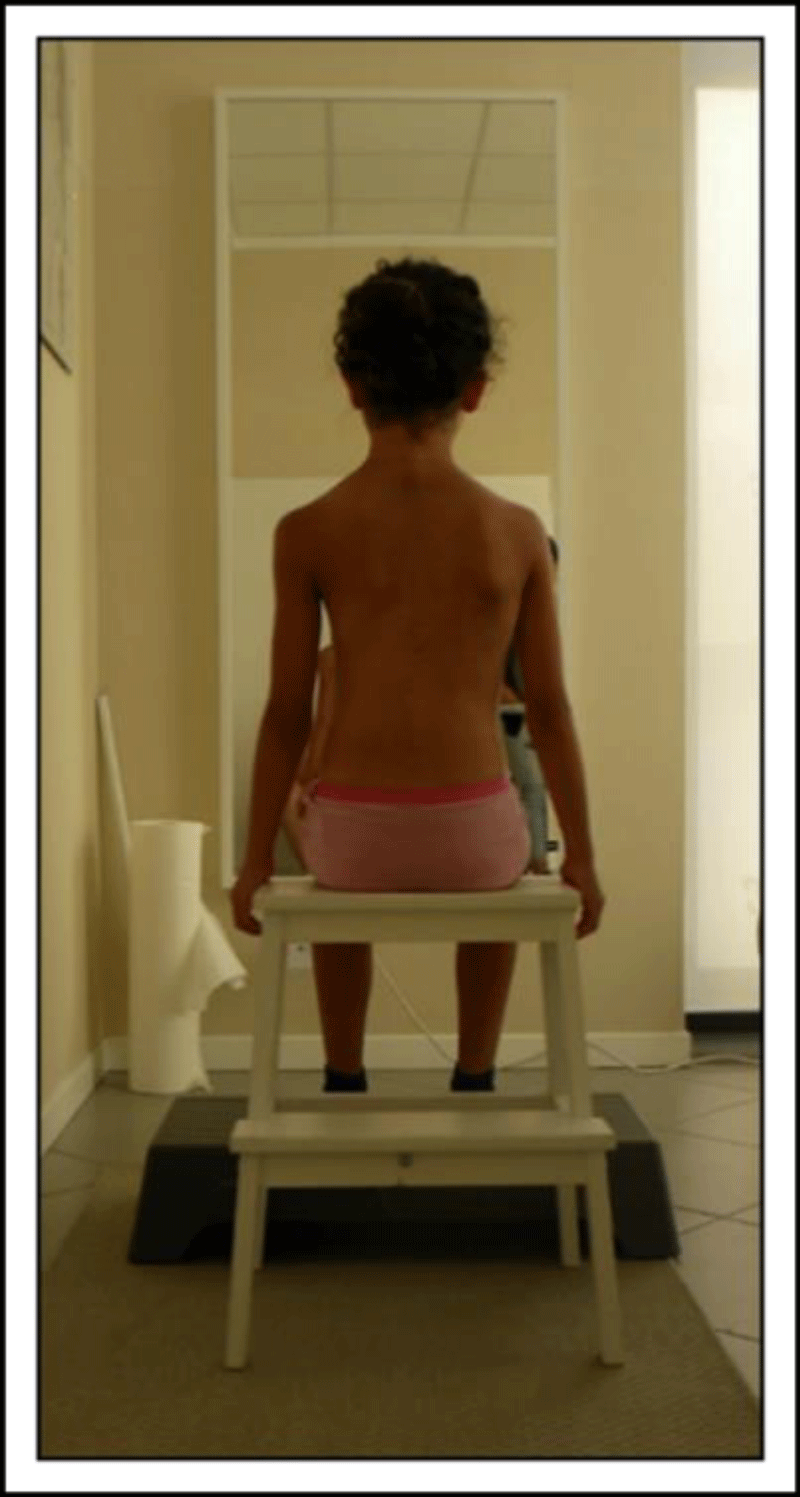
The rehabilitative session, proposed to one of our young patients, consisted in a physiotherapeutic evaluation of the initial postural attitude, in orthostatism and in anterior bending, focusing attention on all the objective and anthropometric aspects of the current axial dysmorphism (Figures 16a,16b); subsequently, the patient was observed in a sitting position with a personalized adjustment of the height of the seat and of the supporting feet in order to realize a postural sitting position with a 90° flexion angle of the pelvis on the lower limbs (Figure 17).
Figure 16a,b: Objective evaluation of axial dysmorphism in A/P view and front bending (own elaboration).
Figure 17: Setup of a correct ergonomic sitting position, adapted to patient’s height (own elaboration).
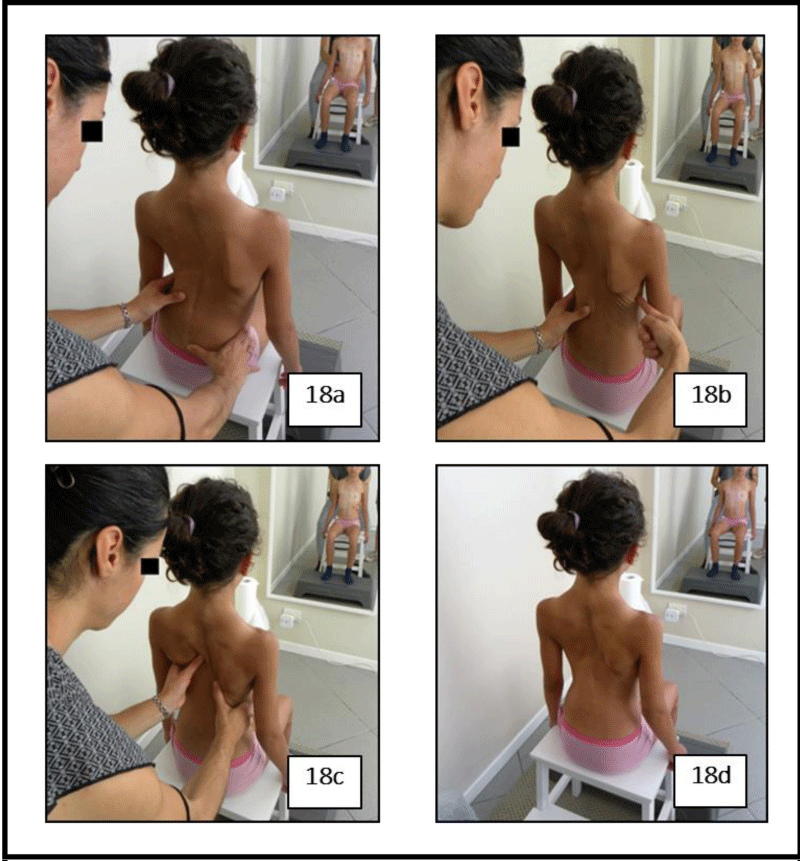
Starting from this positional assessment, the therapist proceeds manually to a guided correction of the axial alignment. Impressing digital and manual corrective pressions first in latero-lateral direction on the lumbar segment, then in the dorsal one and on the ribs, the physiotherapist tries to reduce the rotation of spinous processes (manually guided axial derotation) with the purpose to recover a correct alignment in adduction of scapulo-humeral girdles (Figures 18a-18d). Reached the expected axial alignment, patient is asked to maintain the correct position for 30 seconds in isometric paraxial muscle contraction with subsequent relaxation of the recruited muscle chains. This exercise is repeated 5 times per session to reach a so-called motor and perceptive engrammation of the postural self correction strategy acquired; as a supervisor, the therapist guides vocally and manually the patient to the optimal postural correction during each session, modifing eventual objective imperfections; for a visual feedback facilitation, a mirror can be placed in front of the patient during this rehabilitative phase.
