Abstract
Research Article
Rehabilitation of proximal humerus fractures: An environmental scan of Canadian physiotherapy practice patterns
Lowell L Kwan and Norma J MacIntyre*
Published: 20 September, 2017 | Volume 1 - Issue 3 | Pages: 104-119
Background: Proximal humerus fractures (PHFs) are common injuries particularly in older adults. Evidence-based protocols for PHF rehabilitation are lacking and physiotherapists use a variety of interventions.
Purpose: To determine practice patterns and perceptions of physiotherapists who treat adults with PHF in Ontario, Canada.
Method: A paper and pencil survey asking about respondent demographics and management of Neer Group 1 (minimally/nondisplaced) and complex (displaced 3- and 4-part) PHF was mailed to 875 randomly selected physiotherapists who were registered with the College of Physiotherapists of Ontario in 2013/2014 and working in practice areas likely to be accessed by adults with PHF.
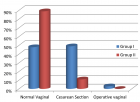
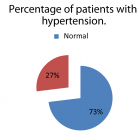
Results: The response rate was low (10%); 83 physiotherapists completed the survey - 80% had experience managing PHF. Respondents treated 1-5 individuals with PHF annually; more treated Neer Group 1 PHF (89%) than complex PHF (68%). Most individuals with PHF were older than 60 years (64%), female (76%) and accessed physiotherapy through a doctor’s referral (91%) more than 1 month post injury (33%).
Main findings: Physiotherapists manage PHF using multi-component interventions and a minimum of 76% include the following elements: education and progression of passive, active assisted, active range of motion exercises and muscle retraining to build coordination and strength. Use of other elements was variable. The main factors influencing the treatment plan were the ability of the individual with PHF to comply, bone quality, and fracture type. Most respondents were unsure that there is sufficient PHF rehabilitation literature to guide treatment.
Conclusions:This environmental scan is the first North American study to document practice patterns and attitudes of physiotherapists providing PHF rehabilitation. Elements used by physiotherapists in Ontario treating small numbers of individuals with Neer Group 1 or complex PHFs each year align well with the limited PHF rehabilitation literature available.
Potential implications:Multi-disciplinary collaborations to design and conduct large, high quality, multi-centre prognostic studies and RCTs that evaluate the effectiveness of key aspects of non-surgical PHF rehabilitation in various patient groups are needed. Meanwhile, consensus guidelines should be developed in the context of region-specific physiotherapy service models to inform best practice in PHF rehabilitation management.
Read Full Article HTML DOI: 10.29328/journal.jnpr.1001013 Cite this Article Read Full Article PDF
Keywords:
Shoulder fractures; Physical therapy; Rehabilitation; Questionnaire
References
- Karl JW, Olson PR, Rosenwasser MP. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma. 2015; 29: 242-244. Ref.: https://goo.gl/MwrqCa
- Launonen AP, Lepola V, Saranko A, Flinkkila T, Laitinene M, et al. Epidemiology of proximal humerus fractures. Arch Osteoporos. 2015; 10: 209. Ref.: https://goo.gl/u52orr
- Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humerus fractures. Acta Orthop Scand. 2001; 72: 365-371. Ref.: https://goo.gl/EoMbNu
- Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011; 20: 747-755. Ref.: https://goo.gl/CfF74Q
- Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011; 20: 1025-1033. Ref.: https://goo.gl/pKvbjJ
- Handoll HHG, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2015. Ref.: https://goo.gl/qZMyUr
- MacIntyre NJ, Kwan LL, Johal H, Lefaivre KA, Sprague S, et al. Rehabilitation of proximal humerus fractures: a scoping review. SM J Trauma Care. 2017; 1:1001. Ref.: https://goo.gl/QGzh33
- Handoll HHG, Goodchild L, Brealey SD, Hanchard NCA, Jefferson L, et al. Developing, delivering and documenting rehabilitation in a multi-centre randomised controlled surgical trial: experiences from the PROFHER trial. Bone Joint Res. 2014; 3: 335-340. Ref.: https://goo.gl/SDs45Y
- Hodgson S. Proximal humerus fracture rehabilitation. Clin Orthop Relat Res. 2006; 442: 131-138. Ref.: https://goo.gl/EyfTyE
- Tousignant M, Giguere AM, Morin M, Pelletier J, Sheehy A, et al. In-home telerehabilitation for proximal humerus fractures: a pilot study. Int J Telerehabil. 2015; 6: 31-37. Ref.: https://goo.gl/TXvjn7
- Shih T, Xitao F. Comparing response rates from web and mail surveys: A meta-analysis. Field Methods. 2008; 20: 249-271. Ref.: https://goo.gl/4VudfG
- Guy P, Slobogean GP, McCormack RG. Treatment preferences for displaced three- and four-part proximal humerus fractures. J Orthop Trauma. 2010; 24: 250-254. Ref.: https://goo.gl/pgpeZx
- Canadian Institute for Health Information. Physiotherapists in Canada, 2010 National and Jurisdictional Highlights and Profiles. 2017.
