Abstract
Review Article
Enhancing Physiotherapy Outcomes with Photobiomodulation: A Comprehensive Review
Nivaldo Antonio Parizotto* and Cleber Ferraresi
Published: 23 July, 2024 | Volume 8 - Issue 2 | Pages: 031-038
Physiotherapy treatments employ complex approaches tailored to the patient’s diagnosis. Exercise is the primary strategy to enhance rehabilitation processes for most individuals. However, electrophysical agents, such as Photobiomodulation (PBM), that utilize specific wavelengths of light to penetrate tissues and stimulate cellular activity, can modulate various biological processes and may improve physiotherapy outcomes. This non-invasive treatment can reduce pain and inflammation, promote tissue repair, and accelerate tissue healing. Currently, PBM has numerous applications, including pain and inflammation treatment, wound healing (such as diabetic foot ulcers, pressure ulcers, post-surgery wounds, and skin grafts in burn injuries), and the management of musculoskeletal disorders (such as arthritis, tendinopathies, muscle injuries, and spinal disorders). It is also utilized to improve muscle performance and recovery in rehabilitation and sports. Additionally, transcranial PBM has shown promise in enhancing neurorehabilitative processes by facilitating the recovery of cognitive and motor functions in various types of lesions. The safety and efficacy of this treatment allow it to be incorporated alongside regular exercises and manual therapies as an adjunctive treatment, potentially enhancing outcomes in different areas of rehabilitation.
Read Full Article HTML DOI: 10.29328/journal.jnpr.1001061 Cite this Article Read Full Article PDF
References
- Hamblin MR. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017;4(3):337-361. Available from: https://doi.org/10.3934/biophy.2017.3.337.
- Alqualo-Costa R, Rampazo EP, Thome GR, Perracini MR, Liebano RE. Interferential current and photobiomodulation in knee osteoarthritis: A randomized, placebo-controlled, double-blind clinical trial. Clin Rehabil. 2021;35(10):1413-1427. Available from: https://doi.org/10.1177/02692155211012004.
- Pigatto GR. Involvement of the descending endogenous pain modulation system in antinociceptive control by light-emitting diode therapy. Doctorate Thesis – Post Graduation Program in Biotechnology in Regenerative Medicine and Medical Chemistry – University of Araraquara, Brazil; 2020.
- Pigatto GR, Silva CS, Parizotto NA. Photobiomodulation therapy reduces acute pain and inflammation in mice. J Photochem Photobiol B. 2019;196:111513. Available from: https://doi.org/10.1016/j.jphotobiol.2019.111513.
- Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. Lancet. 2009;374(9705):1897-1908. Available from: https://doi.org/10.1016/s0140-6736(09)61522-1.
- Enwemeka CS, Parker JC, Dowdy DS, Harkness EE, Sanford LE, Woodruff LD. The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg. 2004;22(4):323-329. Available from: https://doi.org/10.1089/pho.2004.22.323.
- Yamany MS, El-Sayed WF. Effect of low-level laser therapy on neurovascular function of diabetic peripheral neuropathy. J Adv Res. 2013;4(6):459-466.
- Minatel DG, Frade MAC, França CM, Enwemeka CS. Phototherapy promotes healing of chronic diabetic leg ulcers that failed to respond to other therapies. Lasers Surg Med. 2019;41(6):433-441. Available from: https://doi.org/10.1002/lsm.20789.
- Karimpour S, Amirmotamed MH, Rashno F, Tahmasebinia F, Keramatinia A, Fathabadi FF, et al. Unveiling Therapeutic Potential: A Systematic Review of Photobiomodulation Therapy and Biological Dressings for Diabetic Foot Ulcers. J Lasers Med Sci. 2023;14. Available from: https://doi.org/10.34172/jlms.2023.49.
- Tchanque-Fossuo CN, Ho D, Dahle SE, Koo E, Li CS, Isseroff RR, et al. A systematic review of low-level light therapy for treatment of diabetic foot ulcer. Wound Repair Regen. 2016;24(2):418-426. Available from: https://doi.org/10.1111/wrr.12399.