Figure 18a-d: Manual facilitation for axial self-correction and final maintenance of the desired posture achieved (own elaboration).
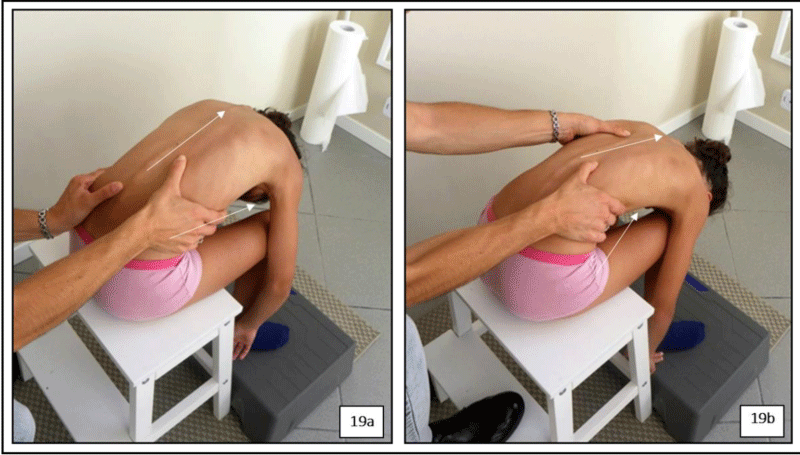
The same corrections are required and manually facilitated by asking the patient to perform a progressive and slow forward flexion of the trunk (still in a sitting position), as shown in figures 19a,19b.
Figure 19a,b: Manual facilitation maneuvers for axial self-correction and final maintenance of the desired posture achieved in anterior bending of the trunk (own elaboration).
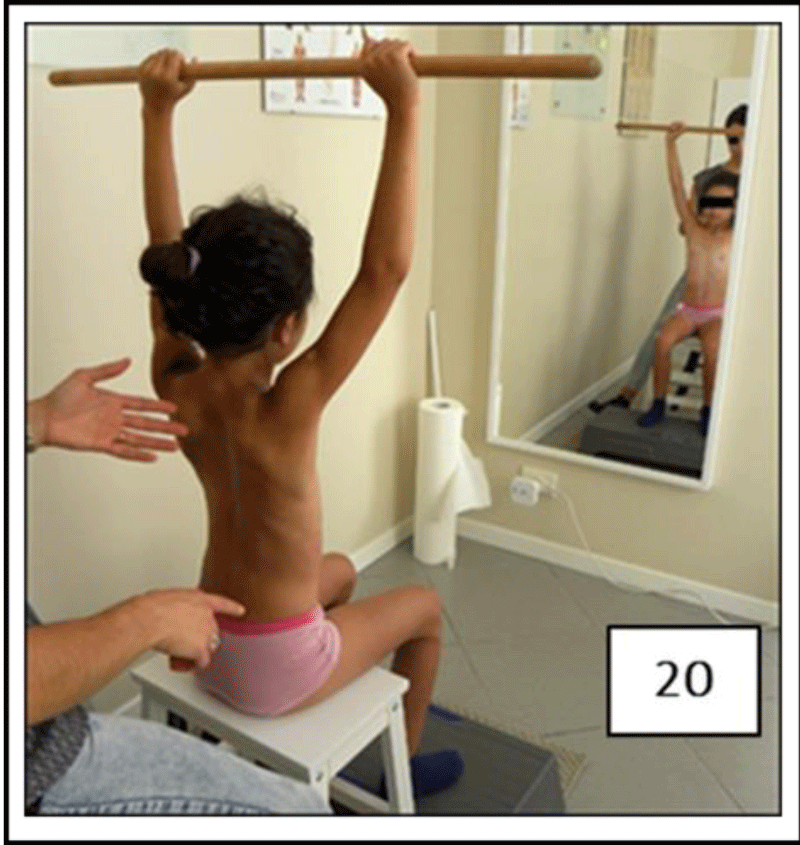
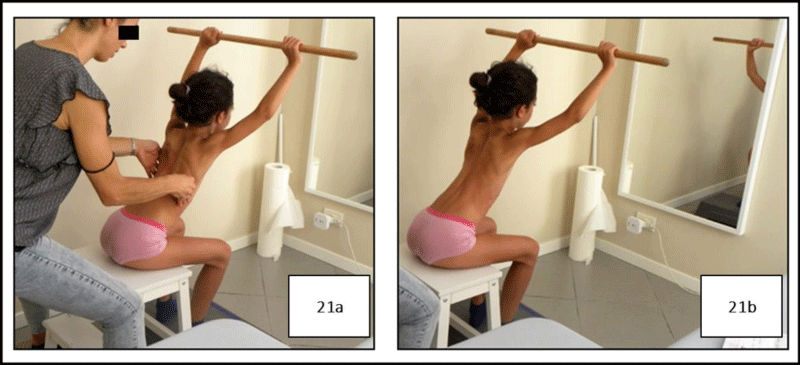
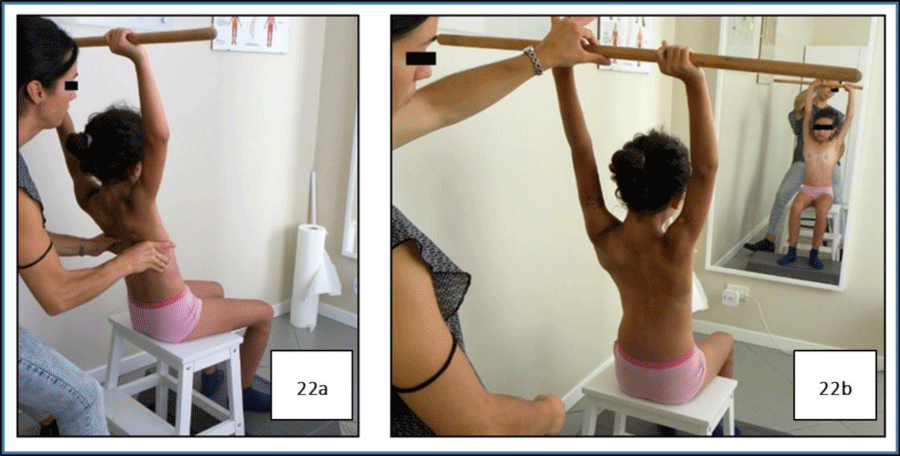
Fixing the initial sitting position, the therapist uses a stick that the patient keeps with both hands above the head with limbs extended (Figure 20), producing a sort of distal constraint to set and guide, with elongated spine, manual axial corrections in sitting position and anterior bending. Reached the maximal range of self-correction in spine elongation, the patient is asked to maintain the position with an isometric paraxial muscle contraction for 30 seconds; the exercise is repeated for 5 times, asking the patient to return to starting position at the end of each repetition (Figures 21a,21b). The same exercise is than repeated, by asking the patient a posterior trunk bending (Figures 22a,22b).
Figure 20: Positioning of the patient in axial elongation in S/S with the stick kept in two-hand grip above the head (own elaboration).
Figure 21a,b: Exercise of guided correction of axial alignment with stick constraint in anterior bending (own elaboration).
Figure 22a,b: Exercise of guided correction of axial alignment with stick constraint in posterior bending (own elaboration).
