Research Article
Effectiveness of Soft Tissue Mobilisation as an adjunct to the Conventional Therapy in patients with Ankylosing Spondylitis

Patitapaban Mohanty*
Associate Professor (Physiotherapy), Swami Vivekanand National Institute of Rehabilitation Training and Research, Olatpur, Bairoi, Cuttack, India*Address for Correspondence: Patitapaban Mohanty, Ph.D, Associate Professor (Physiotherapy), Swami Vivekanand National Institute of Rehabilitation Training and Research, Olatpur, Bairoi, Cuttack, India, Email: ppmphysio@rediffmail.com
Dates: Submitted: 20 December 2017; Approved: 03 January 2018; Published: 05 January 2018
How to cite this article: Mohanty P. Effectiveness of Soft Tissue Mobilisation as an adjunct to the Conventional Therapy in patients with Ankylosing Spondylitis. J Nov Physiother Rehabil. 2018; 2: 001-014. DOI: 10.29328/journal.jnpr.1001016
Copyright License: © 2017 Mohanty P. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Chronic low back pain; Duration of pain; Severity of pain; Lung function
Abstract
Introduction: The HRMT (Human Resting Myofasial Tone) factor plays an important role to initiate the trigger the inflammation at the disease site in Ankylosing spondylitis (AS) as in all spondyloarthropathies. The incidence of fibromyalgia is higher in AS and a limiting factor to undergo the exercise program.
Aim of the study: To know the effectiveness of soft tissue mobilisation in patients with Ankylosing Spondylitis when it used as an adjuncts to the conventional exercises.
Methodology: 40 subjects were randomly assigned in to experimental and conventional group. Experimental group (n=20) received conventional exercises along with soft tissue mobilisation and the conventional group (n=20) received only conventional exercises (flexibility exercises, aerobic exercise and breathing exercise) for a period of 4 weeks, 5days/week.
Results: The result of the study showed that both the conventional and experimental groups improved significantly in stiffness, pain and physical function aspects after treatment. However the experimental group had a greater change as compared to conventional group.
Conclusion: The study demonstrates that soft tissue mobilisation has an effect when it used before the conventional exercise in patients with ankylosing spondylitis.
Introduction
Ankylosing spondylitis (AS) is a chronic, progressive and inflammatory disorder, primarily affecting the sacroiliac joints of the pelvis, the axial skeleton also including the rib cage, but peripheral joints, entheses and extra-articular sites are also involved [1]. Pain, stiffness, and bony ankylosis cause variable degrees of restricted mobility of the spine with consequent loss of functional capacity having impact on physical, social and psychological aspect of living being and impairment and disability are the important components of the patient’s perception of the disease [2-4]. It is the prototype and the most severe form of the spondyloarthritis (SpA), with AS prevalence per 10,000 population as 23.8 cases in Europe, 16.7 in Asia, 31.9 in North America, 10.2 in Latin America and 7.4 in Africa [5]. Age of onset of AS begins in late adolescent or early adulthood, according to the study Prakash S et al. in India it is 21.2 year in average, which is the most productive period of time, thereby causing a significant health burden to society [6].
Establishing an optimal management protocol of AS by the Assessment of Spondyloarthritis International Society-European League against Rheumatism (ASAS/EULAR) working groups, combination of non-pharmacological and pharmacological treatment came under main stream [7]. The only available non-pharmacological measure in AS management is physiotherapy aiming to prevent and/or retard restriction of spinal mobility, improving pain and stiffness as long as possible [8]. To avoid stiffening in a flexed posture and to maintain/improve functional capacity and QOL, patient education and regular exercise is effective in patient under TNF inhibitors [9]. In order to learn specific exercise to continue, at the initial phase i.e. first years of the disease multidisciplinary in-patient rehabilitation program is needed that had a positive effect on disease activity, pain, function and well-being [10].
There is recommendation of active physical therapy intervention over passive physical therapy like modalities, any form of massage, trigger point release etc. for the treatment of Ankylosing spondylitis and Non-radiographic Axial Spondylitis by American college of Rheumatology/spondylitis, Association of America/spondyloarthritis Research and Treatment Network 2015, thereby limited literature options are found other than conventional exercises [11]. Considering the current evidence in management of AS, which includes primarily educational training, flexibility exercises, breathing exercise, hydrotherapy, pilates training, aerobic training, global postural re-education (GPR)etc, there is a more need of literature of intervention that targets to reduce the triggering factor of inflammation in AS [12-18].
There is incidence of fibromyalgia in patients with AS and its symptoms like pain, fatigue, anxiety and depression may be the factors, limiting a person to motivate and undergo home exercise program [19]. Mobilising the soft tissue, the effects like pain relief by activating cutaneous receptors that block the nociceptive stimulate, reduction of tone by relaxation and stretching the shorten structures can be utilise to have adjunct effects on conventional exercise in patients with AS [20]. Considering the above facts and incidence the purpose of the study is to see the effectiveness of soft tissue mobilisation when it is added to the conventional therapy protocol of AS patients.
Aim of the Study
To find out the effect of soft tissue mobilisation as an adjunct therapy to the conventional exercise in patients with ankylosing spondylitis.
Methodology
Study design: Pre-test post-test conventional group experimental design.
Subjects: 40 patients diagnosed as ankylosing spondylitis by modified New York criteria were recruited from the MS unit of Physiotherapy department, SVNIRTAR after fulfilling the inclusion and exclusion criteria and randomly assigned into two groups.
