Abstract
Research Article
TRIA-MF protocol as an innovative tool in the comprehensive treatment and outcome evaluation of lower limb amputees before and after prosthesis use
Maurizio Falso*, Silvia Zani, Eleonora Cattaneo, Marco Zucchini and Franco Zucchini
Published: 18 January, 2019 | Volume 3 - Issue 1 | Pages: 001-024
Background: A structured multidisciplinary team is very important during every phase of the amputation process and a good communicative team guarantees a greater tranquility for the patient, thanks to more homogenous information, that is already discussed between the clinicians.
Aim: The aim of this study was to define the efficacy and outcome value of an innovative procedure tool (TRIA-MF protocol) in the treatment of lower limb amputees before and after prosthesis use with the purpose to quantify the quality of the procedure and its economic impact on the clinical patients’ recovery.
Setting: A rehabilitation institute for the treatment of neurological and orthopaedic gait disorders.
Methods: 12 patients (4 women and 8 males) subjected to lower limb amputation and admitted according to the principles of inclusion criteria of the TRIA-MF protocol at the Rehabilitation Department of the Clinical Institute Città di Brescia were recruited in this study. All patients were included in an integrated and task-specific management protocol of the amputee, which allowed to follow the rehabilitation process from amputation to the final restoration, for a period of 6 months for each patient. Patients were evaluated 5 times during the study, collecting their degree of pain (VAS), their independence profile (Barthel Index) and the cirtometry of their amputation stump. Data on the duration of their admission to the rehabilitation unit, the inter-time between the amputation and acquisition of the temporary prosthesis, and between temporary prosthesis acquisition and the final prosthesis acquisition were also reported.
Results: Patients of our sample, at the end of their hospitalization, highlight a significant modification of the temporal data at 1 month and 6 months from their hospital discharge. A statistical significant increase of the Barthel Index value was observed in all patients recruited in this study proceeding from time T0 to time T4; in the same way, a statistical significant decrease of the VAS scale was observed in all patients recruited proceeding from time T0 to time T4; the cirtometry of the amputation stump (expressed in cm) showed a statistical significant decrease in all patients recruited proceeding from time T0 to time T4. We haven’t observed a statistical significant correlation between the duration of the rehabilitative hospitalization and our clinical data; no statistical significant correlation was observed between the amputation stump cirtometry time-related modification and our intertime data.
Conclusions: The protocol was found to be a clear and relevant tool with the definition of the operational profile for each single professional figure involved; it could also be considered as an optimal tool for coding the management and evaluation of the effectiveness of amputee treatment, with a related high reproducibility, sensitivity and specificity profile. In line with the literature, the TRIA-MF protocol has allowed us not to exceed a period of hospitalization in rehabilitation units of more than 23 days, thus showing that it is an excellent tool for optimizing the management costs of the amputee over time.
Read Full Article HTML DOI: 10.29328/journal.jnpr.1001024 Cite this Article Read Full Article PDF