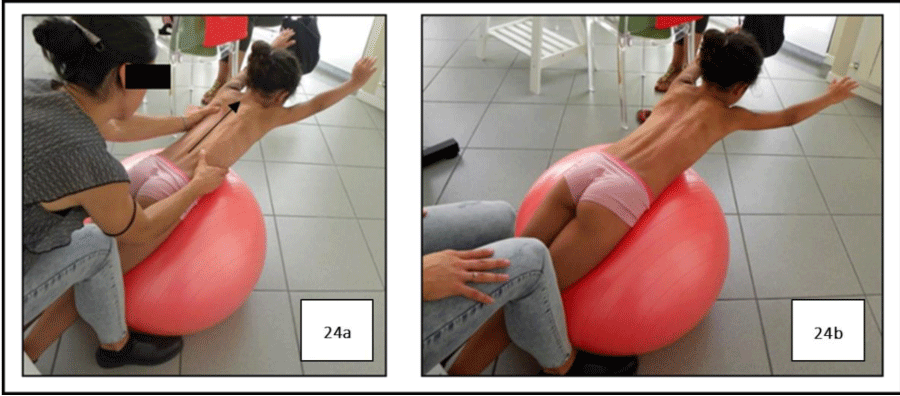
Once the patient has achieved a satisfactory ability to repeat the axial self-corrective strategies, it will be possible to introduce exercises in prone decubitus, resting on the abdominal wall on a Bobath ball, leaving legs elongated with feet resting on the ground on their tips and hands resting with the palm on the floor (Figure 23). Starting from this position, the patient is asked to perform a trunk extension with a synchronous elevation of both arms extended while therapist provides specific manual corrections on both dorsal and lumbar spine; after reaching the maximum range of correction, the patient is asked to maintain this attitude with an isometric trunk muscles contraction for 30 seconds, repeating the exercise for 5 times (Figures 24a,24b).
Figure 23: Starting position in a facilitated exercise with Bobath ball in prone decubitus (own elaboration).
Figure 24a,b: Exercise of trunk extension with Bobath ball in, first guided by the therapist and then self-corrected (own elaboration).
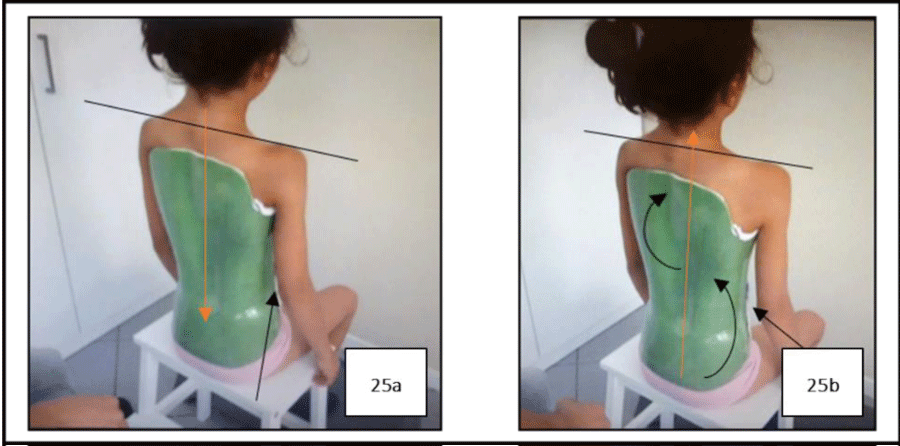
Deeply exploiting pro-proprioceptive and pro-rehabilitative properties on the “skin”, offered by the BRIXIA brace, the therapist will perform during the last 10-15 minutes of the physioterapic rehabilitation session the facilitating path to axial self-correction, previously set, by using the brace (Figures 25a,25b). The effectiveness of patient’s self-correcting postural strategies by using BRIXIA brace is evaluated by the therapist through light digital strokes performed on its dorsolumbar surface. If the stroke sound, produced during the self-correction in correspondence of the scoliotic curve, is “severe”, the patient is able to react to the dynamic pro-corrective facilitation induced by the spine brace at that point, moving away from the inner surface of it; otherwise, the sound will be “acute” if the patient can’t detach himself in self-correction from the inner surface of the brace at that point, on which instead he will tend to lie down (Figure 26).
Data processing and statistics
Statistical analysis was made using the statistical software SPSS (version 22). Time-related differences between our clinical variables and RMS data, acquired using SEMG analysis of paraxial dorsolumbar muscles activity, was performed in all six study conditions using a parametric one-sample t-test. The non-parametric Wilcoxon post-hoc test was also used to realize an inter-time (from time T0 to time T4) comparative analysis between our RMS and clinical data. The significance level was set to p< 0.05.
Results
VPA (Visual Postural Analysis)
At time T0 and time T4, recruited patients underwent an objective orthostatic postural evaluation (Visual Postural analysis or VPA) focusing the attention to:
- symmetric or asymmetric relation between the trunk sides and the shoulder and hip alignment
- frontal head-neck-trunk unit alignment
- plantar support alignment
- analytical and global postural attitude
The VPA profile modification, proceeding from time T0 to time T4 (at this last time evaluation made with and without BRIXIA brace) was made for each patient (P) focusing attention on each postural variable mentioned above in tables 3-7.