Inclusion criteria: a) Radiological grading: stage I and II according to the AS staging system based on modified New York criteria 1984 b) Stages I, II and III AS based on classical Steinbrocker functional criteria of Rheumatic disease c) Age >45 years
Exclusion criteria: a) Had any spinal surgery and recently joint replacement surgery b) Systemic organic involvement c) Sever co morbidity
Procedure: 40 patients (38males, 2 females) were recruited with mean age (32.97±6.78) years from the physiotherapy department of SVNIRTAR after fulfilling the inclusion and exclusion criteria. Patients were evaluated through an assessment Performa and consent form was taken after giving verbal instruction and explanations regarding the study. Before initiation of treatment the baseline values for all dependent variable i.e. BASMI, BASDAI, BASFI and chest expansion was taken and intervention was started on the same day.
a) Bath Ankylosing Spondylitis Metrology Index (BASMI): It asses accurately the axial status (cervical, dorsal and lumbar spine, hip and pelvic soft tissue) of individuals with AS and defines clinical significance in spinal mobility. 5 simple clinical measurements such as 1) Tragus to wall distance, 2) Lumbar side flexion, 3) Modified Schober’s, 4) Cervical rotation , 5) Intermalleolar distance were included in the index. [21].
b) Bath Ankylosing Spondylitis Disease Activity Index (BASDAI): It is the gold standard for measuring and following disease activity in Ankylosing Spondylitis [22]. BASDAI consists of 10cm visual analogue scales used to answer 6 questions pertaining to the 5 major symptoms of AS such as Fatigue, Spinal pain, Joint pain/swelling, Areas of localized tenderness, Morning stiffness. A BASDAI score >4 is internationally accepted to indicate active disease
c) Bath Ankylosing Spondylitis Functional Index (BASFI): This is a set of 10 questions designed to determine the degree of functional limitation in those with AS. It is measured using a visual analogue scale (ranging from 0 being easy and 10 being impossible) and the questions are focused on the person’s ability to perform specific functional tasks. The first 8 questions consider activities related to functional anatomy, such as putting on socks with or without help and climbing steps with or without using a handrail. The final two questions assess the patients’ ability to cope with everyday life. It is included in the ASAS core sets for AS assessment. The BASFI has shown to have high levels of validity and reliability when measuring functional ability in AS [23].
d) Chest expansion: Chest expansion is defined as the difference in chest circumference at maximal inspiration and expiration at the level of the fourth intercostal space [14].
Subjects were randomly assigned into 2 groups (group 1 & group 2). All the patients were taken consultation from rheumatologist and were under medication. The patients with shoulder and hip involvement were also included and specific treatment was given.
Group-1 (conventional): 20 subjects (19 male &1 female) with mean age 35.35±7.04 received conventional flexibility exercise, aerobic exercise and breathing exercise.
• Flexibility exercises
a) Stretching of neck side flexors, triceps, hip flexors, abductors and pyrifomis. Each muscle was taken to its maximum length with little discomfort but no pain, maintained the hold for 30 sec and repeated for 5 times.
b) ROM exercises
c) Strengthening exercise: static quadriceps, glutei, hip abductor and chin tucking 2 sets of exercise twice daily, each set 10 repetition and 2-3 min rest in between each set.
• Aerobics exercises in form of static cycling 30 min thrice a week.
• Breathing exercise; deep breath through nose and expanding the chest with abduction and elevation of both arms and spine extension. Expiration through mouth, sinking the abdomen in with adduction and flexion of spine.
Group-2 (experimental): 20 subjects (19 male & 1 female) with mean age 30.60±5.74 treated by soft tissue mobilisation of periscapular and paravertebral muscles along with conventional treatment.
• Soft tissue mobilisation given by the heel of the one hand reinforced by other hand, therapist applied sustained pressure by using the body weight till the motion barrier reached in the direction of downward and laterally for leavator scapulae and upper trapezius from cervical spinous processes to the superior ZDFSVVVXV of scapula and laterally and outward from the thoracic spinous processes towards medial ZDFSVVVXV of scapula for rhomboids and middle trapezius andcephalo-caudally and caudalo-cephalic direction with maintained pressure throughout the length of paravertebral muscle.
All the patient were taught and encouraged to do home exercise programme. Treatment was given 5 days in a week for 4 weeks and at the end of 4 weeks of intervention, post measurement for all dependent was taken again.
Data Collection: Measurements were taken prior to the beginning of treatment (pre-test) and were repeated after completion of four weeks (post-test).
Data Analysis: The dependent variables were analysed using a 2×2 ANOVA, repeated measures on second factor. There was one between factor (group) with two levels (groups: experimental, conventional) and one within factor (time) with two levels (time: pre, post). Post-hoc analysis was done using a 0.05 level significance.
Results
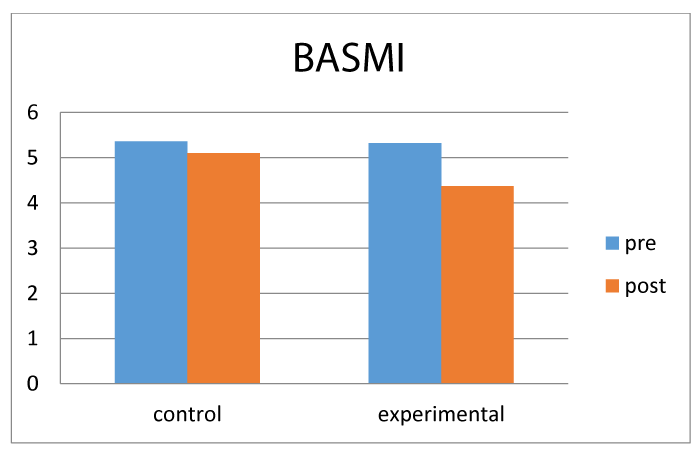
The graph 1 illustrates, there was reduction in BASMI score in both groups from pre to post treatment measurements. But there was comparative more reduction in experimental group than the conventional group.
There was a main effect for time F(1,38,0.05)=224.519, p=0.000. There was no main effect for group F(1,38,0.05)=0.964, p=0.332. The main effects were qualified into time x group interaction F(1,38,0.05) =73.010, p=0.000
Post hoc analysis showed though both group improved but a significant difference in BASMI score in the experimental group over conventional group when soft tissue mobilisation used as adjunct.