- Santos CM dos, Rocha RB, Hazime FA, Cardoso VS. A Systematic Review and Meta-Analysis of the Effects of Low-Level Laser Therapy in the Treatment of Diabetic Foot Ulcers. Int J Low Extrem Wounds. 2021;20(3):198-207. Available from: https://doi.org/10.1177/1534734620914439.
- Wang HT, Yuan JQ, Zhang B, Dong ML, Mao C, Hu D. Phototherapy for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev. 2017;6. Available from: https://doi.org/10.1002/14651858.cd011979.pub2.
- Huang J, Chen J, Xiong S, Huang J, Liu Z. The effect of low-level laser therapy on diabetic foot ulcers: A meta-analysis of randomized controlled trials. Int Wound J. 2021;18(6):763-776. Available from: https://doi.org/10.1111/iwj.13577.
- Meyer PF, Maia RR, de Morais Carreiro E, da Silva RMV, Farias SLQ, Picariello F, et al. Analysis of modified ilib therapy in patients submitted to plastic surgery. Lasers Med Sci. 2024;39(1):110. Available from: https://link.springer.com/article/10.1007/s10103-024-04057-4.
- Kazemikhoo N, Vaghardoost R, Dahmardehei M, Mokmeli S, Momeni M, Nilforoushzadeh MA, et al. Healing process after skin gragft surgery in burned patients (A randomized Clinical Trial). J Lasers Med Sci. 2018;9(2):139-143. doi: 10.15171/jlms.2018.26. Available from: https://doi.org/10.15171%2Fjlms.2018.26.
- Taradaj J, Halski T, Kucharzewski M, Urbanek T, Halska U, Kucio C. Effect of Laser Irradiation at Different Wavelengths (940, 808, and 658 nm) on Pressure Ulcer Healing: Results from a Clinical Study. Evid Based Complement Alternat Med. 2013;2013:960240. doi: 10.1155/2013/960240. Available from: https://doi.org/10.1155/2013/960240.
- Huang YY, Chen AC, Carroll JD, Hamblin MR. Low-level laser therapy (LLLT) for treatment of osteoarthritis. Photomed Laser Surg. 2022;40(1):14-21.
- Ahmad MA, A Hamid MS, Yusof A. Effects of low-level and high-intensity laser therapy as adjunctive to rehabilitation exercise on pain, stiffness and function in knee osteoarthritis: a systematic review and meta-analysis. Physiotherapy. 2022;114:85-95. Available from: https://doi.org/10.1016/j.physio.2021.03.011
- Leal-Junior ECP, Vanin AA, Miranda EF, de Carvalho PD, Dal Corso S, Bjordal JM. Effect of photobiomodulation therapy (PBMT) on Achilles tendinitis in athletes: a randomized, double-blind, placebo-controlled trial. Lasers Med Sci. 2021;36(2):251-258.
- Ketz AK, Anders J, Orina J, Garner B, Hull M, Koreerat N, et al. Photobiomodulation Therapy Plus Usual Care Is Better than Usual Care Alone for Plantar Fasciitis: A Randomized Controlled Trial. Int J Sports Phys Ther. 2024;19(1):1438-1453. Available from: https://doi.org/10.26603/001c.90589.
- Dos Santos SA, Sampaio LM, Caires JR, Fernandes GHC, Marsico A, Serra AJ, et al. Parameters and Effects of Photobiomodulation in Plantar Fasciitis: A Meta-Analysis and Systematic Review. Photobiomodul Photomed Laser Surg. 2019;37(6):327-335. Available from: https://doi.org/10.1089/photob.2018.4588.