| Table 3: VPA of P1 – M.N. (own elaboration). | |||||
| Patient P1-M.N. | Visual Postural Analysis (VPA) | ||||
| Evaluation time | Trunk sides | Hip alignment | Head-neck-trunk unit | Plantar support alignment | Postural attitude |
| T0 | Asymmetric with a right shoulder elevation | Asymmetric with left hip elevation | Right side flexed | Minimal hind and mid foot valgus-pronation | Dorsal trunk astenic attitude with a lumbar pseudo-hyper lordosis |
| T4 with BRIXIA | Amelioration of the symmetry with a decreased right shoulder elevation | Decreased asymmetry with a residual left hip elevation | Greater realignment | Greater realignment of the hind/midfoot | Decrease of the dorsal hyperkiphosis and of the lumbar lordosis |
| T4 without BRIXIA | Preservation of the symmetry | Decrease of the asymmetry | Further greater realignment | Normalization of the medial plantar muscle tonous and of the ankle stability | Greater control of the physiological dorsal kyphosis and the lumbar lordosis |
| Table 4: VPA of P2 – L.F. (own elaboration). | |||||
| Patient P2-L.F. | Visual Postural Analysis (VPA) | ||||
| Evaluation time | Trunk sides | Hip alignment | Head-neck-trunk unit | Plantar support alignment | Postural attitude |
| T0 | Asymmetric with a right shoulder elevation | Asymmetric with left hip elevation | Right side flexed | Medial plantar surface hypotonous with a physiological hindfoot valgus | Dorsal trunk astenic attitude with a lumbar pseudo- hyperlordosis |
| T4 with BRIXIA | Amelioration of the symmetry with a decreased right shoulder elevation | symmetric | Aligned | Residual flat-foot | Decrease of the dorsal hyperkiphosis and of the lumbar lordosis |
| T4 without BRIXIA | Preservation of the symmetry | Symmetric | Preservation of the alignment | Residual flat-foot | Greater control of the physiological dorsal kyphosis and the lumbar lordosis |
| Table 5: VPA of P3 – P.E. (own elaboration). | |||||
| Patient P3- P.E. | Visual Postural Analysis (VPA) | ||||
| Evaluation time | Trunk sides | Hip alignment | Head- neck- trunk unit | Plantar support alignment | Postural attitude |
| T0 | Asymmetric with a left shoulder elevation | Asymmetric with left hip elevation | Right side flexed | Normal | Dorsal trunk astenic attitude with a lumbar pseudo-hyperlordosis and an innatural anterior head flexion |
| T4 with BRIXIA | Amelioration of the symmetry with a decreased left shoulder elevation | Decreased asymmetry with a residual left hip elevation | Unchanged | Normal | Decrease of the lumbar lordosis and of the anterior head flexion |
| T4 without BRIXIA | Further amelioration of the symmetry wit a less left shoulder elevation | Further decreased asymmetry with a residual left hip elevation | Unchanged | Normal | Decrease of the lumbar lordosis and of the anterior head flexion |
| Table 6: VPA of P4 – F.M. (own elaboration). | |||||
| Patient P4-F.M. | Visual Postural Analysis(VPA) | ||||
| Evaluation time | Trunk sides | Hip alignment | Head-neck-trunk unit | Plantar support alignment | Postural attitude |
| T0 | Asymmetric with a right shoulder elevation | Asymmetric with right hip elevation | Aligned | Normal | Dorsal trunk astenic attitude with a lumbar pseudo-hyperlordosis |
| T4 with BRIXIA | Amelioration of the symmetry with a decreased right shoulder eleation | Decreased asymmetry with a residual right hip elevation | Aligned | Normal | Decrease of the dorsal hyperkiphosis and of the lumbar lordosis |
| T4 without BRIXIA | Light amelioration of the symmetry with a less right shoulder elevation | Decrease of the asymmetry | Aligned | Normal | Greater control of the physiological dorsal kyphosis and the lumbar lordosis |
| Table 7: VPA of P5 – S.S. (own elaboration). | |||||
| Patient P5 –S.S. | Visual Postural Analysis (VPA) | ||||
| Evaluation time | Trunk sides | Hip alignment | Head-neck-trunk unit | Plantar support alignment | Postural attitude |
| T0 | Asymmetric with a right shoulder elevation | Asymmetric with left hip elevation | Left side flexed | Minimal hind and midfoot valgus-pronation | Dorsal trunk astenic attitude with a lumbar pseudo-hyperlordosis |
| T4 with BRIXIA | Amelioration of the symmetry with a decreased right shoulder elevation | Decreased asymmetry with a residual left hip elevation | Further alignment | Further alignment of the mid/hindfoot | Decreased of the dorsal hyperkiphosis and of the lumbar lordosis |
| T4 without BRIXIA | Preservation of the symmetry | Symmetric | Preservation of the alignment | Normalization of the medial plantar muscle tonous and of the ankle stability | Greater control of the physiological dorsal kyphosis and the lumbar lordosis |
We observed an amelioration of the symmetry of trunk sides, shoulders and of the hip alignment at time T4 by using BRIXIA brace; this VPA profile was preserved and in some cases demonstrated a further amelioration without BRIXIA use, with a clear evidence of the effectiveness of the cross-linked self-correction strategies acquired during the rehabilitative treatment and facilitated by BRIXIA use. Proceeding from time T0 to time T4, an increase of the symmetric hip alignment was also observed as a result of a progressive rebalancing, in a self-corrected postural arrangement, between the anterior and posterior kinetic muscle chains recruitment. In line with a muscle chain rebalancing concept of the global postural attitude, an increase of the medial plantar muscle tonous and of the ankle stability was observed at time T4 with and without BRIXIA brace use. At time T4, we also observed the achievement of an ergonomic remodulation of the global postural assessment in all patients recruited. At the end of the rehabilitative treatment, all patients showed a stronger sense of self-immage and self-correcting attitude reported by using BRIXIA brace (pro-proprioceptive and pro-rehabilitative properties offered by the BRIXIA brace) and a tonic postural control without using BRIXIA brace (motor and perceptive engrammation of the postural self correction strategies as expression of a perfect relationship between postural re-education and pro-rehabilitative effect offered by the BRIXIA brace use).
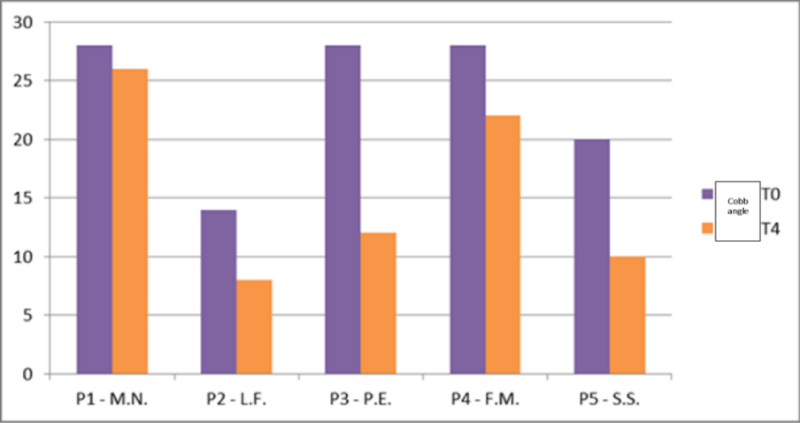
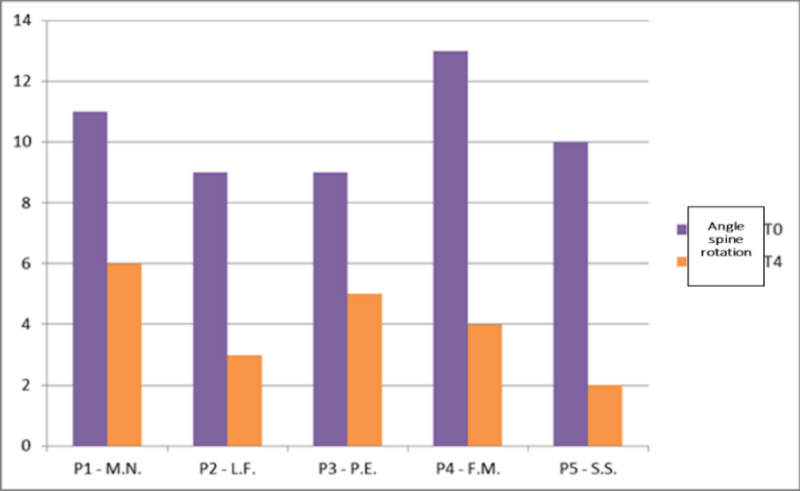
Cobb angle and α spine rotation
In line with our study design, we acquired for each patient the graw data of Cobb angle and of the related angle spine rotation proceeding from time T0 to time T4 (Table 8).
| Table 8: Resume of the time-relate trend course of Cobb angle and angle spine rotation proceeding from time T0 to time T4 (own elaboration). | ||||
| Patient | Cobb angle T0 | Cobb angle T4 | Angle spine rotation T0 | Angle spine rotation T4 |
| M.N. | 28° | 26° | 11° | 6° |
| L.F. | 14° | 8° | 9° | 3° |
| P.E. | 28° | 12° | 9° | 5° |
| F.M. | 24° | 22° | 13° | 4° |
| S.S. | 20° | 10° | 10° | 2° |
The analysis of the trend course of Cobb angle showed a not uniform decrease of this parameter proceeding from time T0 to time T4, with a consistent change in patient P.E and S.S (Figure 27).