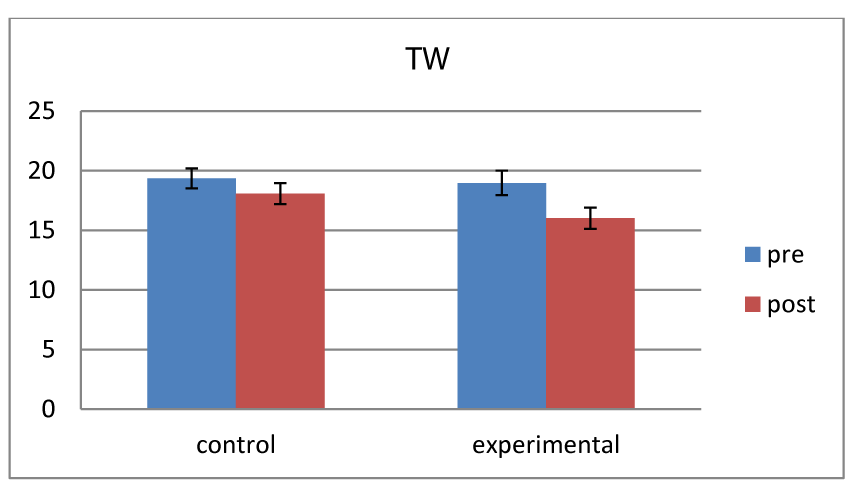
The graph 2 shows, there was greater reduction in tragus to wall distance in experimental than conventional group.
There was a main effect for time F(1,38,0.05)=94.433, p=0.000. The main effect were qualified for time x group interaction F(1,38,0.05)=15.022, p=0.004. There was no main effect for group F(1,38,0.05)=0.910, p=0.345.
Post hoc test shows there was significant reduction in score for both the groups. However, the experimental group showed greater reduction than conventional group at the end of 4 weeks.
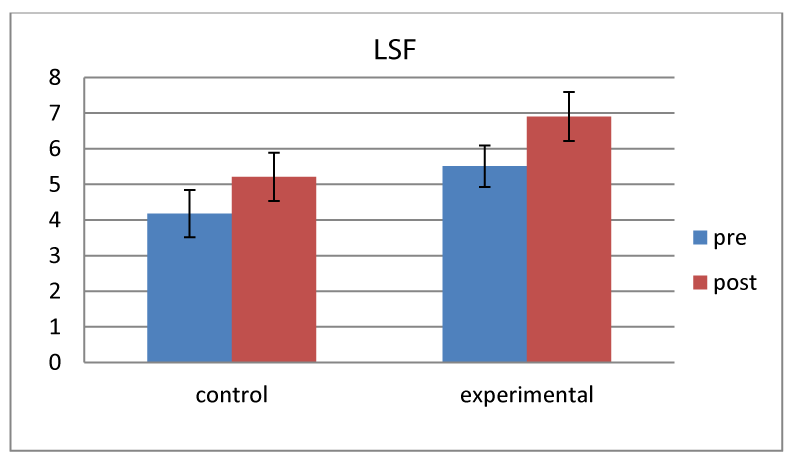
As the graph 3 illustrates, there was improvement of lumbar side flexion measured by difference in finger to floor distance in both groups. However, there was greater improvement in experimental group than conventional group.
There was a main effect for time F(1,38,0.05)=99.790, p=0.000. The main effect were qualified for time x group interaction F(1,38,0.05)=30.662, p=0.000. There was no main effect for group F(1,38,0.05)=1.694, p=0.201.
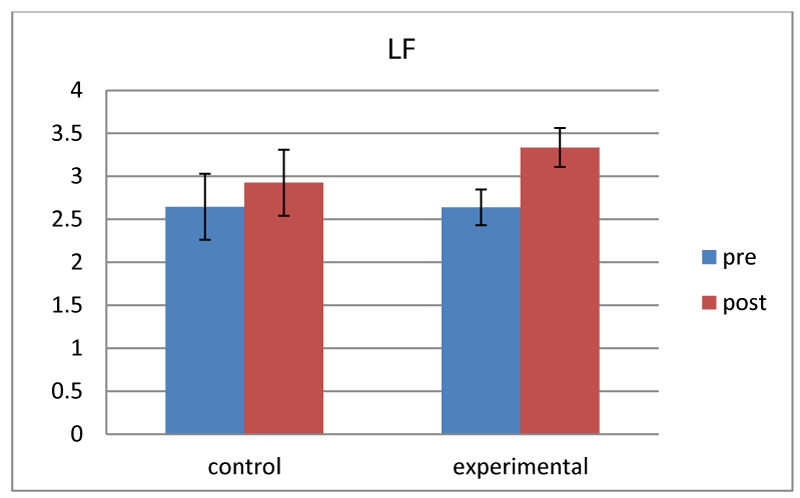
As the graph 4 shows, there was greater improvement in lumbar flexion measured by modified schober test in experimental group than conventional group after a period of 4 weeks.
There was a main effect for time F(1,38,0.05)=158.333, p=0.000. The main effects were also qualified into time x group interaction F (1,38,0.05)=28.683, p=0.000. There was no main effect for group F (1,38,0.05)=0.212, p=0.648.
Post hoc test shows there was improvement in lumbar flexion for both the groups, whereas the experimental group shows more than conventional group.
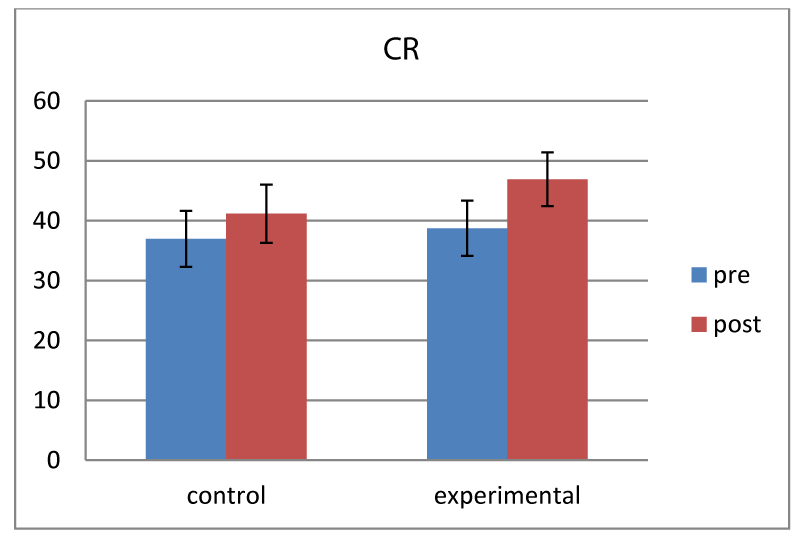
The graph 5 shows, there was an increase in cervical rotation in both groups from pre to post-test measurements. But there was more in experimental group than conventional group.