- Anders JJ, Moges H, Wu X. Photobiomodulation for the treatment of muscle injuries: a study on animal models. J Biophotonics. 2023;17(5)
- De Toni MM, Duarte RS, das Neves LMS, Diefenthaeler F, Fonseca MCR, Barbosa RI, et al. Physiotherapeutic approach in seamstresses with neck pain: A single-blind, randomized clinical trial. J Bodyw Mov Ther. 2022;31:90-96. doi: 10.1016/j.jbmt.2022.03.008. Available from: https://doi.org/10.1016/j.jbmt.2022.03.008.
- Navarro-Ledesma S, Carroll J, Burton P. Short-Term Effects of Whole-Body Photobiomodulation on Pain, Quality of Life and Psychological Factors in a Population Suffering from Fibromyalgia: A Triple-Blinded Randomised Clinical Trial. Pain Ther. 2023;12:225-239. Available from: https://doi.org/10.1007/s40122-022-00450-5.
- Hainline B, Derman W, Vernec A, Budgett R, Deie M, Dvorak J, et al. International Olympic Committee consensus statement on pain management in elite athletes. Br J Sports Med. 2017;51(17):1245-1258. Available from: https://doi.org/10.1136/bjsports-2017-097884.
- Craig JA, Barlas P, Baxter GD, Walsh DM, Allen JM. Delayed-onset muscle soreness: lack of effect of combined phototherapy/low-intensity laser therapy at low pulse repetition rates. J Clin Laser Med Surg. 1996;14(6):375-380. Available from: https://doi.org/10.1089/clm.1996.14.375.
- Craig JA, Barron J, Walsh DM, Baxter GD. Lack of effect of combined low intensity laser therapy/phototherapy (CLILT) on delayed onset muscle soreness in humans. Lasers Surg Med. 1999;24(3):223-230. Available from: https://doi.org/10.1002/(sici)1096-9101(1999)24:3%3C223::aid-lsm7%3E3.0.co;2-y.
- Vieira W, Goes R, Costa F, Parizotto N, Perez S, Baldissera V, et al. Enzymatic adaptation of LDH in rats subjected to aerobic training on a treadmill and low-intensity laser. Braz J Physiother. 2006;10:205-211. Available from: https://doi.org/10.1590/S1413-35552006000200011.
- Lopes-Martins RA, Marcos RL, Leonardo PS, Prianti AC, Muscara MN, Aimbire F, et al. Effect of low-level laser (Ga-Al-As 655 nm) on skeletal muscle fatigue induced by electrical stimulation in rats. J Appl Physiol (1985). 2006;101(1):283-288. Available from: https://doi.org/10.1152/japplphysiol.01318.2005 .
- Ferraresi C, Hamblin MR, Parizotto NA. Low-level laser (light) therapy (LLLT) on muscle tissue: performance, fatigue and repair benefited by the power of light. Photonics Lasers Med. 2012;1(4):267-286. Available from: https://doi.org/10.1515/plm-2012-0032.
- Ferraresi C, Huang YY, Hamblin MR. Photobiomodulation in human muscle tissue: an advantage in sports performance? J Biophotonics. 2016;9(11-12):1273-1299. Available from: https://doi.org/10.1002/jbio.201600176.
- Vanin AA, Verhagen E, Barboza SD, Costa LOP, Leal-Junior ECP. Photobiomodulation therapy for the improvement of muscular performance and reduction of muscular fatigue associated with exercise in healthy people: a systematic review and meta-analysis. Lasers Med Sci. 2018;33(1):181-214. Available from: https://doi.org/10.1007/s10103-017-2368-6.
- Gorgey AS, Wadee AN, Sobhi NN. The effect of low-level laser therapy on electrically induced muscle fatigue: a pilot study. Photomed Laser Surg. 2008;26(5):501-506. Available from: https://doi.org/10.1089/pho.2007.2161.
- Leal Junior EC, Lopes-Martins RA, Dalan F, Ferrari M, Sbabo FM, Generosi RA, et al. Effect of 655-nm low-level laser therapy on exercise-induced skeletal muscle fatigue in humans. Photomed Laser Surg. 2008;26(5):419-424. Available from: https://doi.org/10.1089/pho.2007.2160.