- Arias-Buria JL,Valero-Alcaide R, Cleland JA, Salom-Moreno J, OrtegaSantiago R, et al. Inclusion of trigger point dry needling in a multimodal physiotherapy program for postoperative shoulder pain: a randomized clinical trial. J Manipulative Physiol Ther. 2015; 38: 179-187. Ref.: https://goo.gl/eVWzXN
- Rubinik P, Calmels P, Edouard P, Genty M, Yelnik AP. Care pathways in physical and rehabilitation medicine (PRM): the patient after proximal humeral fracture and shoulder hemi-arthroplasty. Ann Phys Rehabil Med. 2012; 55: 557-564. Ref.: https://goo.gl/NnvCwN
- Singleton E, Turner R, Gulotta L. Rehabilitation after proximal humerus fracture. Tech Shoulder Elb Surg. 2014; 15: 46-50. Ref.: https://goo.gl/EUDMo3
- Lundberg BJ, Svenungson-Hartwig E, Wikmark R. Independent exercises versus physiotherapy in nondisplaced proximal humeral fractures. Scand J Rehabil Med. 1979; 11: 133-136. Ref.: https://goo.gl/RZ1AKT
- Bertoft ES, Lundh I, Ringqvist I. Physiotherapy after fracture of the proximal end of the humerus. Comparison between two methods. Scand J Rehabil Med. 1984; 16: 11-16. Ref.: https://goo.gl/1ypkhG
Figures:
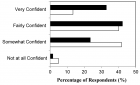
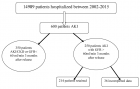
Figure 1

Figure 2

Figure 3
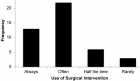
Figure 4
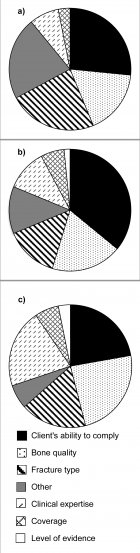
Figure 5
Similar Articles
-
Achilles Tendon Injuries: Comparison of Different Conservative and Surgical Treatment and RehabilitationAlessandro Bistolfi,Jessica Zanovello, Elisa Lioce,Lorenzo Morino,Raul Cerlon,Alessandro Aprato*,Giuseppe Massazza. Achilles Tendon Injuries: Comparison of Different Conservative and Surgical Treatment and Rehabilitation. . 2017 doi: 10.29328/journal.jnpr.1001006; 1: 039-053
-
Determining the use and value of social support in Telerehabiliation Interventions for individuals with Multiple Sclerosis: A narrative synthesis reviewLucinda Pidgeon,Trudy Pelton*,Andrew Soundy. Determining the use and value of social support in Telerehabiliation Interventions for individuals with Multiple Sclerosis: A narrative synthesis review. . 2017 doi: 10.29328/journal.jnpr.1001014; 1: 120-136
-
Rehabilitation of proximal humerus fractures: An environmental scan of Canadian physiotherapy practice patternsLowell L Kwan,Norma J MacIntyre*. Rehabilitation of proximal humerus fractures: An environmental scan of Canadian physiotherapy practice patterns. . 2017 doi: 10.29328/journal.jnpr.1001013; 1: 104-119
-
Frequency specific microcurrent resolves chronic pain and adhesions after ulnar transposition surgeryJodie Adams*,Carolyn McMakin. Frequency specific microcurrent resolves chronic pain and adhesions after ulnar transposition surgery. . 2017 doi: 10.29328/journal.jnpr.1001012; 1: 099-103
-
The short and mid-term effects of Mulligan concept in patients with chronic mechanical neck painKonstantinos Zemadanis*. The short and mid-term effects of Mulligan concept in patients with chronic mechanical neck pain. . 2018 doi: 10.29328/journal.jnpr.1001018; 2: 022-035
-