There was a main effect for time F(1,38,0.05)=175.466, p=0.000. There was also main effect for time x group interaction F(1,38,0.05)=18.106, p=0.000. There was no main effect for group F(1,38,0.05)=0.331, p=0.569.
Post hoc test analysis shows there was improvement of function in both the groups. However, there was more improvement in experimental group compared to conventional group.
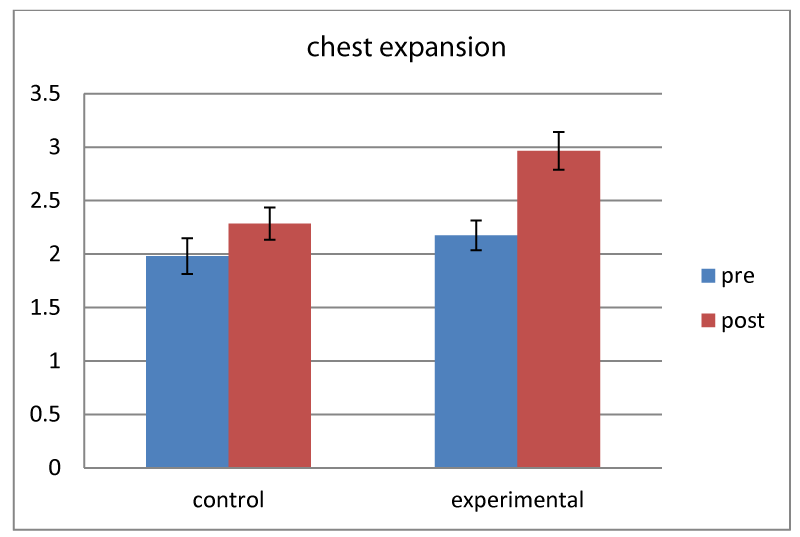
The graph 6, there was increase in chest expansion measured in cm in both the groups from pre-treatment to post treatment after 4 week with more increase in experimental group than conventional group.
There was main effect for time F(1,38,0.05)=104.803, p=0.000. The main effect also qualified for time x group interaction F(1,38,0.05)=20.560, p=0.000. There was no main effect for group F(1,38,0.05)=4.004, p=0.053.
Post hoc test shows there was significant improvement in score for both the groups. However, the experimental group showed greater increase than conventional group at the end of 4 weeks.
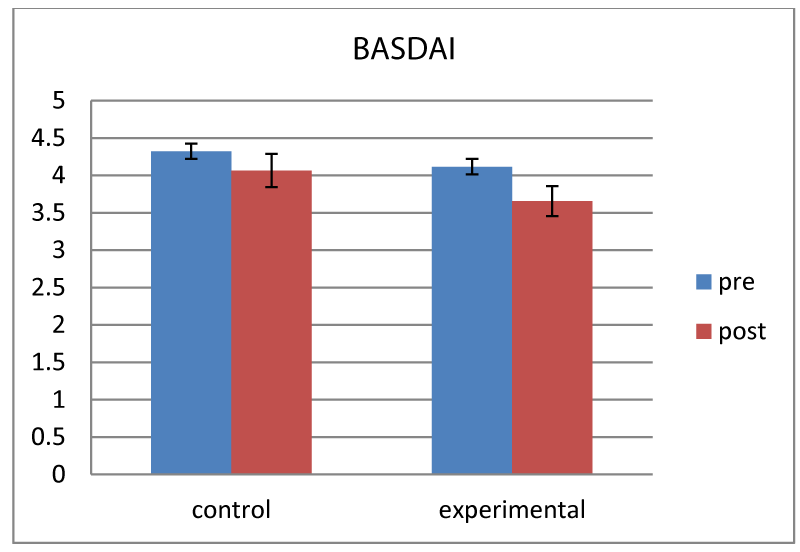
As the graph 7 shows, there was reduction in BASDAI score in both the groups from pre-treatment to post treatment measurements with more reduction in experimental group than conventional group.
There was a main effect for time F(1,38,0.05)=62.717, p=0.000. The main effects were also qualified into time x group interaction F(1,38,0.05)=5.156, p=0.029. There was no main effect for group F(1,38,0.05)=1.011, p=0.321.
Post hoc test shows there was reduction in disease activity for both the groups, whereas the experimental group shows more than conventional group.
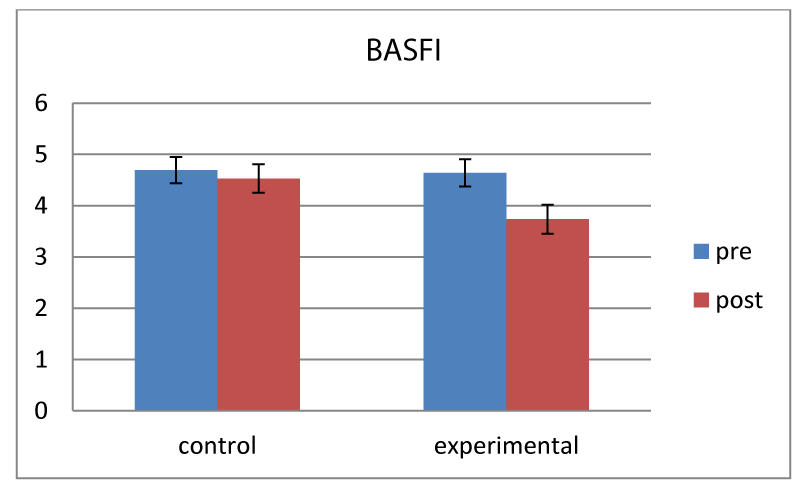
The graph 8 reveals there was decrease in BASFI score in both groups, seen in pre to post test. But there was more in experimental group than conventional group.
There was a main effect for time F(1,38,0.05)=40.527, p=0.000. There was also main effect for time x group interaction F(1,38,0.05)=19.384, p=0.000. There was no main effect for group F(1,38,0.05)=1.288, p=0.264.