- Ferraresi C, de Brito Oliveira T, de Oliveira Zafalon L, de Menezes Reiff RB, Baldissera V, de Andrade Perez SE, et al. Effects of low level laser therapy (808 nm) on physical strength training in humans. Lasers Med Sci. 2011;26(3):349-358. Available from: https://doi.org/10.1007/s10103-010-0855-0.
- Ferraresi C, Dos Santos RV, Marques G, Zangrande M, Leonaldo R, Hamblin MR, et al. Light-emitting diode therapy (LEDT) before matches prevents increase in creatine kinase with a light dose response in volleyball players. Lasers Med Sci. 2015;30(4):1281-1287. Available from: https://doi.org/10.1007/s10103-015-1728-3.
- Ferraresi C, Bertucci D, Schiavinato J, Reiff R, Araujo A, Panepucci R, et al. Effects of Light-Emitting Diode Therapy on Muscle Hypertrophy, Gene Expression, Performance, Damage, and Delayed-Onset Muscle Soreness: Case-control Study with a Pair of Identical Twins. Am J Phys Med Rehabil. 2016;95(10):746-757. Available from: https://doi.org/10.1097/phm.0000000000000490.
- Baroni BM, Rodrigues R, Freire BB, Franke Rde A, Geremia JM, Vaz MA. Effect of low-level laser therapy on muscle adaptation to knee extensor eccentric training. Eur J Appl Physiol. 2015;115(3):639-647. Available from: https://doi.org/10.1007/s00421-014-3055-y.
- Ferraresi C, de Sousa MV, Huang YY, Bagnato VS, Parizotto NA, Hamblin MR. Time response of increases in ATP and muscle resistance to fatigue after low-level laser (light) therapy (LLLT) in mice. Lasers Med Sci. 2015;30(4):1259-1267. Available from: https://doi.org/10.1007/s10103-015-1723-8.
- Ferraresi C, Parizotto NA, Pires de Sousa MV, Kaippert B, Huang YY, et al. Light-emitting diode therapy in exercise-trained mice increases muscle performance, cytochrome c oxidase activity, ATP and cell proliferation. J Biophotonics. 2015;8(9):740-54. Available from: https://doi.org/10.1002/jbio.201400087
- González-Muñoz A, Cuevas-Cervera M, Pérez-Montilla JJ, Aguilar-Núñez D, Hamed-Hamed D, Aguilar-García M, et al. Efficacy of Photobiomodulation Therapy in the Treatment of Pain and Inflammation: A Literature Review. Healthcare. 2023;11(7):938. Available from: https://doi.org/10.3390/healthcare11070938.
- Salehpour F, Majdi A, Pazhuhi M, Ghasemi F, Khademi M, Pashazadeh F, et al. Transcranial Photobiomodulation Improves Cognitive Performance in Young Healthy Adults: A Systematic Review and Meta-Analysis. Photobiomodul Photomed Laser Surg. 2019;37(10):635-643. Available from: https://doi.org/10.1089/photob.2019.4673.
- Barrett DW, Gonzalez-Lima F. Transcranial infrared laser stimulation produces beneficial cognitive and emotional effects in humans. Neurosci Lett. 2018;665:36-40.
- Chao LL. Transcranial photobiomodulation improves cognitive performance and functional connectivity in older adults with mild cognitive impairment: a pilot study. J Alzheimers Dis. 2019;71(3):765-774.
- Cassano P, Petrie SR, Hamblin MR, Henderson TA, Iosifescu DV, Buchheit CL. Review of transcranial photobiomodulation for major depressive disorder: targeting brain metabolism, inflammation, oxidative stress, and neurogenesis. Photomed Laser Surg. 2019;37(10):617-625.
- Liu TC, Huang CM, Huang LT, Chen CH, Chen YC. Transcranial photobiomodulation for the treatment of generalized anxiety disorder: a pilot study. Photobiomodul Photomed Laser Surg. 2020;38(2):89-95.