Physical Therapy for Transverse Myelitis: A Case ReportAllison Buchanan,Kelli J Wilkerson,Han-Hung Huang*. Physical Therapy for Transverse Myelitis: A Case Report. . 2018 doi: 10.29328/journal.jnpr.1001017; 2: 015-021
-
Perceptive and Rehabilitative Muscle Recruitment Facilitation Secondary to the use of a Dynamic and Asymmetric Spine Brace in the treatment of Adolescent Idiopathic Scoliosis (AIS)Maurizio Falso*, Laura Forti,Silvia Iezzi,Gloria Cottali,Eleonora Cattaneo,Marco Zucchini,Franco Zucchini. Perceptive and Rehabilitative Muscle Recruitment Facilitation Secondary to the use of a Dynamic and Asymmetric Spine Brace in the treatment of Adolescent Idiopathic Scoliosis (AIS). . 2018 doi: 10.29328/journal.jnpr.1001021; 2: 054-079
-
Influence of an integrated rehabilitative treatment on the modification of body representation in patients affected by Unilateral Spatial NeglectMaurizio Falso*,Michela Delpero,Eleonora Cattaneo. Influence of an integrated rehabilitative treatment on the modification of body representation in patients affected by Unilateral Spatial Neglect. . 2018 doi: 10.29328/journal.jnpr.1001023; 2: 087-100
-
Functional Electrical Stimulation (FES): Clinical successes and failures to dateGad Alon*. Functional Electrical Stimulation (FES): Clinical successes and failures to date. . 2018 doi: 10.29328/journal.jnpr.1001022; 2: 080-086
-
TRIA-MF protocol as an innovative tool in the comprehensive treatment and outcome evaluation of lower limb amputees before and after prosthesis useMaurizio Falso*,Silvia Zani,Eleonora Cattaneo,Marco Zucchini,Franco Zucchini. TRIA-MF protocol as an innovative tool in the comprehensive treatment and outcome evaluation of lower limb amputees before and after prosthesis use. . 2019 doi: 10.29328/journal.jnpr.1001024; 3: 001-024
Recently Viewed
-
Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean sectionToon Wen Tang*,Phoon Wai Leng Jessie. Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean section. Clin J Obstet Gynecol. 2021: doi: 10.29328/journal.cjog.1001094; 4: 092-095
-
Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience ResearchAlex, Gideon S*,Olanrewaju Oluwaseun Oke,Joy Wilberforce Ekokojde,Tolulope Judah Gbayisomore,Martina C. Anene-Ogbe,Farounbi Glory,Joshua Ayodele Yusuf. Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience Research. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001102; 8: 106-114
-
Late discover of a traumatic cardiac injury: Case reportBenlafqih C,Bouhdadi H*,Bakkali A,Rhissassi J,Sayah R,Laaroussi M. Late discover of a traumatic cardiac injury: Case report. J Cardiol Cardiovasc Med. 2019: doi: 10.29328/journal.jccm.1001048; 4: 100-102
-
A two-phase sonographic study among women with infertility who first had normal sonographic findingsKalu Ochie*,Abraham John C. A two-phase sonographic study among women with infertility who first had normal sonographic findings. Clin J Obstet Gynecol. 2022: doi: 10.29328/journal.cjog.1001117; 5: 101-103
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001099; 8: 075-077
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."