Post hoc test analysis shows there was improvement of function in both the groups. However, there was more improvement in experimental group compared to conventional group.
Discussion
Overall results of the study, both conventional and experimental group showed improvement in flexibility measured by BASMI (tragus to wall, cervical rotation, lumbar flexion and lumbar side flexion) and chest expansion, disease activity measured by BASDAI and physical function measured by BASFI after 4 weeks of intervention in patient with ankylosing spondylitis. Though there was no statistical significant between both the group, clinically there was improvement more in experimental group.
ROM in conventional group
The limitation of joint range of motion due to soft tissue structure was benefited by our flexibility exercises that include the stretching, ROM exercise and strengthening exercises [24]. The shortening of muscle is due to structural changes through healing by scarring, following inflammation and active tension due to reflexive spasm and contraction [25].
Stretching the tissue increases the muscle length which inversely related to decreased muscle tension. When a muscle is lengthened, the stretch force is transmitted to the muscle fibers via the connective tissue (endomysium and perimysium) in and around the fiber [26]. There is molecular interaction link between contractile and noncontractile units of muscle resulting elongation [27]. Regular stretching followed by ROM exercises and strengthening exercises to maintain the gained length for 4 weeks showed the improvement in flexibility of the spine in our conventional group.
Chest expansion measurement is usually evaluated for the chest wall mobility, respiratory muscle function [28,29]. Increase in thoracic kyphosis in patient with AS leads to limitation of chest wall excursion and respiratory muscle weakness. In addition to involvement of costo-vertebral, costocartilage and costotransverse joints etc., direct pulmonary complication like fibrosis of more commonly apical segment may be the cause of restricted pulmonary function [30].
Movement of chest wall is a synchronising movement of the rib cage, sternum, vertebrae and related soft tissue. Change in any of its configuration influences the chest wall expansion and breathing [31,32]. During the spine extension, extensor group of muscles are most active, there is posterior rotation of vertebrae associated with the superior upward and posterior gliding of the costotransverse joints. There is anterior and upward expansion of sternum, where manubrium moves with 1st rib and body is flexible around the 2nd to 7th rib while taking deep inspiration. The opposite recoiling movement happens for the flexion with expiration [33].
Breathing exercises including trunk and extremity movements are termed as chest mobilization exercises which is designed to maintain or improve mobility of chest wall emphasizing the depth of inspiration and expiration [34].
In the present study there was increase in flexibility of spine measured by BASMI (tragus to wall distance, lumbar side-flexion, lumbar flexion and cervical rotation) and chest expansion in both conventional and experimental groups. Though evidence is limited in understanding the effect of flexibility exercises or breathing exercise alone on mobility of spine and chest in AS, there is an abundance of literature in the area of multi-modal exercise programs incorporating flexibility components to their program which are consistent with present study [13,35].
ROM in experimental group
In our experimental study, subjects with AS received soft tissue release of peri-scapular and paravertebral muscles with fascia in addition to conventional exercises.
In post-inflammatory phase, there is formation of new connective tissue fibers by fibroblast activity in a haphazard manner. In addition, the restrictive matrix has spider-web like tentacles attached to surrounding structures usually limit the mobility [36]. Immobility of soft tissue structures due to pain, spasm leads to ground substance dehydration. With loss of water the tissue become stiffer by formation of intermolecular crosslink fibers restricting inter-fiber mobility and extensibility [37,38].
Therapeutically soft tissue mobility can be restored by altering scar tissue matrix, stimulating the GAG synthesis, thereby prevent dehydration, breaking of restrictive intermolecular crosslink, gaining the mechanical and viscoelastic elongation of collagen tissue through creep and hysteresis phenomenon [39]. Utilising the described physiology, soft tissue release of periscapular and paravertebral muscles have an effect on improving flexibility of spine. In the present study there is no significant difference between the conventional and experimental groups (p=0.332) that may be due to small sample size and shorter duration of treatment period. But clinically the additional improvement achieved in our experimental study may be due this soft tissue release.
Lack of literature exists showing the effectiveness of soft tissue release alone or adjunct to the conventional exercise in patients with AS. However a case study was found to show the effect of a massage protocol that include Swedish strokes, stretching with myofascial release and trigger point therapy for 7 sessions (28 days) on a 47 year old woman had an improvement of stiffness in VAS to 1.2 from 3. Forward and lateral (left and right) Finger to floor distance had decreased to 4inch, 16.5inch and 16.5inch respectively whereas the initial values were 6inch, 21inch and 20.5inch respectively [40].
BASDAI score in conventional group
The inflammation that is due to activeness of disease leads to pain and tenderness of joints which interrelated with stiffness and reduced mobility. The flexibility exercise aims at improving and/or maintaining the spinal, articular mobility, fitness and functioning that reduces the pain and stiffness through the mechanoreceptors, which may be the cause reduction of BASDAI score.
Aerobic exercises reduce cardiopulmonary complication in chronic illness like AS improving maximal oxygen uptake (vo2 max) thereby enhancing functional capacity of a person [41]. Adaption and activation of an antioxidant activity induced by aerobics have an effect on the physiological changes on pathogenesis of AS [42]. Anti-inflammatory and analgesic effect due to production of catecholamine, cortisol, ᵦ-endorphin causing alternation in level of stress hormone and in the number and distribution of peripheral blood lymphocytes can be a reason of reduction of BASDAI score [43].
The exercise training has direct impact on inflammatory process and to modify the normal course of autoimmune diseases like AS by lowering the level of inflammatory cytokines that is associated with disease activity [44,45]. Though limited literature on role of exercise on inflammation in AS patient available, it was well proved in healthy subjects.
Pedersen et al. [46], referred skeletal muscle as ‘endocrine organ’ which secrete a number of cytokine (myokines) like interleukin 6(IL-6),followed by anti-inflammatory cytokines, such as interleukin 1 receptor antagonist (IL-1ra), interleukin-10 (IL-10) and tumor necrosis factor receptor (TNF-R)which all behave like hormone during muscle contraction, supressing the triggering of inflammation [46].
Lastly, in long term the adverse effects of pharmacological therapy like metabolic disturbances, low bone and lean mass, immunosuppression etc. were attenuated by combination of aerobic and strengthening exercise [41].