References
- Ippolito E, Flaviani L, Belcaro G. Amputazione degli arti inferiori nelle arteriopatie periferiche. Edizioni Minerva Medica, 2005; Ref.: https://goo.gl/j1zT7d
- De Ciechi R. Ausili per persone adulte ed anziane amputate di arto inferiore. Corso di perfezionamento. Fondazione Don Carlo Gnocchi, 2009/2010. Ref.: https://goo.gl/nRLXoy
- Zaniolo O. Costi del diabete in Italia. Farmaeconomia e percorsi terapeutici, 2009. Ref.: https://goo.gl/ketA1M
- Geertzen J1, van der Linde H2, Rosenbrand K3, Conradi M4, Deckers J, et al. Dutch evidence-based guidelines for amputation and prosthetic of lower extremity: parts 2. Prosthet Orthot Int. 2015; 39: 361-371. Ref.: https://goo.gl/HSBRpk
- Conte MS. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) and the (hoped for) dawn of evidence-based treatment for advanced limb ischemia. J Vasc Surg. 2010; 51(5 Suppl): 69S-75S. Ref.: https://goo.gl/R4UUR8
- Klenow TD, Mengelkoch LJ, Stevens PM, Ràbago CA, Hill OT, et al. The role of exercise testing in predicting successful ambulation with a lower extremity prosthesis: a systematic literature review and clinical practice guideline. J Neuroeng Rehabil. 2018; 15(Suppl 1): 64. Ref.: https://goo.gl/Y3p5LC
- Sanders JE, Fatone S. Residual limb volume change: Systematic review of measurement and management. J Rehabil Res Dev. 2011; 48: 949–986. Ref.: https://goo.gl/SGGe3G
- Yahata T, Takeuchi A, Yoshida S, Tsuchiya H. Distinctive features of stump volume change in a fresh lower limb amputee with Parkes-Weber syndrome. BMJ Case Rep. 2014; 2014. pii: bcr2014206315. Ref.: https://goo.gl/fZ33fC
- Highsmith MJ, Kahle JT, Klenow TD, Andrews CR, Lewis KL, et al. interventions to Manage Residual Limb Ulceration due to Prosthetic use in Individuals with Lower Extremity Amputation: A Systematic Review of the Literature. Technol Innov. 2016; 18: 115-123. Ref.: https://goo.gl/dWXT4H
- Mendoza-Cruz F, Rodríguez-Reyes G, Galván Duque-Gastélum C, Alvarez-Camacho M. Comparative study of the volume difference vs. healthy limb, morphological and population description in transfemoral amputees. Rev Invest Clin. 2014; 66 Suppl 1: S85-93. Ref.: https://goo.gl/YW2Fti
- Liu J, Lu N, Lou VWQ. Care tasks in the stress process for family caregivers in urban China. Clinical Gerontology. 2017; 40: 428-434. Ref.: https://goo.gl/Wf5uZq
- Madsen UR, Hommel A, Bååth C, Berthelsen CB. Pendulating-A grounded theory explaining patients' behavior shortly after having a leg amputated due to vascular disease. Int J Qual Stud Health Well-being. 2016; 11: 32739. Ref.:
- Rotariu M, Filep R, Turnea M, Ilea M, Arotăriţei D, Popescu M. Analyse of socket-prosthesis-blunt complex for lower limb amputee using objective measure of patient's gait cycle. Rev Med Chir Soc Med Nat Iasi. 2015; 119: 281-286. https://goo.gl/SxRqrA
- Murray CD1, Simpson J, Eccles F, Forshaw MJ. Involvement in rehabilitative care and wellbeing for partners of people with an amputation. Psychol Health Med. 2015; 20: 71-76. Ref.: https://goo.gl/xJ3KKW
- Mckechnie PS,John A. Anxiety and depression following traumatic limb amputation: a systematic review. Injury. 2014; 45: 1859-1866. Ref.: https://goo.gl/BfCyJ2
- Horgan O,MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disabil Rehabil. 2004; 26: 837-850. Ref.: https://goo.gl/kwvjTB
- Augustin M, Baade K, Heyer K, Price PE, Herberger K, et al. Quality-of-life evaluation in chronic wounds: comparative analysis of three disease-specific questionnaires. Int Wound J. 2017; 14: 1299-1304. Ref.: https://goo.gl/kK7HRN
Figures:

Figure 1

Figure 2

Figure 3

Figure 4
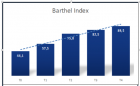
Figure 5
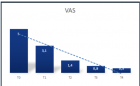
Figure 6
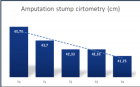
Figure 7

Figure 8

Figure 9

Figure 10
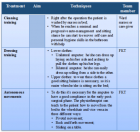
Figure 11
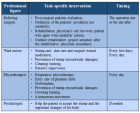
Figure 12

Figure 13
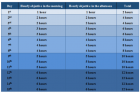
Figure 14

Figure 15

Figure 16

Figure 17
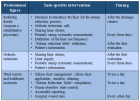
Figure 18
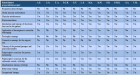
Figure 19
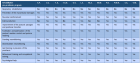
Figure 20
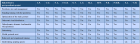
Figure 21

Figure 22
Similar Articles
-
Postural Stability Induced by Supervised Physical Training may improve also Oxygen Cost of Exercise and Walking Capacity in Post-Menopause, Obese WomenFernanda Velluzzi,Massimiliano Pau,Andrea Loviselli,Raffaele Milia,Daniela Lai,Daniele Concu,Gianmarco Angius,Abdallah Raweh,Andrea Fois,Alberto Concu*. Postural Stability Induced by Supervised Physical Training may improve also Oxygen Cost of Exercise and Walking Capacity in Post-Menopause, Obese Women. . 2017 doi: 10.29328/journal.jnpr.1001001; 1: 001-011
-
Effects of Fast-Walking on Muscle Activation in Young Adults and Elderly PersonsCamila Fonseca de Oliveira*,Denise Paschoal Soares,Michel Christian Bertani,Leandro José Rodrigues Machado,João Paulo Vila-Boas. Effects of Fast-Walking on Muscle Activation in Young Adults and Elderly Persons. . 2017 doi: 10.29328/journal.jnpr.1001002; 1: 012-019
-
Pulsed Shortwave Diathermy and Joint Mobilizations Restore a Twice Fractured Elbow with Metal Implants to Full Range of MotionDavid O. Draper*,Emily Veazey. Pulsed Shortwave Diathermy and Joint Mobilizations Restore a Twice Fractured Elbow with Metal Implants to Full Range of Motion. . 2017 doi: 10.29328/journal.jnpr.1001003; 1: 020-026
-
Comparison of two types of strengthening exercises in upper limbs for improvement of wheelchair propulsion in paraplegicsAkanksha Satyavanshi,Monalisa Pattnaik,Patitapaban Mohanty*. Comparison of two types of strengthening exercises in upper limbs for improvement of wheelchair propulsion in paraplegics. . 2017 doi: 10.29328/journal.jnpr.1001004; 1: 027-033
-
Foot Arch Differences in Elderly People at Standing: Considering Gender and AgeMichel Bertani,Denise Soares,Everton Rocha,Leandro Machado. Foot Arch Differences in Elderly People at Standing: Considering Gender and Age. . 2017 doi: 10.29328/journal.jnpr.1001005; 1: 034-038
-
Achilles Tendon Injuries: Comparison of Different Conservative and Surgical Treatment and RehabilitationAlessandro Bistolfi,Jessica Zanovello, Elisa Lioce,Lorenzo Morino,Raul Cerlon,Alessandro Aprato*,Giuseppe Massazza. Achilles Tendon Injuries: Comparison of Different Conservative and Surgical Treatment and Rehabilitation. . 2017 doi: 10.29328/journal.jnpr.1001006; 1: 039-053
-
How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?Maurizio Falso*, Eleonora Cattaneo,Elisa Foglia,Marco Zucchini,Franco Zucchini. How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?. . 2017 doi: 10.29328/journal.jnpr.1001010; 1: 072-092
-
First Metatarsal Stress Fracture of a pre-adolescent female Irish dancer with Medial Plantar Foot Pain: A Case ReportDale Gerke,Jean-Michel Brismée*. First Metatarsal Stress Fracture of a pre-adolescent female Irish dancer with Medial Plantar Foot Pain: A Case Report. . 2017 doi: 10.29328/journal.jnpr.1001009; 1: 067-071
-
Factors affecting muscle strength in cancer patients receiving chemotherapyJiro Nakano*,Shun Ishii,Takuya Fukushima,Ayumi Natsuzako,Junya Sakamoto,Minoru Okita. Factors affecting muscle strength in cancer patients receiving chemotherapy. . 2017 doi: 10.29328/journal.jnpr.1001008; 1: 056-066
-
The effects of EMF (ELECTROMAGNETIC FIELDS) on the Bone and Cartilage TissueCemil Sert*. The effects of EMF (ELECTROMAGNETIC FIELDS) on the Bone and Cartilage Tissue. . 2017 doi: 10.29328/journal.jnpr.1001007; 1: 054-055
Recently Viewed
-
Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean sectionToon Wen Tang*,Phoon Wai Leng Jessie. Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean section. Clin J Obstet Gynecol. 2021: doi: 10.29328/journal.cjog.1001094; 4: 092-095
-
Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience ResearchAlex, Gideon S*,Olanrewaju Oluwaseun Oke,Joy Wilberforce Ekokojde,Tolulope Judah Gbayisomore,Martina C. Anene-Ogbe,Farounbi Glory,Joshua Ayodele Yusuf. Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience Research. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001102; 8: 106-114
-
Late discover of a traumatic cardiac injury: Case reportBenlafqih C,Bouhdadi H*,Bakkali A,Rhissassi J,Sayah R,Laaroussi M. Late discover of a traumatic cardiac injury: Case report. J Cardiol Cardiovasc Med. 2019: doi: 10.29328/journal.jccm.1001048; 4: 100-102
-
A two-phase sonographic study among women with infertility who first had normal sonographic findingsKalu Ochie*,Abraham John C. A two-phase sonographic study among women with infertility who first had normal sonographic findings. Clin J Obstet Gynecol. 2022: doi: 10.29328/journal.cjog.1001117; 5: 101-103
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001099; 8: 075-077
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."