Similarly, the anlaysis of the trend course of angle spine rotation, refered to the principal scoliotic curve, showed a conistent decrease of this parameter in all patients recruited from time T0 to time T4 (Figure 28).
Figure 28: Trend course of angle spine rotation proceeding from time T0 to time T4 (own elaboration).
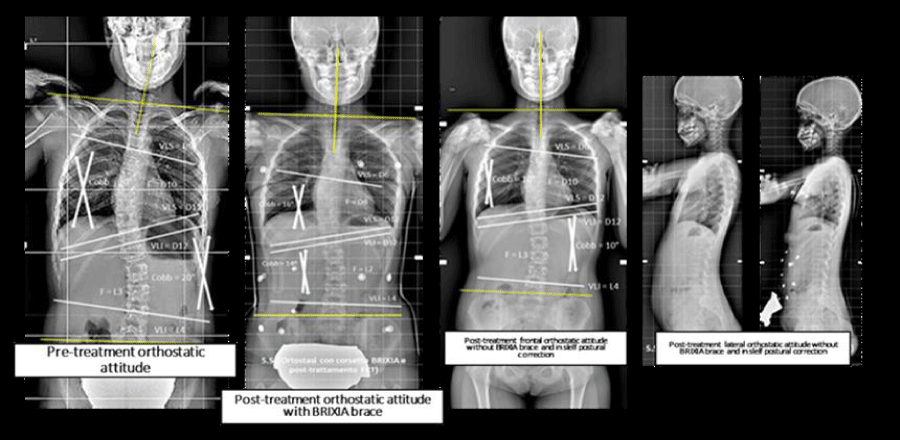
In line with the X-ray time-related evaluation of each patient postural attitude and modification of the Cobb angle, we observed an amelioration of the spine alignment proceeding from time T0 to time T4 with a not uniform trend for all patients recruited. Particularly:
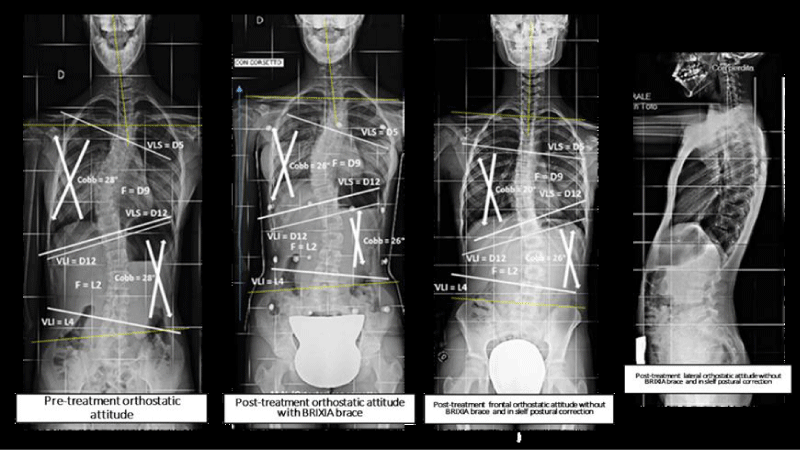
• at time T4 (Figure 29) we observed in patient (M.N) a decrease of the Cobb angle from 28° to 26°, a stronger axial cross-linked self-correction without using Brixia brace, preservation of a shoulder symmetric alignment, an amelioration of the frontal head-neck alignment, an astenic dorsal attitude without using BRIXIA brace; angle spine rotation, refered to the principal scoliotic curve, showed a consistent decrease from 11° to 6° at time T4;
Figure 29: Orthostatic total spine X-ray of patient P1 – M-N. proceeding from time T0 to time T4 (own elaboration).
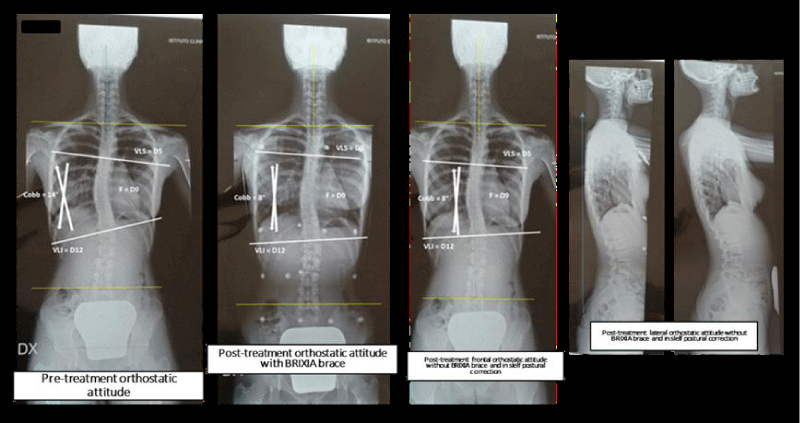
• at time T4 (Figure 30), we observed in patient (L.F) a decrease of the Cobb angle from 14° to 8°, a similar axial cross-linked self-correction with and without using Brixia brace, preservation of a shoulder symmetric alignment, an amelioration of the frontal head-neck alignment, an astenic dorsal attitude without using BRIXIA brace; angle spine rotation, refered to the principal scoliotic curve, showed a consistent decrease from 9° to 3° at time T4;
Figure 30: Orthostatic total spine X-ray of patient P2 – L.F. proceeding from time T0 to time T4 (own elaboration).
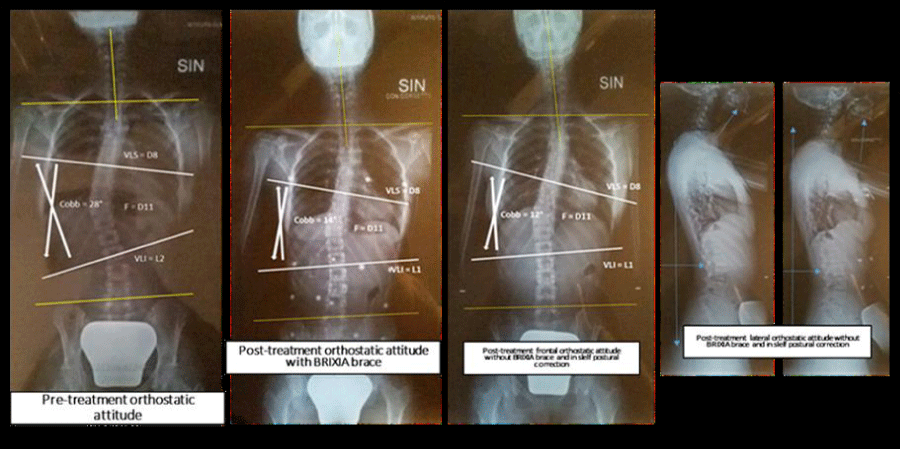
• at time T4 (Figure 31), we observed in patient (P.E) a decrease of the Cobb angle from 28° to 12°, a similar axial cross-linked self-correction with and without using Brixia brace, preservation of a shoulder symmetric alignment, an amelioration of the frontal head-neck alignment, an astenic dorsal attitude without using BRIXIA brace; angle spine rotation, refered to the principal scoliotic curve, showed a consistent decrease from 9° to 5° at time T4;
Figure 31: Orthostatic total spine X-ray of patient P3 – P.E. proceeding from time T0 to time T4 (own elaboration).