In the present study there was reduction of disease activity measured by BASDAI score in the conventional group. The result is consistent with following studies which used aerobic and flexibility exercises as an intervention in patients with AS.
Zsuzsanna et al., had a retrospective study which showed that after 3 months of exercise program consists of postural education, mobilisation of spine, pelvic and extremity exercises and stretching exercises there were decreased BASDAI and BASFI by 15-18% with improvement of flexibility [41].
BASDAI score in experimental group
The scoring of BASDAI items specially question 1 (fatigue) and 3 (peripheral joint pain and swelling) are influenced by coexistence of fibromyalgia [47]. Fatigue, depression, anxiety, sleep disorders are reported by patient with AS caused by FM triggering the pain [48]. Decrease in these symptoms associated with FM due to soft tissue release, may be one of the reason of reduction in BASDAI score.
STR encourages removal of cellular waste products as circulation increases, alleviating chemical pain. Mechanical pain can be modulated activating autonomic nervous system and pacinian receptors blocking nociceptive stimuli. Release of endogenous opiates may be another factor to decrease the symptoms interrupting the pain-spasm-pain cycle [49]. Very less no of literatures available on this topic in patients with AS as the latest evidence doesn’t include soft tissue release in effective treatment [50,51]. Though some studies include massage as adjunct treatment, studies are still in search to prove the effectiveness [52].
Romanowski et al. [40], conducted a randomized clinical pilot study to compare the effectiveness of two different types of massage in patients with AS [40]. Total 27 patients were allotted in both groups (one group treated with deep tissue massage other with therapeutic massage) were taken 10 session of 30 minutes for 2 weeks each. The DTM performed using trigger point therapy and oblique pressure with combination of lengthening stroke, cross-fiber stroke and stretch techniques. The result showed there was only statistically significant improvement in BASDAI and pain in the group taking DTM. Other mobility measures are not significantly increased.
A case study by Chunco R [53] showed the effects of massage on pain, stiffness and fatigue level associate with AS. After giving 7 sessions over 28 days pain, stiffness intensity and duration, forward and lateral flexion were measured again. There was greatest improvement of stiffness intensity i.e. 0.75 from 5, duration of stiffness 1.2 from 3.5 and pain 1 from 4, which all were the factors of BASDAI, though it was not mentioned [53].
The literature having improvement on disease activity on the conventional group (i.e. treated without any physical therapy) managed by pharmacological therapy are also available. The slight decrease in BASDAI score may be due to medication taken by all subjects that we did not conventional. Again the small duration period may not be able to show the added effects of soft tissue release with conventional exercise.
Physical Function (BASFI)
There was more reduction of BASFI score in the experimental group i.e. 0.91 (4.64 to 3.73) than in the conventional group i.e. 0.16 (4.69 to 4.53). In our study there is statistical significant in both groups from the baseline measurement (p=0.000) but the amount of improvement seen between two groups is not sufficient to show statistically significant (p=0.264).
BASFI score signifies how the disease affects the patient’s daily activities [54]. There is strong correlation exists between pain, stiffness, loss of mobility, fatigue, emotional or psychological or socioeconomic factors that influence the physical function impairment [55]. Decrease in stiffness and disease activity in both the groups may be the reason of decrease in BASFI score.
In our study BASFI is sensitive to the conventional exercise, which is also supported by studies by Altan et al. [16], Hsieh LF et al. [56], Günay et al. [57].
A comparison study between group based exercise and home based exercise in patient with AS showed the influence of conventional exercise on Bath indices like BASFI. Two groups (supervised and home based) were taken the exercise programme of respiratory exercise, stretching, mobility and strengthening exercise for upper limb ,lower limb and back 45 min per day, 3days a week for 6 weeks. In the result there were no statistical significant of BASFI within as well between groups which may be due to low scoring i.e. pre mean (SD) 2.62 (2.15) and 1.76 (1.67) in both groups [15].
A literature search revealed studies having multimodal exercise program including some from of aerobic exercise had increased aerobic capacity, improved physical function, decrease fatigue and pain including spinal flexibility [10,12]. Our study had 3% reduction in BASFI score in conventional group and 19% in experimental group which is similar in Analay et al. [34] study where the reduction of BASFI score was 23% [34]. The studies with home based exercise had reduction of BASFI score found 46% who have taken the duration of 8 weeks [10].
Soft tissue mobilisation followed by motor exercises in patient with ankylosing spondylitis is recommended as there is subsequent benefit. It stretches the shorten muscle structures, reduces the increased muscle tone, relieves the pain thereby improved motivation and physical activation like effects of massage [58].
Conclusion
The result of the study suggests soft tissue mobilisation is effective to improve spinal flexibility, chest expansion as an adjunctive therapy to the conventional exercise protocol in patient with Ankylosing spondylitis. There is also reduction of disease activity and improvement in functional status following 4 weeks of intervention.
References
- Russel AS. Ankylosing spondylitis: history. In: Klippel JH, Dieppe PA, eds. Rheumatology. St Louis: Mosby. Section 6. 1994.