- Naeser MA, Zafonte R, Krengel MH, Martin PI, Frazier J. Improved cognitive function after transcranial, light-emitting diode treatments in chronic, traumatic brain injury: two case reports. Photomed Laser Surg. 2020;38(3):170-179.
- Mitrofanis J, Jeffery G. Does photobiomodulation influence ageing? Aging (Albany NY). 2018;10(9):2224-2225. doi: 10.18632/aging.101556. Available from: https://doi.org/10.18632/aging.101556.
- Berman MH, Halper JP, Nichols TW, Gerber J, Sanner J. Photobiomodulation-induced changes in beta-amyloid levels in the brain of an Alzheimer's disease mouse model: a pilot study. Photobiomodul Photomed Laser Surg. 2018;36(11):584-590.
- El Khoury H, Mitrofanis J, Henderson LA. Exploring the effects of transcranial photobiomodulation in Parkinson's disease: a preliminary study. J Parkinsons Dis. 2019;9(3):503-510..
- Hennessy M, Hamblin MR. Photobiomodulation and the brain: a new paradigm. J Opt. 2017 Jan;19(1):013003. Available from: https://doi.org/10.1088/2040-8986/19/1/013003.
- Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514-530. Available from: https://doi.org/10.7326/m16-2367.
- Sobral AP, Sobral SS, Campos TM, Horliana AC, Fernandes KP, Bussadori SK, Motta LJ. Photobiomodulation and myofascial temporomandibular disorder: Systematic review and meta-analysis followed by cost-effectiveness analysis. J Clin Exp Dent. 2021;13(7). Available from: https://doi.org/10.4317/jced.58084.
- González-Muñoz A, Perez-Montilla JJ, Cuevas-Cervera M, Aguilar-García M, Aguilar-Nuñez D, Hamed-Hamed D, Pruimboom L, Navarro-Ledesma S. Effects of Photobiomodulation in Sports Performance: A Literature Review. Appl Sci. 2023;13:3147. Available from: https://doi.org/10.3390/app13053147.
- Ferraresi C, Kaippert B, Avci P, Huang YY, de Sousa MV, Bagnato VS, et al. Low-level laser (light) therapy increases mitochondrial membrane potential and ATP synthesis in C2C12 myotubes with a peak response at 3-6 h. Photochem Photobiol. 2015;91(2):411-416. Available from: https://doi.org/10.1111/php.12397.
- Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516-533. Available from: https://doi.org/10.1007/s10439-011-0454-7
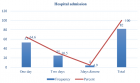
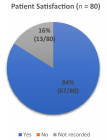
Figures:
Similar Articles
-
Postural Stability Induced by Supervised Physical Training may improve also Oxygen Cost of Exercise and Walking Capacity in Post-Menopause, Obese WomenFernanda Velluzzi,Massimiliano Pau,Andrea Loviselli,Raffaele Milia,Daniela Lai,Daniele Concu,Gianmarco Angius,Abdallah Raweh,Andrea Fois,Alberto Concu*. Postural Stability Induced by Supervised Physical Training may improve also Oxygen Cost of Exercise and Walking Capacity in Post-Menopause, Obese Women. . 2017 doi: 10.29328/journal.jnpr.1001001; 1: 001-011
-
Effects of Fast-Walking on Muscle Activation in Young Adults and Elderly PersonsCamila Fonseca de Oliveira*,Denise Paschoal Soares,Michel Christian Bertani,Leandro José Rodrigues Machado,João Paulo Vila-Boas. Effects of Fast-Walking on Muscle Activation in Young Adults and Elderly Persons. . 2017 doi: 10.29328/journal.jnpr.1001002; 1: 012-019
-
Pulsed Shortwave Diathermy and Joint Mobilizations Restore a Twice Fractured Elbow with Metal Implants to Full Range of MotionDavid O. Draper*,Emily Veazey. Pulsed Shortwave Diathermy and Joint Mobilizations Restore a Twice Fractured Elbow with Metal Implants to Full Range of Motion. . 2017 doi: 10.29328/journal.jnpr.1001003; 1: 020-026