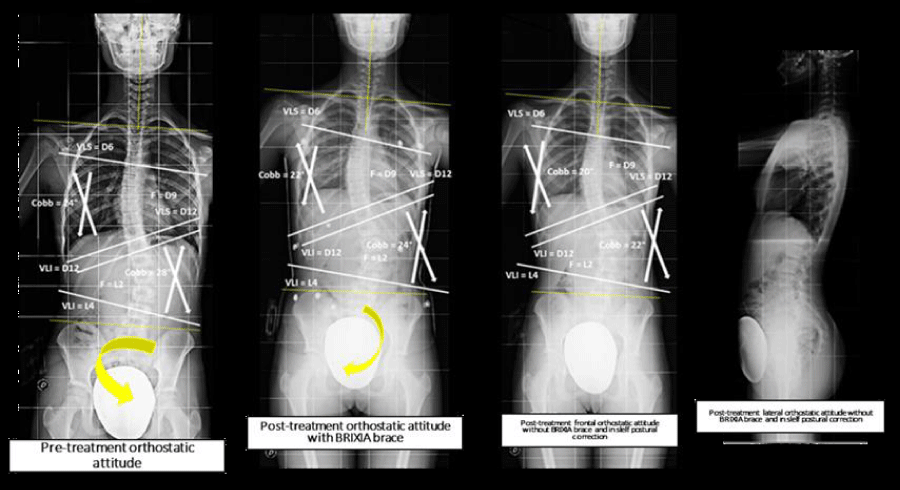
• at time T4 (Figure 32) we observed in patient (F.M) a decrease of the Cobb angle from 28° to 22°, a similar axial cross-linked self-correction with and without using Brixia brace, a slight modification of the shoulder asymmetric alignment, an amelioration of the frontal head-neck alignment, an astenic dorsal attitude without using BRIXIA brace; an evident hip derotation with the achievement of a symmetry between right and left iliac spine; angle spine rotation, referred to the principal scoliotic curve, showed a consistent decrease from 13° to 4° at time T4;
Figure 32: Orthostatic total spine X-ray of patient P4 – F.M. proceeding from time T0 to time T4 (own elaboration).
• at time T4 (Figure 33) we observed in patient (S.S) a decrease of the Cobb angle from 20° to 10°, a stronger axial cross-linked self-correction without using Brixia brace, preservation of a shoulder symmetric alignment, an amelioration of the frontal head-neck alignment, an astenic dorsal attitude without using BRIXIA brace; angle spine rotation, refered to the principal scoliotic curve, showed a consistent decrease from 10° to 2° at time T4.
Figure 33: Orthostatic total spine X-ray of patient P5 – S.S. proceeding from time T0 to time T4 (own elaboration).
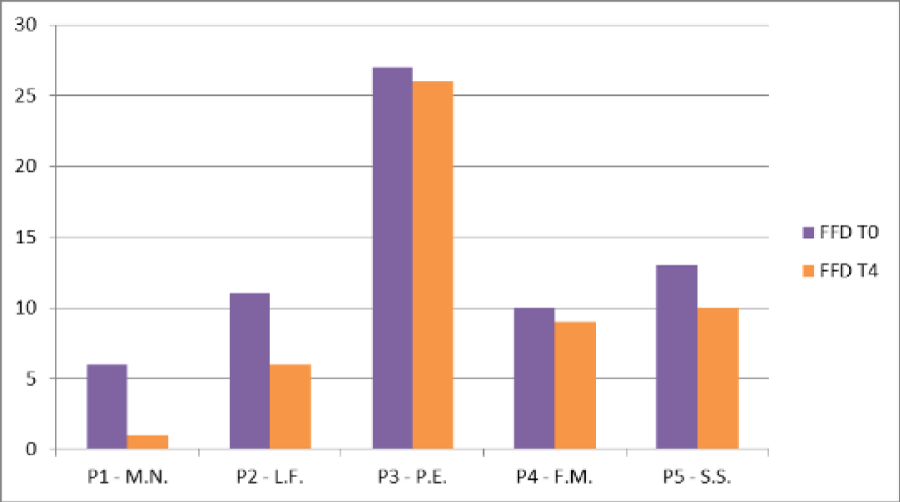
FFD (Finger Floor Distance)
In line with our study design, we acquired for each patient the graw data of the FFD (Finger Floor Distance) proceeding from time T0 to time T4 (Table 9).
| Table 9: Resume of the time-related trend course of FFD proceeding from time T0 to time T4 (own elaboration). | ||
| Patient | FFD T0 | FFD T4 |
| M.N. | 6 cm | 1 cm |
| L.F. | 11 cm | 6 cm |
| P.E. | 27 cm | 26 cm |
| F.M. | 10 cm | 9 cm |
| S.S. | 13 cm | 10cm |
The analysis of the trend course of FFD showed a decrease of this parameter proceeding from time T0 to time T4, as reported in figure 34.
Particularly:
1. patient (M.N) reduced FFD value from 6cm to 1cm;
2. patient (L.F) reduced FFD value from 11cm to 6cm;
3. patient (P.E) reduced FFD value from 27cm to 26cm;
4. patient (F.M) reduced FFD value from 10cm to 9cm;
5. patient (S.S) reduced FFD value from 13cm to 10cm.
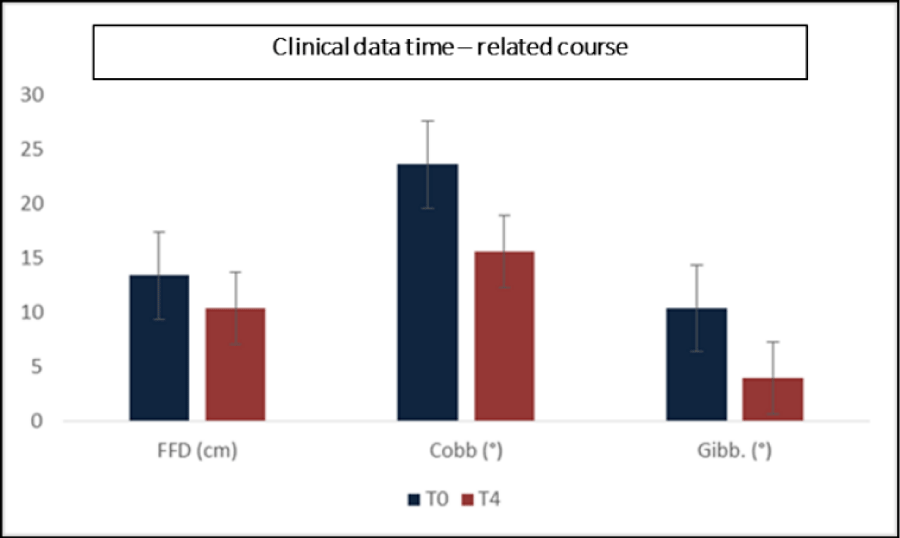
Comparative analysis of clinical data acquired at time T0 and T4
For the aim of our study a parametric one-sample t-test was used to evaluate the parametric infragroup time-related modifications; similarly a non-parametric Wilcoxon post-hoc test was used to realize a comparative analysis of our clinical mean data (FFD, Cobb angle and angle spine rotation) acquired at time T0 and time T4 (Table 10). We observed a significant statistical modification of the Finger Floor Distance (FFD) proceeding from time T0 to time T4 (M= 13,40 vs M= 10,40; t(4)= 3,354; p<0,05), a significant statistical decrease of Cobb angle proceeding from time T0 to time T4 (M= 23,80 vs M= 15,60; (t)= 3,381; p<0,05), a significant statistical decrease of the angle spine rotation proceeding from time T0 to time T4 (M= 10,40 vs M= 4; (t)= 6,901; p<0,05) (Figure 35).