- Dougados M, Gueguen A, Nakache JP, Nguyen M, Amor B. Evaluation of a functional index for patients with ankylosing spondylitis. J Rheumatol. 1990; 17: 1254-1255. Ref.: https://goo.gl/jijT5k
- Ward MM. Quality of life in patient with ankylosing spondylitis. Rheum Dis Clin North Am. 1998; 4: 815-827. Ref.: https://goo.gl/ugoLUL
- Ruof J, Stucki G. Comparison of the Dougados Functional Index and the Bath Ankylosing Spondylitis Functional Index. A literature review. J Rheumatol. 1999; 4: 955-960. Ref.: https://goo.gl/pF6zRp
- Dean LE, Jones GT, MacDonald AG, Downham C, Sturrock RD, Macfarlane GJ. Global Prevalence of Ankylosing Spondylitis. Rheumatology. 2014; 4: 650-657. Ref.: https://goo.gl/y69jHU
- Prakash S, Mehra NK, Bhargava S, Vaidya MC, Malaviya AN. Ankylosing Spondylitis in North India: A Clinical and Immunogenetic Study. Ann Rheum Dis. 1984; 3: 381-385. Ref.: https://goo.gl/GwHUuZ
- Van der Heijde D, Ramiro S, Landewé R, Baraliakos X, Van den Bosch F, et al. 2016 Update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis. 2016; 6: 978-991. Ref.: https://goo.gl/QkdJ3M
- Ward MM, Deodhar A, Akl EA, Lui A, Ermann J, et al. American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network 2015 Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2016; 2: 282-298. Ref.: https://goo.gl/rB2ErW
- Yigit S, Sahin Z, Demir SE, Aytac DH. Home-based exercise therapy in ankylosing spondylitis: short-term prospective study in patients receiving tumor necrosis factor alpha inhibitors. Rheumatol Int. 2013; 1: 71-77. Ref.: https://goo.gl/UiHnop
- Kjeken I, Bø I, Rønningen A, Spada C, Mowinckel P, et al. A three-week multidisciplinary in-patient rehabilitation programme had positive long-term effects in patients with ankylosing spondylitis: randomized controlled trial. J Rehabil Med. 2013; 3: 260-267. Ref.: https://goo.gl/MQpzxX
- Ozgocmen S, Akgul O, Altay Z, Altindag O, Baysal O, et al. Expert Opinion and Key Recommendations for the Physical Therapy and Rehabilitation of Patients with Ankylosing Spondylitis. Int J Rheum Dis. 2012; 3: 229-238. Ref.: https://goo.gl/DLptRj
- Masiero S, Bonaldo L, Pigatto M, Lo Nigro A, Ramonda R, et al. Rehabilitation treatment in patients with ankylosing spondylitis stabilized with tumor necrosis factor inhibitor therapy: a randomized controlled trial. J Rheumatol. 2011; 38: 1335-1342. Ref.: https://goo.gl/n1aBFP
- Ince G, Sarpel T, Durgun B, Erdogan S. Effects of a multimodal exercise program for people with ankylosing spondylitis. Phys Ther. 2006; 86: 924-935. Ref.: https://goo.gl/fE7yMZ
- So MW, Heo HM, Koo BS, Kim YG, Lee CK, et al. Efficacy of incentive spirometer exercise on pulmonary functions of patients with ankylosing spondylitis stabilized by tumor necrosis factor inhibitor therapy. J Rheumatol. 2012; 39: 1854-1858. Ref.: https://goo.gl/ZtC9eG
- Karapolat H, Eyigor S, Zoghi M, Akkoc Y, Kirazli Y, et al. Are swimming or aerobic exercise better than conventional exercise in ankylosing spondylitis patients? A randomized controlled study. Eur J Phys Rehabil Med.2009; 4: 449-457. Ref.: https://goo.gl/HzDaPT
- Altan L, Korkmaz N, Dizdar M, Yurtkuran M. Effect of Pilates Training on People with Ankylosing Spondylitis. Rheumatol Int. 2012; 7: 2093-2099. Ref.: https://goo.gl/VCfvjN
- Fábio J, Oliveira HA, De Souza MC, Cruz VDG, Natour J. Effects of Aerobic Training in Patients with Ankylosing Spondylitis. J Rheumatol. 2015; 12: 2347-2353. Ref.: https://goo.gl/LJaHcf
- Silva EM, Andrade SC, Vilar MJ. Evaluation of the effects of Global Postural Reeducation in patients with ankylosing spondylitis. Rheumatol Int. 2012; 7: 2155-2163. Ref.: https://goo.gl/4dqhVW
- Altan L, Yusuf S, İlker E. Can Bath Ankylosing Spondylitis Disease Activity Index be Affected by Accompanying Fibromyalgia or Depression?. Arch Rheumatol. 2015; 1: 34-39. Ref.: https://goo.gl/fFC2qu
- Bechterew M, Falkenbach A.Beratung, Betreuung, Behandlung. Wien, New York: Springer. 2005.
- Jones SD, Steiner A, Garrett SL, Calin A. The Bath Ankylosing Spondylitis Patient Global Score (BAS-G). Br J Rheumatol. 1996; 1: 66-71. Ref.: https://goo.gl/qvgZMJ
- Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, et al. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994; 12: 2286-2291. Ref.: https://goo.gl/BM5NUu
- Ruof J, Stucki G. Comparison of the Dougados Functional Index and the Bath Ankylosing Spondylitis Functional Index. A literature review. J Rheumatol. 1999; 26: 955-960. Ref.: https://goo.gl/NjtLdA
- Page P. Current concepts in muscle stretching for exercise and rehabilitation. Int J Sports Phys Ther. 2012; 1: 109-119. Ref.: https://goo.gl/4w9sHV
- Riley DA, Van Dyke JM. The effects of active and passive stretching on muscle length. Phys Med Rehabil Clin N Am. 2012; 1: 51-57. Ref.: https://goo.gl/wsBQXL
- Bulstrode SJ, Barefoot J, Harrison RA, Clarke AK. The role of passive stretching in the treatment of ankylosing spondylitis. Br J Rheumatol. 1987; 1: 40-42. Ref.: https://goo.gl/N5J7VH
- McCarthy D, Dale MM. The leucocytosis of exercise: A review and model. Sports Med. 1988; 6: 333-336. Ref.: https://goo.gl/Fq5NSS
- Bockenhauer SE, Chen H, Julliard KN, Weedon J. Measuring thoracic excursion: reliability of the cloth tape measure technique. J Am Osteopath Assoc. 2007; 5: 191-196. Ref.: https://goo.gl/AJx7qD
- Sharma J, Senjyu H, William L, White C. Intra-Tester and Inter-Tester Reliability of Chest Expansion Measurement in Clients with Ankylosing Spondylitis and Healthy Individuals. J Jpn Phys Ther Assoc. 2004; 1: 23-28. Ref.: https://goo.gl/xxJCGm
- Elliott CG, Hill TR, Adams TE, Crapo RO, Nietrzeba RM, et al. Exercise Performance of Subjects with Ankylosing Spondylitis and Limited Chest Expansion. Bull Eur Physiopathol Respir. 1985. 4: 363-368. Ref.: https://goo.gl/JPpqgZ
- Bates B. A guide to physical examination and history taking. 4th edition. Lippincott. Philadelphia. 1987.