-
Comparison of two types of strengthening exercises in upper limbs for improvement of wheelchair propulsion in paraplegicsAkanksha Satyavanshi,Monalisa Pattnaik,Patitapaban Mohanty*. Comparison of two types of strengthening exercises in upper limbs for improvement of wheelchair propulsion in paraplegics. . 2017 doi: 10.29328/journal.jnpr.1001004; 1: 027-033
-
Foot Arch Differences in Elderly People at Standing: Considering Gender and AgeMichel Bertani,Denise Soares,Everton Rocha,Leandro Machado. Foot Arch Differences in Elderly People at Standing: Considering Gender and Age. . 2017 doi: 10.29328/journal.jnpr.1001005; 1: 034-038
-
Achilles Tendon Injuries: Comparison of Different Conservative and Surgical Treatment and RehabilitationAlessandro Bistolfi,Jessica Zanovello, Elisa Lioce,Lorenzo Morino,Raul Cerlon,Alessandro Aprato*,Giuseppe Massazza. Achilles Tendon Injuries: Comparison of Different Conservative and Surgical Treatment and Rehabilitation. . 2017 doi: 10.29328/journal.jnpr.1001006; 1: 039-053
-
How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?Maurizio Falso*, Eleonora Cattaneo,Elisa Foglia,Marco Zucchini,Franco Zucchini. How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?. . 2017 doi: 10.29328/journal.jnpr.1001010; 1: 072-092
-
First Metatarsal Stress Fracture of a pre-adolescent female Irish dancer with Medial Plantar Foot Pain: A Case ReportDale Gerke,Jean-Michel Brismée*. First Metatarsal Stress Fracture of a pre-adolescent female Irish dancer with Medial Plantar Foot Pain: A Case Report. . 2017 doi: 10.29328/journal.jnpr.1001009; 1: 067-071
-
Factors affecting muscle strength in cancer patients receiving chemotherapyJiro Nakano*,Shun Ishii,Takuya Fukushima,Ayumi Natsuzako,Junya Sakamoto,Minoru Okita. Factors affecting muscle strength in cancer patients receiving chemotherapy. . 2017 doi: 10.29328/journal.jnpr.1001008; 1: 056-066
-
The effects of EMF (ELECTROMAGNETIC FIELDS) on the Bone and Cartilage TissueCemil Sert*. The effects of EMF (ELECTROMAGNETIC FIELDS) on the Bone and Cartilage Tissue. . 2017 doi: 10.29328/journal.jnpr.1001007; 1: 054-055
Recently Viewed
-
Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean sectionToon Wen Tang*,Phoon Wai Leng Jessie. Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean section. Clin J Obstet Gynecol. 2021: doi: 10.29328/journal.cjog.1001094; 4: 092-095
-
Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience ResearchAlex, Gideon S*,Olanrewaju Oluwaseun Oke,Joy Wilberforce Ekokojde,Tolulope Judah Gbayisomore,Martina C. Anene-Ogbe,Farounbi Glory,Joshua Ayodele Yusuf. Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience Research. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001102; 8: 106-114
-
Late discover of a traumatic cardiac injury: Case reportBenlafqih C,Bouhdadi H*,Bakkali A,Rhissassi J,Sayah R,Laaroussi M. Late discover of a traumatic cardiac injury: Case report. J Cardiol Cardiovasc Med. 2019: doi: 10.29328/journal.jccm.1001048; 4: 100-102
-
A two-phase sonographic study among women with infertility who first had normal sonographic findingsKalu Ochie*,Abraham John C. A two-phase sonographic study among women with infertility who first had normal sonographic findings. Clin J Obstet Gynecol. 2022: doi: 10.29328/journal.cjog.1001117; 5: 101-103
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001099; 8: 075-077
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."