Figure 35: Comparative time – related course analysis of clinical data mean values proceeding from time T0 to time T4 (own elaboration).
| Table 10: Mean value and DS of clinical data proceeding from time T0 to time T4 (own elaboration. | ||
| Mean Value | Std.Dev. | |
| FFD T0 | 13.,4 | 8,02 |
| FFD T4 | 10,4 | 9,40 |
| Cobb To | 23,6 | 6,39 |
| Cobb T4 | 15,6 | 7,92 |
| Gibbosita To | 10,4 | 1,67 |
| Gibbosita T4 | 4 | 1,58 |
Comparative analysis of RMS data acquired at time T2, T3 and T4
A parametric one-sample t-test was used to evaluate the parametric infragroup time-related modifications; similarly a non-parametric Wilcoxon post-hoc test was used to realize a comparative analysis of our RMS data acquired in the six study conditions at time T2, T3 and T4. We observed:
- no significant modification of RMS data at time T2, T3 and T4 with and without BRIXIA brace in sitting resting position (SiRP);
- no significant modification of RMS data with and without BRIXIA brace in a Sitting Recruiting Position with a so called pneumothorax thrust (SiRCP);
- no statistical significant modification of RMS data with and without BRIXIA brace in standing resting position (StRP);
- a significant statistical difference of RMS change from time T3 to time T4 in StRCP condition (Standing Recruiting Position) with a so-called pneumothorax thrust by using BRIXIA brace: t(4)= 2,844; p<.05 (t test); this result was confirmed by the non-parametric Wilcoxon post-hoc test: Z= -2,023; p<.05;
- by using BRIXIA brace and in anterior bending condition (BA), a significant statistical difference of RMS from time T2 and T3: t(4)= 3,626; p<.05 (t test); this result was confirmed by the non-parametric Wilcoxon post-hoc test: Z=-2,023 p<.05;
- no statistical significant modification of RMS data with and without BRIXIA brace was observed in Anterior Trunk Recruiting Bending (BARC) condition.
Comparative analysis of RMS data versus clinical data
In line with the aim of this study, we realized a comparative and time-related analysis between our clinical and RMS data. Particularly: Cobb angle trend, acquired at time T0, showed a statistical significant correlation with RMS data, acquired at time T4 in BARC condition and without BRIXIA brace, and with RMS data acquired at time T4 with BRIXIA brace use (p<0,05).
Discussion
In the last years many studies tried to demonstrate the usefulness of paraxial muscle recruitment analysis in patients affected by adolescent idiopathic scoliosis [14-22]. It was clear how the paraxial muscle chains could be important in motor and perceptive engrammation of postural self correction strategies. In line with our study design, recruited patients underwent to a a SEMG (BTS-FREEMG) analysis of paraxial selected muscles wearing our BRIXIA brace in six study conditions at time T2 (rehabilitative treatment onset by using BRIXIA brace), at time T3 (after 2 months from T2) and time T4 (after 5 months from time T3). A comparative analysis of our SEMG data showed different trends in all patients recruited proceeding from time T2 to time T5. We interpreted these results as a consequence of: a. age difference of our patients which conditioned the anthropometric development and a different response of each single patient; b. different axial dysmorphyc attitudes of each single patient which could induce different integrated treatment responses; c. a necessary personalization of a short-term rehabilitative treatment protocol which could induce a different and not uniform postural self correction acquisition. Compared with the study of Kwok et al. [14], our RMSsEMG results offered a very interesting point of view in term of functional and rehabilitative outcome interpretation. Particularly, we observed:
• at time T2, an homogeneous grade of symmetric paraxial muscle recruitment acquisition without using spine brace (53,3%) and by using Chêneau and BRIXIA brace (46,7%); specifically, around 57,14% of our patients used BRIXIA brace and 42,86% Chêneau brace; the most homogeneous response was acquired in BA study condition and the symmetric paraxial muscle recruitment acquisition without using spine brace observed in 80% of our patients; the most grade of not homogeneous muscle activity response was observed in SiRP and StRCP study conditions;
• at time T3, an homogeneous grade of symmetric paraxial muscle recruitment acquisition by using BRIXIA brace (56,7%); all patients recruited (100%) showed in SiRCP study condition the most homogeneous and symmetric paraxial muscle recruitment by using BRIXIA brace; in SiRP and StRCP study condition this trend was observed in 80% of our patients with a reversion of this trend in StRP and BRAC conditions;
• at time T4, an immodification of the grade of symmetric paraxial muscle recruitment acquisition in 56,7% of patients who were using BRIXIA brace; all patients recruited (100%) showed in BARC study condition the most homogeneous and symmetric paraxial muscle recruitment by using BRIXIA brace, while in SiRP condition this trend was observed in 80% of our patients;
• proceeding from time T2 to time T4, a specific muscle recruitment pattern in 3 of 5 patients recruited: a. in patient P1 (M.N.) the most homogeneous and symmetric paraxial muscle recruitment was observed by using BRIXIA brace in SiRP condition; b. in patient P3 (P.E.) the most homogeneous and symmetric paraxial muscle recruitment, refered to the main scoliotic curve, was observed in BA condition by activating an axial cross-linked self-correction; c. in patient P4 (F.M.) the most homogeneous and symmetric paraxial muscle recruitment was observed in StRP and BA conditions by activating an axial cross-linked self-correction.
A critical interpretation of these results can be resumed in few points:
• the individual rehabilitative acquisition of an axial cross-linked self-correction was perceived and acquired in different ways at the end of our integrated treatment course;
• our data demonstrated the perceptive and rehabilitative value of BRIXIA brace by facilitating the acquisition and activation of axial cross-linked self-correction strategies; this response was not uniform in all patients recruited but more significant in patient P1 and P5;
• the innovative manufacturing process of BRIXIA brace, personalized and adapted to patient’s own postural attitude, could produce different biomechanical responses in term of paraxial muscle recruitment remodulation; without paraxial push shells and escapes areas, BRIXIA allowes to imprint mechanically and from a proprioceptive point of view a default trunk postural correction; by using this kind of spine brace, patients does not feel empty areas between the skin and the device with a secondary increase of its proprioceptive value and induction of an immediate cross-linked trunk alignment;
• BRIXIA spine brace can be considered as a “second skin” that trough its structural plasticity and high proprioceptive and rehabilitative value can dynamically help patients to corticalize postural and trunk alignment;
• Brixia brace allows to increase patient’s postural sense and core stability with a secondary increase of feedback and feedforward strategies of balance control;
• Brixia brace allows to increase patient’s cross-linked paraxial muscle recruitment with a strong lateral and rotational trunk corrective imprinting during the rehabilitative postural treatment;
• the corrective value of this kind of dynamic and asymmetric spine brace reflects exactly the dynamic principles of a guided and cross-crowl postural rehabilitative treatment course in all patients affected by AIS.
In line with the aim of this study, we realized a comparative and time-related analysis between our clinical and RMS data. Particularly: Cobb angle trend showed a statistical significant correlation with RMS data, acquired at time T4 in BARC condition and without BRIXIA brace. These results were in line with a significant modification of postural attitude, grade of re-learning capacity of self-correction strategies and with a significant decrease of the main scoliotic curve in all patients recruited for this study. We can interpret the sensible decrease of the spine angle rotation as a result of paraxial muscle recruitment modification acquired at the end of the rehabilitative course and registered with the BTS - FREEMG analysis.
