Abstract
Research Article
How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?
Maurizio Falso*, Eleonora Cattaneo, Elisa Foglia, Marco Zucchini and Franco Zucchini
Published: 30 August, 2017 | Volume 1 - Issue 2 | Pages: 072-092
Background: Orthoses need to support physiotherapy as well as surgical treatment. Related to patient’s rehabilitative goals and pathological gait pattern, orthotists have to produce an orthoses that using an adjustable ankle joint system with preloaded disc springs can store the energy brought in by the body weight and produce a tuning effect on patient’s gait and sense of balance. The purpose of this study was to establish how a personalized proprioceptive individualized rehabilitative treatment could influence the functional response of different AFOs (Ankle Foot Orthoses) in a cohort of patients affected by neurological gait pattern.
Methods: Five patients affected by different neurological gait pattern and volunteered to participate to this study were recruited. The comparative spatio-temporal and functional effect on gait pattern of 3 types of AFOs was investigated under 4 study conditions: 1) without AFO or free-walk (FW); 2) wearing a Codivilla spring, 3) wearing a carbon unjointed AFO (“Toe-Off”); 4) wearing an innovative carbon-kevlar dynamic joint DAFO (DAFONS=Dynamic Ankle Foot Orthoses with Neuroswing). In line with our rehabilitative model, patients underwent to a weekly treatment session, 80 minutes duration per session, for 4 weeks. Evaluation was made before (time T3=time of recruitment) and after our individualized rehabilitative treatment course (time T4=1 month from T3) by using: a. G-Walk sensor (by BTS) spatio-temporal measures in different gait performances; b. clinical/functional outcome measures (Modified Ashworth Scale or MAS for the affected upper and lower limb; Medical Research Council or MRC; orthostatic stability evaluation by using the Berg Balance Scale or BBS).
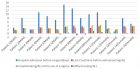
Findings: A comparative analysis of clinical and instrumental data, performed in the pre-defined four investigational conditions, showed:
√ a statistical insignificant change of MRC and MAS scales at time T4, with a significance trend outcome observed at the same time by using the Wilcoxon Signed Rank Test
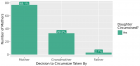
√ a statistical significant difference between test duration (sec) by using Toe-Off vs DAFONS and by using Codivilla spring vs Toe-Off
√ a statistical significant increase of the stride length on the left side (% cycle length) by using DAFONS compared to Toe-Off for patient P1, P3 and P5 with a parameter decrease by using DAFONS compared to Codivilla spring and Toe-Off use for patient P2
√ a statistical significant correlation between BBS trend and test duration (sec) by using Codivilla spring at time T3 and T4
√ a statistical significant correlation between the BBS trend and the double gait support duration on the right side (% cycle) with number of left step cycles by using DAFONS at time T3 and T4
√ in a comparative post-treatment visual gait analysis a modification of each patient’s static and dynamic postural assessment by using 3 different types of orthoses
Interpretation: In line with our study design we noted at the end of the proposed rehabilitative treatment an amelioration of gait quality with the use of DAFONS in all those patients (P1, P3 and P5) who showed a neurocognitive competence with a related functional grade of neurorehabilitative re-learning attitude of the physiological gait pattern and with a compromised perceptive control of gait and core stability. The proprioceptive profile of our rehabilitative program could promote the pro-adaptive and facilitation properties of a personalized gait control, induced by an innovative dynamic ankle foot orthoses with a modulable ankle joint system called Neuroswing. In the daily clinical practice, the personalized integration of a neurorehabilitative program and DAFONS can perform an individualized peripheral neuro-facilitation of gait cycle (peripheral perceptive facilitation), a neurorehabilitative re-learning process of physiological gait pattern (peripheral assisted neuroplasticity facilitation DAFONS induced) and an increase of patient’s motor abilities and quality of life in all daily performances.
Read Full Article HTML DOI: 10.29328/journal.jnpr.1001010 Cite this Article Read Full Article PDF
Keywords:
Ankle foot orthoses; Neurological gait pattern; Kinematic gait analysis; Proprioceptive rehabilitation
References
- Fritz S, Lusardi M. White paper: ‘‘walking speed: The sixth vital sign”. J Geriatr Phys Ther. 2009; 32: 46-49. Ref.: https://goo.gl/cDXLgC
- Muro-de-la-Herran A, Garcia-Zapirain B, Mendez-Zorrilla A. Gait Analysis Methods: An Overview of Wearable and Non-Wearable Systems, highlighting clinical applications. Sensors (Basel). 2014; 14: 3362-3394. Ref.: https://goo.gl/GAZYXR
- Guerra Padilla M, Molina Rueda F, Alguacil D. Effect of ankle-foot orthosis on postural control after stroke: a systematic review. Neurologia. 2014; 29: 423-432. Ref.: https://goo.gl/dMQcxY
- Bleyenheuft C, Deltombe T, Detrembleur C. Influence of ankle-foot orthoses on kinematic segmental covariation among stroke patients. Ann Phys Rehabil Med. 2013; 56: 3-13. Ref.: https://goo.gl/MHpKCY
- Novacheck TF, Trost JP, Sohrweide S. Examination of the child with cerebral palsy. Orthop Clin North Am. 2010; 41: 469-488. Ref.: https://goo.gl/w7DK8X
- Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle. J Bone Joint Surg Br. 2003; 85: 994-998. Ref.: https://goo.gl/aycwbc
- Thoumie P, Sautreuil P, Faucher M. Evaluation des propriétés physiologiques des orthèses de cheville. Revue de littérature. Ann Readapt Med Phys. 2004; 47: 225-232. Ref.: https://goo.gl/FfzQhc
- Richie DH Jr. Effects of foot orthoses on patients with chronic ankle instability. J Am Podiatr Med Assoc. 2007; 97: 19-30. Ref.: https://goo.gl/EAHM9t
- Brehm MA, Harlaar J, Schwartz M. Effect of ankle-foot orthoses on walking efficiency and gait in children with cerebral palsy. J Rehabil Med. 2008; 40: 529-534. Ref.: https://goo.gl/kgwhjM
- Abe H, Michimata A, Sugawara K, Sugaya N, et al. Improving gait stability in stroke hemiplegic patients with a plastic ankle-foot orthosis. Tohoku J Exp Med. 2009; 218: 193-199. Ref.: https://goo.gl/8kYGKP
- Fatone S, Gard SA, Malas BS. Effect of ankle-foot orthosis alignment and foot-plate length on the gait of adults with poststroke hemiplegia. Arch Phys Med Rehabil. 2009; 90: 810-818. Ref.: https://goo.gl/vVnWac
- Kerkum YL, Brehm MA, Buizer AI, van den Noort JC, Becher JG, et al. Defining the mechanical properties of a spring-hinged foot orthosis to assess its potential use in children with spastic cerebral palsy. J Appl Biomech. 2014; 30: 728-731. Ref.: https://goo.gl/qBgeQU
- Kim ES, Yoon YS, Sohn MK, Kwak SH, Choi JH, et al. Effect of pneumatic compressing powered orthosis in stroke patients preliminary study. Ann Rehabil Med. 2015; 39: 226-233. Ref.: https://goo.gl/7q77Re
- Mulroy SJ, Eberly VJ, Gronely JK, Weiss W, Newsam CJ. Effect of AFO design on walking after stroke: impact of ankle plantar flexion contracture. Prosthet Orthot Int. 2010; 34: 277-292. Ref.: https://goo.gl/23SH7V
- Slijper A, Danielsson A, Willen C. Ambulatory Function and Perception of Confidence in Persons with Stroke with a Custom-Made Hinged versus a Standard Ankle Foot Orthosis. Rehabil Res Pract. 2012; 2012: 206495. Ref.: https://goo.gl/iRaL1a
- Falso M, Cattaneo E, Zucchini M, Zucchini F. Influence of a custom-made dynamic ankle-foot orthosis with a reciprocant ankle joint system called Neuroswing on walking spatio-temporal parameters in patients affected by neurological gait schema: a comprehensive investigational study. JJ Physical Rehab Med. 2017; 3: 029.
Figures:

Figure 1

Figure 2

Figure 3

Figure 4

Figure 5

Figure 6

Figure 7

Figure 8

Figure 9

Figure 10

Figure 11

Figure 12

Figure 13

Figure 14

Figure 15

Figure 16

Figure 17

Figure 18

Figure 19
Similar Articles
-
How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?Maurizio Falso*, Eleonora Cattaneo,Elisa Foglia,Marco Zucchini,Franco Zucchini. How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?. . 2017 doi: 10.29328/journal.jnpr.1001010; 1: 072-092
Recently Viewed
-
Enhancing Physiotherapy Outcomes with Photobiomodulation: A Comprehensive ReviewNivaldo Antonio Parizotto*, Cleber Ferraresi. Enhancing Physiotherapy Outcomes with Photobiomodulation: A Comprehensive Review. J Nov Physiother Rehabil. 2024: doi: 10.29328/journal.jnpr.1001061; 8: 031-038
-
From Adversity to Agency: Storytelling as a Tool for Building Children’s ResilienceKate Markland*. From Adversity to Agency: Storytelling as a Tool for Building Children’s Resilience. J Nov Physiother Rehabil. 2024: doi: 10.29328/journal.jnpr.1001062; 8: 039-042
-
Physiotherapy Undergraduate Students’ Perception About Clinical Education; A Qualitative StudyPravakar Timalsina*,Bimika Khadgi. Physiotherapy Undergraduate Students’ Perception About Clinical Education; A Qualitative Study. J Nov Physiother Rehabil. 2024: doi: 10.29328/journal.jnpr.1001063; 8: 043-052
-
Management of Non-contact Injuries, Nonspecific Chronic Pain, and Prevention via Sensory Conflicts Detection: Vertical Heterophoria as a Landmark IndicatorEric Matheron*. Management of Non-contact Injuries, Nonspecific Chronic Pain, and Prevention via Sensory Conflicts Detection: Vertical Heterophoria as a Landmark Indicator. J Nov Physiother Rehabil. 2024: doi: 10.29328/journal.jnpr.1001057; 8: 005-013
-
The Impact of Telerehabilitation on Physical Therapy Services in Rural CommunitiesLi Ma*. The Impact of Telerehabilitation on Physical Therapy Services in Rural Communities. J Nov Physiother Rehabil. 2024: doi: 10.29328/journal.jnpr.1001058; 8: 014-016
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."