- Hammon L. Review of respiratory anatomy, In: Chest physical therapy and pulmonary rehabilitation. Frownfelter, D.L (Ed), Year Book Medical Publishers. 1978; 3-18.
- Neumann DA. Kinesiology of the musculoskeletal system, In: Foundations for physical rehabilitation. Mosby. 2002; 288-300.
- Analay Y, Ozcan E, Karan A, Diracoglu D, Aydin R. The effectiveness of intensive group exercise on patients with ankylosing spondylitis. Clin Rehabil. 2003; 6: 631-636. Ref.: https://goo.gl/kUiBm8
- Pooja G, Riddhi S. Response of Ankylosing Spondilitis to Physiotherapy: A Case Report. JEPR. 2017; 1: 34-36.
- Cyriax J. Textbook of orthopaedic medicine: diagnosis of soft tissue lesions. 8th edition. Baltimore. Williams & Wilkins. 1984.
- Cummings GS, Crutchfield CA, Barnes MR. Orthopedic physical therapy. Vol 1. Soft tissue changes in contractures. Atlanta. Strokesville. 1983.
- Peacock E, VanWinkle W. Wound repair. 2nd edition. Philadelphia. WB Saunders. 1976.
- Van der Muelen JC. Present state of knowledge on processes of healing in collagen structures. Int J Sports Med. 1982; 3: 4-8. Ref.: https://goo.gl/j7cqUs
- Romanowski MW, Špiritović M, Rutkowski R, Dudek A, Samborski W, et al. Comparison of Deep Tissue Massage and Therapeutic Massage for Lower Back Pain, Disease Activity, and Functional Capacity of Ankylosing Spondylitis Patients: A Randomized Clinical Pilot Study. Evid Based Complement Alternat Med. 2017. Ref.: https://goo.gl/mRHQoP
- Gyurcsik ZN, András A, Bodnár N, Szekanecz Z, Szántó S. Improvement in pain intensity, spine stiffness, and mobility during a controlled individualized physiotherapy program in ankylosing spondylitis. Rheumatol Int. 2012; 12: 3931-3936. Ref.: https://goo.gl/1yuLKa
- Lazarevic G, Antic S, Cvetkovic T, VlahovicP, Tasic I, et al. A physical activity programme and its effects on insulin resistance and oxidative defense in obese male patients with type 2 diabetes mellitus. Diabetes Metab. 2006; 6: 583-590. Ref.: https://goo.gl/Qxp6P3
- Karakoc M, Altindag O, Keles H, Soran N, Selek S. Serum oxidative-antioxidative status in patients with ankylosing spondilitis. Rheumatol Int. 2007; 27: 1131-1134. Ref.: https://goo.gl/QbPE94
- Campbell KS, Lakie M. A cross-bridge mechanism can explain the thixotropic short-range elastic component of relaxed frog skeletal muscle. J Physiol. 1998; 3: 941-962. Ref.: https://goo.gl/VE5p93
- Huxley HE, Stewart A, Sosa H, Irving T. X-Ray diffraction measurements of the extensibility of actin and myosin filaments in contracting muscle. Biophys J. 1994; 6: 2411-2421. Ref.: https://goo.gl/gpTDa5
- Petersen AM, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol. 2005; 4: 1154-1162. Ref.: https://goo.gl/RZs8rW
- Aloush V, Ablin J, Reitblat T, Caspi D, Elkayam O. Fibromyalgia in women with ankylosing spondylitis. Rheumatol Intern. 2007; 9: 865-868. Ref.: https://goo.gl/tvbCww
- Dernis-Labous E, Messow M, Dougados M. Assessment of fatigue in the management of patients with ankylosing spondylitis. Rheumatology. 2003; 12: 1523-1528. Ref.: https://goo.gl/uekr8E
- Anderson E, Shivakumar G. Effects of Exercise and Physical Activity on Anxiety. Front Psychiatry. 2013; 4: 27. Ref.: https://goo.gl/FL4Pwx
- Braun JR, Berg V, Baraliakos X, Boehm H, Burgos-Vargas R, et al. 2010 update of the ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis. 2011; 6: 896-904. Ref.: https://goo.gl/ZHVdBn
- Van den berg R, Baraliakos X, Braun J, Van der heijde D. First update of the current evidence for the management of ankylosing spondylitis with non-pharmacological treatment and non-biologic drugs: a systematic literature review for the ASAS/EULAR management recommendations in ankylosing spondylitis. Rheumatology. 2012; 8: 1388-1396. Ref.: https://goo.gl/CtaHQb
- Passalent LA. Physiotherapy for ankylosing spondylitis: evidence and application. Curr Opin Rheumatol. 2011; 2: 142-147. Ref.: https://goo.gl/CU48Xq
- Chunco R. The Effects of Massage on Pain, Stiffness, and Fatigue Levels Associated with Ankylosing Spondylitis: A Case Study. Int J Ther Massage Bodywork. 2011; 1: 12-17. Ref.: https://goo.gl/4jPa2d
- Calin A, Garrett S, Whitelock H, Kennedy LG, O'Hea J, et al. A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol. 1994; 12: 2281-2285. Ref.: https://goo.gl/AQFHmr
- Sivas F, Mermerci BB, Inal EE, Bodur H. The relationship between enthesitis indices and disease activity parameters in patients with ankylosing spondylitis. Clin Rheumatol. 2009; 28: 259-264. Ref.: https://goo.gl/tuRJnE
- Hsieh LF, Chuang CC, Tseng CS, Wei JC, Hsu WC, et al. Combined home exercise is more effective than range-of-motion home exercise in patients with ankylosing spondylitis: a randomized controlled trial. Biomed Res Int. 2014. Ref.: https://goo.gl/w7pidZ
- Brown MA. Genetics of ankylosing spondylitis. Curr Opi Rheumatol. 2010; 2: 126-132. Ref.: https://goo.gl/xcAMzc
- Falkenbach A. Morbus Bechterew-Beratung, Betreuung, Behandlung.Wien, New York: Springer Wien-NewYork. 2005; 7: 501-505. Ref.: https://goo.gl/AsnnuV