As demonstrated by the Visual Postural Analysis trend, our rehabilitative model showed in this study a sensible capacity to modify patient’s individual sense of posturality and to increase the acquisition of axial cross-linked self-correction strategies with a rebalancing between the anterior and posterior kinetic muscle chains recruitment. These rehabilitative principles were perfectly in line with the perceptive and pro-rehabilitative value of our innovative BRIXIA brace: with a daily correct management and development of self-correction strategies, acquired by using BRIXIA brace, functional pro-corrective informations were performed with the supervision of the Physiotherapist.
In conclusion, our study will underline the professional attitude of all physiotherapists to use in a critical and task-specific way our dynamic and asymmetric spine orthesis that allows to achieve:
1) an individualized peripheral neuromodulation of patient’s sense of postural attitude (peripheral perceptive re-modulation of paraxial muscle recruitment)
2) a neurorehabilitative re-learning device of postural self-correction strategies (peripheral neurosensitive facilitation of a dynamic process of motor corticalization)
3) an increase of patient’s quality of life in term of appearance and relational sense (life-impact device-related).
In the next future, multiprofessional approach and a task-specific knowledge will be request to offer to all patients affected by AIS the best treatment options secondary to a perfect integration between rehabilitation and the use of a personalized spine orthosis.
References
- Sarwahi V, Sugarman EP, Wollowick AL, Amaral TD, Lo Y, et al. Prevalence, Distribution, and Surgical Relevance of Abnormal Pedicles in Spines with Adolescent Idiopathic Scoliosis vs. No Deformity: A CT-Based Study. J Bone Joint Surg. 2014; 96: 92. Ref.: https://goo.gl/5274wX
- Longworth B, Fary R, Hopper D. Prevalence and predictors of adolescent idiopathic scoliosis in adolescent ballet dancers. Arch Phys Med Rehabil. 2014; 95: 1725-1730. Ref.: https://goo.gl/1s3Ybz
- Lee JY, Moon SH, Kim HJ, Park MS, Suh BK, et al. The Prevalence of Idiopathic Scoliosis in Eleven Year-Old Korean Adolescents: A 3 Year Epidemiological Study. Yonsei Med J. 2014; 55: 773-778. Ref.: https://goo.gl/DhLFLP
- Théroux J, May SL, Fortin C, Labelle H. Prevalence and management of back pain in adolescent idiopathic scoliosis patients: A retrospective study. Pain Res Manag. 2015; 20: 153-157. Ref.: https://goo.gl/hZZ2yY
- Cheng JC, Castelein RM, Chu WC, Danielsson AJ, Dobbs MB, et al. Adolescent idiopathic scoliosis. Nat Rev Dis Primers. 2015; 24:. Ref.: https://goo.gl/RKGVn7
- Berdishevsky H, Lebel VA, Bettany-Saltikov J, Rigo M, Lebel A, et al. Physiotherapy scoliosis-specific exercises - a comprehensive review of seven major schools. Scoliosis Spinal Disord. 2016; 11:. Ref.: https://goo.gl/Pu9jy9
- Nault ML, Allard P, Hinse S, Le Blanc R, Caron O, et al. Relations between standing stability and body posture parameters in adolescent idiopathic scoliosis. Spine. 2002; 27: 1911-1917. Ref.: https://goo.gl/QSXQ8L
- Odermatt D, Mathieu PA, Beauséjour M, Labelle H, Aubin CE. Electromyography of scoliotic patients treated with a brace. J Orthop Res. 2003; 21: 931-936. Ref.: https://goo.gl/Hsu1nT
- Chwała W, Koziana A, Kasperczyk T, Walaszek R, Płaszewski M. Electromyographic assessment of functional symmetry of paraspinal muscles during static exercises in adolescents with idiopathic scoliosis. BioMed Res Int. 2014;. Ref.: https://goo.gl/BLh1df
- Farahpour N, Younesian H, Bahrpeyma F. Electromyographic activity of erector spinae and external oblique muscles during trunk lateral bending and axial rotation in patients with adolescent idiopathic scoliosis and healthy subjects. Clin Biomech. 2015; 30: 411-417. Ref.: https://goo.gl/QhzYcn
- Hawes MC. The use of exercises in the treatment of scoliosis: an evidence-based critical review of the literature. Pediatric Rehabilitation. 2003; 6: 171-182. Ref.: https://goo.gl/FnQ4To
- Chen YT, Kwon MH, Fox EJ, Christou EA. Altered activation of the antagonist muscle during practice compromises motor learning in older adults. J Neurophysiology. 2014; 112: 1010-1019. Ref.: https://goo.gl/4SPq9V
- Vallbo AB, al-Falahe NA. Human muscle spindle response in a motor learning task. J Physiology. 1990; 421: 553-568. Ref.: https://goo.gl/Hgej74
- Kwok G, Yip J, Cheung MC, Yick KL. Evaluation of Myoelectric Activity of Paraspinal Muscles in Adolescents with Idiopathic Scoliosis during Habitual Standing and Sitting. BioMed Res Int. 2015;. Ref.: https://goo.gl/udNTpJ
- Avikainen VJ, Rezasoltani A, Kauhanen HA. Asymmetry of paraspinal EMG-time characteristics in idiopathic scoliosis. J Spinal Disord. 1999; 12: 61-67. Ref.: https://goo.gl/w9JiZk
- O’Sullivan PB, Grahamslaw KM, Kendell MM, Lapenskie SC, Moller NE, et al. The effect of different standing and sitting postures on trunk muscle activity in a pain-free population. Spine. 2002; 27: 1238-1244. Ref.: https://goo.gl/r4MZyW
- Cheung J, Halbertsma JPK, Veldhuizen AG, Sluiter WJ, Maurits NM, et al. A preliminary study on electromyographic analysis of the paraspinal musculature in idiopathic scoliosis. European Spine Journal. 2005; 14: 130-137. Ref.: https://goo.gl/ryM75z
- Youdas JW, Boor MMP, Darfler AL, Koenig MK, Mills KM. et al. Surface electromyographic analysis of core trunk and hip muscles during selected rehabilitation exercises in the side-bridge to neutral spine position. Sports Health: A Multidisciplinary Approach. 2014; 6: 416-421. Ref.: https://goo.gl/GwUuu5
- Packer AC, Pires PF, Dibai-Filho AV, Rodrigues-Bigaton D. Effect of upper thoracic manipulation on mouth opening and electromyographic activity of masticatory muscles in women with temporomandibular disorder: a randomized clinical trial. J Manipulative Physiol Ther. 2015; 38: 253-261. Ref.: https://goo.gl/bEzJKZ
- Feldwieser FM, Sheeran L, Meana-Esteban VS. Electromyographic analysis of trunk-muscle activity during stable, unstable and unilateral bridging exercises in healthy individuals. Eur Spine J. 2012; 21: 171-186. Ref.: https://goo.gl/bt9f93
- Lu WW, Hu Y, Luk KDK, Cheung KMC, Leong JCY. Paraspinal muscle activities of patients with scoliosis after spine fusion: an electromyographic study. Spine. 2002; 27: 1180-1185. Ref.: https://goo.gl/GJbKDc
- Park KH, Oh JS, An DH, Yoo WG, Kim JM, et al. Difference in selective muscle activity of thoracic erector spinae during prone trunk extension exercise in subjects with slouched thoracic posture. PMR. 2015; 7: 479-484. Ref.: https://goo.gl/cX6SQx